Abstract
Objective: To evaluate the effects of patellar taping on knee joint proprioception.
Design and Setting: In a research unit, 3 proprioceptive tests were performed. For each of the tests, a standardized patellar taping technique was applied in random order.
Subjects: Fifty-two healthy volunteers (27 women, 25 men; age, 23.2 ± 4.6 years; body mass index, 23.3 ± 3.7).
Measurements: We measured active angle reproduction, passive angle reproduction, and threshold to detection of passive movement on an isokinetic dynamometer.
Results: We found no significant differences between the tape and no-tape conditions in any of the 3 proprioceptive tests (P > .05). However, when the subjects' results for active angle reproduction and passive angle reproduction were graded as good (≤5°) and poor (>5°), taping was found to improve significantly those with poor proprioceptive ability (P < .01).
Conclusions: Subjects with good proprioception did not benefit from patellar taping. However, in those healthy subjects with poor proprioceptive ability as measured by active and passive ankle reproduction, patellar taping provided proprioceptive enhancement. Further studies are needed to investigate the effect of patellar taping on the proprioceptive status of patients with patellofemoral pain syndrome.
Keywords: proprioception testing, patellofemoral pain syndrome
Although patellar taping is readily used by physiotherapists in the treatment of patients with patellofemoral pain syndrome (PFPS), doubts still exist regarding the mechanism for its success. McConnell1 originally described patellar taping as part of a treatment program for PFPS and theorized that this technique could alter patellar position, enhance contraction of the vastus medialis oblique muscle, and hence, decrease pain. Studies thus far on patients with PFPS have been inconclusive regarding patellar taping enhancement of vastus medialis oblique contractions2 and taping realignment of patellar position.3 However, some studies have shown that patellar taping helps to decrease pain in patients with PFPS2 and in patellofemoral osteoarthritis,4 although the mechanism for this symptomatic improvement remains unknown. Some investigators have speculated that patellar taping may perform a role in providing a sense of mechanical stability to the patella.5,6
Proprioception is thought to play a more significant role than pain in preventing acute injury and in the evolution of chronic injury and degenerative joint disease.7 A recently updated paradigm described it as the acquisition of stimuli from peripheral mechanoreceptors in joints, muscles, and deep tissues (conscious) and the projection of these stimuli to the central nervous system to modify motor control (unconscious).8 Proprioceptive deficits have been found in anterior cruciate ligament–deficient knees,9,10 osteoarthritic knees,11 and knees with chronic effusions.12 Application of a knee brace or bandage improves the proprioceptive deficit. The only studies to date on PFPS and proprioceptive capacity have been contradictory. Prymka et al13 noted poorer proprioceptive capacity in patients with “chondropathia patellae” compared with healthy subjects, whereas Kramer et al14 could not find any proprioceptive deficits in patients with PFPS in either weight-bearing or non–weight-bearing tests. Interestingly, Prymka et al13 showed that an elastic knee bandage improved patients' proprioceptive status significantly. A proposed mechanism for this finding was that the bandage stimulated rapidly adapting superficial receptors in the skin during joint motion and increased pressure on the underlying muscles and joint capsule.15 Jerosch and Prymka16 speculated that patients who experienced patellofemoral dislocation disrupted a host of neuroproprioceptive structures in the medial retinaculum, capsule, bursae, and vastus medialis. This damage to the position sense receptors17 may account for the knee's poor proprioception status. Hypothetically, PFPS patients with more subtle forms of chronic patellar malalignment may also exhibit some dysfunction of the peripatellar plexus, detectable with proprioceptive testing. Therefore, just as the restoration to good proprioception status is widely accepted as a key component in the rehabilitation of other knee conditions, modulating proprioception in patients with PFPS may help promote normal knee function and accelerate the rehabilitation process.
Although a plethora of investigators have studied the role of elastic bandages and knee braces on proprioceptive enhancement in both symptomatic and asymptomatic groups,9–12 to date none have evaluated this phenomenon with patellar taping. Such a study may not only help to define the similarities between taping and bandaging but may also explain some of the mechanisms behind patellar taping. Our purpose was to determine the effect of application of patellar taping on the proprioceptive ability of the knee in a group of healthy subjects.
METHODS
Subjects
A convenience sample of 52 healthy volunteers (27 women, 25 men; mean age, 23.2 ± 4.6 years; body mass index, 23.3 ± 3.7) gave their informed consent. The study was performed in accordance with the Declaration of Helsinki. All subjects had healthy knees with no previous significant injury and were symptom free at the time of the study. Each subject served as his or her own control, with the no-tape condition being the internal control.
Materials
Testing was performed on the Biodex 2 Isokinetic Dynamometer (Biodex Corp, Shirley, NY) using this system's electrogoniometer, which is sensitive to 1° increments. This was calibrated before the sessions in accordance with the manufacturer's instructions. Data were processed using the Biodex Advantage software (version 4.5). Visual cues were eliminated by blindfolds. The tape was a 10-cm-wide strip of Hypafix (Smith & Nephew, Hull, UK). A sphygmomanometer cuff was supplied to provide equal sensory input to the lower limb of each patient from the dynamometer's tibial pad (SP Services, Telford, UK).
Procedures
Each subject was in shorts, barefoot, and blindfolded for the test and sat on the testing seat with hip flexion at 90° (Figure 1). The right limb was chosen for each subject to facilitate the testing setup and because previous studies had shown no proprioceptive differences between dominant and nondominant limbs.18 The tibial pad was secured to the shank of the leg 3 cm superior to the lateral malleolus. The sphygmomanometer cuff was wrapped around the tibia under the tibial pad. It was inflated to 40 mm Hg and was checked constantly to ensure equal pressure throughout the study. To avoid any learning effect, both the order of tests and the order of conditions were randomly allocated for each subject. Each of the 6 testing conditions (2 tape conditions and 3 tests) was completely randomized. After each test, the subject was instructed to leave the seat and walk around the room to reduce any possibility of proprioceptive carryover to the next test.
Figure 1.
Patient setup on the Biodex dynamometer.
Measurement of Proprioception
Proprioception can be appreciated and measured consciously by sensations of movement and joint sense. To detect both these aspects and, therefore, test proprioception, methods were adopted from previous studies. The methods chosen were passive angle reproduction (PAR),15 active angle reproduction (AAR),19 and the threshold for detection of passive movement (TDPM).10
Passive Angle Reproduction
Starting at 90° of knee flexion, the lever arm passively extended the test limb, without resistance to the movement, to the target angle of 45°. This angle is in the working range of the knee during daily weight-bearing activities.11 Passive movement was set at an angular velocity of 2°·s−1 to limit reflexive muscle contractions. Subjects were instructed not to voluntarily contract their muscles, and we assumed that no muscular contraction was present. The limb was maintained at the target angle for 10 seconds to enable the subject to remember the position. After the limb was passively returned to 90°, there was a 5-second pause, and the cycle was performed again. This time the subject activated a handheld stop button when he or she felt the target angle had been achieved. Once the button had been activated, patients were not permitted to correct the angle. The angle was identified from the onscreen goniometer. Three readings were taken, and the absolute difference between the perceived angle and the target angle was calculated for each reading.
Active Angle Reproduction
In the same seated conditions, the subject actively moved the limb to the target angle of 45° of flexion. The leg was held there for 10 seconds, so the subject could memorize the position, and then returned to 90° of knee flexion. After a pause of 5 seconds, the subject moved the lower limb by active contraction at an angular velocity approximating 2°·s−1 and stopped when he or she thought the target angle had been reached. Subjects were not permitted to correct the angle. The absolute difference between the perceived angle and the target angle was calculated for each trial.
Threshold to Detection of Passive Movement
In the same seated conditions, the dynamometer was set at a knee angle of 90° of flexion and the passive angular velocity at 30°·s−1. The subject was asked to press the handheld stop button when he or she felt a sensation of movement or a change in the starting knee position. The onset of movement was delayed randomly by the operator. Auditory cues were masked by a set of headphones. Three consecutive trials were performed, with the movement in degrees from the starting position noted.
Patellar Taping
Patellar taping was applied by one of the 2 principal investigators (M.J.C. or J.S.). Practice sessions were performed to ensure a similar procedure for taping and testing. With the subject supine with a relaxed, extended knee, one strip of tape was applied without tension across the center of the patella. The center of the tape was as near as possible to the center of the patella, with its medial and lateral edges aligned with the medial and lateral joint lines. The tape was not pulled in either the medial or lateral direction because the subjects were asymptomatic and had no evidence of patellar malalignment. Care was taken with the length of tape because anthropometric differences among subjects may have meant some smaller patients received proportionally greater amounts of tape than others. Thus, the length of tape was calculated to be 50% of the total circumference of the subject's knee as measured with a tape measure.
Data Analysis
Statistical analysis was performed using the Statistical Package for the Social Sciences for Windows (version 7.5, SPSS Inc, Chicago, IL). The data were tested using the Kolmogorov-Smirnov test and found to be not normally distributed (P > .05); therefore, separate nonparametric Wilcoxon signed rank tests were used for each measure of proprioception tested. The level of probability was set at P < .05. Each subject had 3 readings on each of the 3 tests (PAR, AAR, and TDPM) and the 2 conditions (tape and no tape). For PAR and AAR, the absolute differences between the target angle and the actual angle recorded were used. For TDPM, differences between the start and stop angles for all consecutive trials were calculated. Three readings were taken for each subject in each condition and used to calculate the difference between the actual angle and the target angle.20 The actual angle may have been greater or less than the target angle, but because the difference between them was the more relevant figure for analysis, the positive or negative direction was disregarded.15
RESULTS
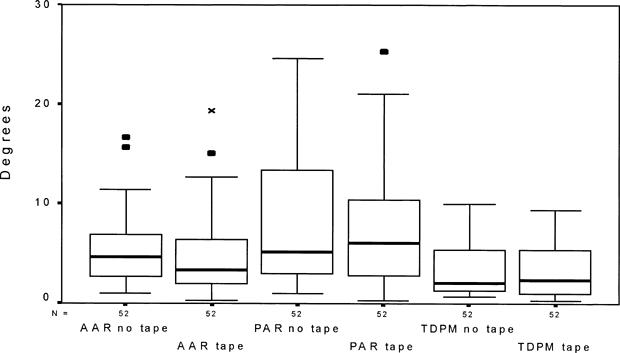
Nonparametric test results for all methods of testing for proprioception are displayed in Table 1. The results of the Wilcoxon signed rank tests revealed no significant differences between the tape and no-tape conditions for the 3 tests (AAR, P = .173; PAR, P = .358; TDPM, P = .881). The medians and interquartile ranges of the degrees from the target angle for all 52 subjects in all conditions are shown in Figure 2. Parametric results are also presented in Table 2 and Figure 3.
Table 1. Degrees From the Target Angle*
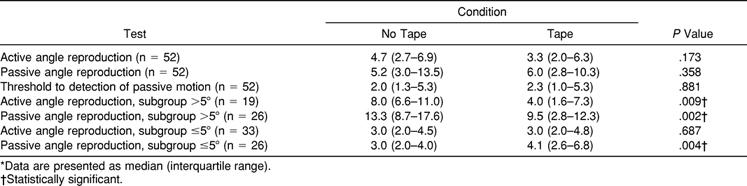
Figure 2.
Deviation from the target angle for all tests and both conditions. 0 indicates target angle; x, outlying values; ▪, extreme values; AAR, active angle reproduction; PAR, passive angle reproduction; and TDPM, threshold to detection of passive motion.
Table 2. Degrees From the Target Angle*
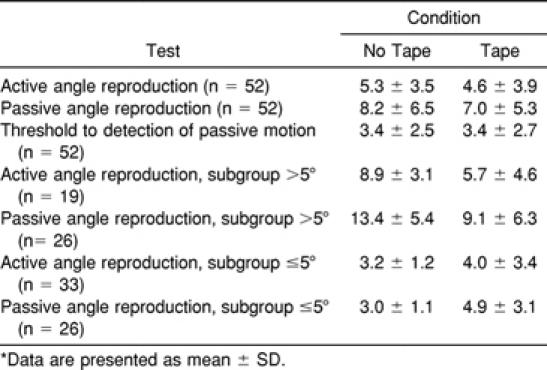
Figure 3.
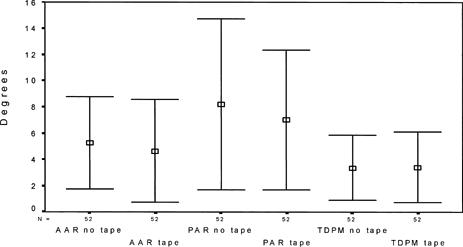
Deviation from the target angle for all tests and both conditions. 0 indicates target angle; AAR, active angle reproduction; PAR, passive angle reproduction; and TDPM, threshold to detection of passive motion.
Previous researchers15 had further analyzed their data by subdividing their samples into good (≤5°) and poor (>5°) proprioceptive groups. These were simply categoric names allocated according to the accuracy score and not a specific diagnosis of the subjects' status. We also conducted this analysis on the present data to ascertain if such a division existed in our group of healthy subjects and if taping would similarly help those who displayed poor proprioception. For PAR, accuracy from the target angle was more than 5° for 26 subjects and 5° or less for 26 subjects. Wilcoxon signed rank tests revealed that taping significantly improved the accuracy of the poor group (P = .004) (Figure 4) and actually worsened that of the good group (P = .007). The same analysis was performed on the AAR test, with 19 subjects in the poor group and 33 in the good group. Once again, taping significantly improved the poor group's accuracy (P = .009) (Figure 5) but had no effect on the good group (P = .687).
Figure 4.
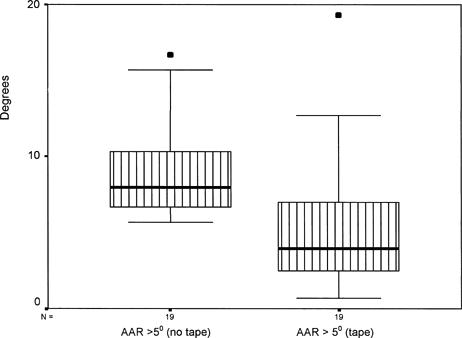
Improvement in accuracy after tape for active angle reproduction test in subgroup with more than 5° difference from target angle. 0 indicates target angle; ▪, extreme values; and AAR, active angle reproduction.
Figure 5.
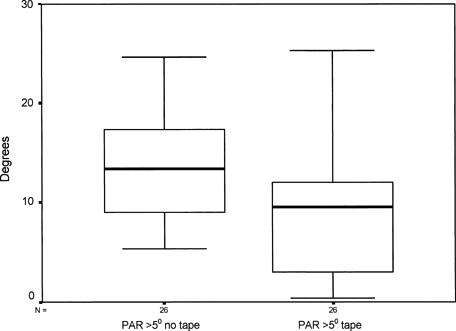
Improvement in accuracy after tape for passive ankle reproduction test in subgroup with more than 5° difference from target angle. 0 indicates target angle; PAR, passive angle reproduction.
DISCUSSION
We hypothesized that patellar taping would enhance proprioception in healthy subjects using 3 common measures of proprioception. Taping did improve the proprioceptive status of those categorized as having poor proprioception but not those with good status as measured by AAR and PAR. In previous studies involving the application of various types of knee braces and bandages, knee joint proprioception has improved on both static21 and dynamic18 proprioception tests. This has been attributed more to a sensory function than a purely mechanical one. Lephart et al22 speculated that because proprioception is mediated by afferent input from articular, muscular, and cutaneous structures, the improvement in knee joint proprioception was due to augmented afferent input via enhancement of cutaneous stimulation from a neoprene sleeve. Barrett et al11 used a similar explanation for improvement in osteoarthritic knees with an elastic bandage. A comparable knee bandage has been previously investigated in patients with patellar dislocation and proven proprioceptive deficit.19 The proprioceptive enhancement demonstrated in that study indicated that such deficits could be rectified by stimulating skin during motion and by pressure on underlying muscles and the joint capsule. This was the basis for our investigation into patellar taping, and we speculate that similar mechanisms accounted for our results in poor-proprioception subjects on the AAR and PAR tests.
Our initial results indicated that taping did not enhance the ability of healthy subjects to reproduce a target angle either actively or passively or to detect passive motion. However, as has been found in a previous study,15 it seems that not all healthy subjects have good proprioception, and their ability could be classified as poor or good depending on their accuracy in reproducing the target angle. Improvement in proprioception did not occur to statistical significance when the whole group was analyzed, probably because the data from the good and poor groups canceled out.
We hypothesize that subjects with poor proprioceptive ability (ie, >5° accuracy from the target angle) may have received improved afferent feedback via cutaneous receptor stimulation from the patellar tape, thereby improving joint reposition accuracy. This, however, was not the case in subjects classified as having good proprioception. Another explanation might be that those with good proprioception were good enough not to need any influence from external aids such as taping; the poor group, on the other hand, was more amenable to any external help given to them by taping. Birmingham et al21 also noted that the poorer the inherent proprioceptive ability, the greater the improvement after application of an external device.
Active Angle Reproduction
The improvement in accuracy for the whole group in our study was not statistically significant, although the value of 1.4° was very similar to the findings of Birmingham et al21 on the open kinetic chain active reproduction test (1.2°) using a neoprene sleeve, which were statistically significant. The difference in statistical significance is probably due to the use of parametric statistical analysis by Birmingham et al,21 with greater dispersal about the means and smaller SDs. Furthermore, they averaged their absolute differences in 5 attempts over 5 different target angles. In contrast, we used nonparametric analysis and had large interquartile ranges, reflecting overlapping medians. Categorizing the present data into poor and good subjects15 revealed that patellar taping significantly improved the proprioceptive ability of those with an AAR score of more than 5°. In contrast, patellar taping had no effect at all on those whose AAR score was 5° or less. Reasons for this are discussed in the context of PAR testing.
Passive Angle Reproduction
The difference from the target angle in our study between tape and no-tape conditions was 0.8°. This figure is similar to that of Perlau et al,15 who noted a difference of 1° using an elastic knee sleeve at 5°·s−1; the sleeve markedly improved the PAR results of subjects with poor proprioceptive ability (>5° from a target angle), but there was no demonstrable effect on their subjects with good proprioception (≤5°). They did not put their data to formal statistical analysis. With the same 5° angle criterion to separate the data, our formal statistical analysis concurs with the descriptive analysis of Perlau et al15: statistically significant improvements with the tape for those in the poor group. Interestingly, those with good proprioception were actually made significantly worse by patellar taping (P = .004), although the difference of 1.1° is far smaller than any of the other taping effects. Perlau et al15 speculated that afferent stimuli enhanced by external appliances, although helpful to some subjects whose proprioceptive status for PAR is classified as poor, can be unhelpful or even confusing to subjects with better proprioceptive status. Our results seem to enforce this theory in both the good PAR (worse) and the good AAR (no help).
Threshold to Detecting Passive Motion
One possible reason for this test's inability to show any differences may have lain more with the insensitivity of the Biodex dynamometer than the ineffectiveness of the tape. The onscreen goniometer was only sensitive to 1° increments, compared with other studies that used more sensitive devices or electrogoniometers. This device limitation means that proprioceptive differences of less than 1° would not be detected. During the feasibility phase of this study, we used a testing angular velocity of 2°·s−1, which was within the usual range of angular velocities of 0.2°·s−1 to 5°·s−1.23 This angular velocity range has been recommended to minimize the contribution of musculotendinous mechanoreceptors in providing the central nervous system with information regarding limb position and movement. At 2°·s−1, we noted that subjects were able to detect motion but registered very little variation on the onscreen goniometer. An increase in angular velocity to 30°·s−1 allowed more variation among subjects' scores, but this was far in excess of the recommended angular velocity for this type of test, and its reliability and validity have not been addressed. We found a very small worsening of 0.3°, similar to that of Beynnon et al,20 who found a difference of 0.28°. Although this initially may be considered of doubtful clinical significance, it is possible that in real life, with the limb moving at great velocity and subjected to high forces, this small value takes on greater clinical significance than first thought. We recommend that careful consideration be given to using a commercial dynamometer, such as the Biodex, for the TDPM test. A purpose-built device20,23 or electrogoniometry14,18 may be more sensitive methods for detecting threshold to passive motion.
The taping was applied by senior outpatient clinicians who run regular courses on patellar taping for graduate physiotherapists. To ensure that their technique was consistent, a simple method was used, with the tape applied directly over the patella of the extended, relaxed knee. Although more complex variations of patellar taping have been advocated, this study was performed on asymptomatic subjects who had no abnormality to correct. Furthermore, the amount of skin covered was considered more important than the number of tape layers over the same area of skin. Our findings also suggest that care should be taken when using a group of healthy subjects to establish normative data. In the PAR test, exactly 50% of the subjects were classified as having poor proprioception according to the criteria of Perlau et al.15 In the AAR test, 37% of the subjects were classified as poor using the same criteria.
Limitations of the Study
Although the sample size of 52 is considerably larger than any other study we have cited except for Perlau et al15 (N = 54) and Birmingham et al21 (N = 59), and our mean values are comparable with those of many other studies, our subjects exhibited larger variance around the mean, resulting in the study's low power. For example, for the tape and no-tape conditions (N = 52), the AAR test had a power of 0.12; the PAR test had a power of 0.15 (P < .05). Put another way, with the mean differences and the variance exhibited by our patients, we would have needed 664 patients to detect a meaningful difference in the AAR test and 461 for the PAR. We recommend that future investigators consider this aspect carefully by performing proper calculations for the sample size.
The power calculation at P < .05 for the poor AAR group (n = 19) was 0.57 and for the poor PAR group (n = 26) was 0.69. It was not possible to determine sample power from the data reported in Perlau et al,15 but we calculated that although Birmingham et al21 had excellent power (0.99) for AAR, power for PAR was only 0.47 (P < .05).
The TDPM test was conducted at an angular velocity in excess of that recommended by other researchers in this field.18 We accept this limitation and acknowledge that the results for this particular test should be interpreted with caution. The sensitivity of the Biodex goniometer could also be construed as a limitation, because the 1° increments may be insensitive to more subtle differences among subjects or between taping conditions. Some clinicians may argue that the taping technique was not specific enough to reflect different clinical situations or abnormalities of PFPS. Our methods were designed to facilitate technique between the authors and control for variable skin coverage. Furthermore, the subjects had neither PFPS nor abnormalities of the patella.
CLINICAL IMPLICATIONS
The clinical implications of these findings are that poor proprioceptive status can be enhanced by a simple patellar taping technique. Clinicians using patellar taping need not apply a complex technique to achieve an improvement in proprioception. Healthy subjects with poor proprioception may be at enhanced risk for PFPS. As with other knee conditions, applying an external appliance such as tape may reduce the risk of injury by enhancing proprioception. Proprioception in PFPS is underresearched, and further study is necessary to investigate this phenomenon and also the effect of patellar taping on the proprioceptive status of patients with PFPS.
CONCLUSION
Knee proprioception measured by AAR, PAR, and TDPM did not change significantly when healthy subjects received patellar taping. The improvement achieved with patellar taping reached statistical significance, however, when applied to those subjects with poor knee joint proprioception (>5° accuracy) in the AAR and PAR tests.
Acknowledgments
ACKNOWLEDGMENTS
We are grateful for the cooperation of the Schools of Physiotherapy at the Universities of Manchester and Bradford, UK, to Bradford Hospital NHS Trust, and to Dr Julie Winstanley for statistical analysis.
REFERENCES
- McConnell J. The management of chondromalacia patellae: a long term solution. Aust J Physiother. 1986;32:215–223. doi: 10.1016/S0004-9514(14)60654-1. [DOI] [PubMed] [Google Scholar]
- Cerny K. Vastus medialis oblique/vastus lateralis muscle activity ratios for selected exercises in persons with and without patellofemoral pain syndrome. Phys Ther. 1995;75:672–683. doi: 10.1093/ptj/75.8.672. [DOI] [PubMed] [Google Scholar]
- Crossley K, Cowan S M, Bennell K L, McConnell J. Patellar taping: is clinical success supported by scientific evidence? Man Ther. 2000;5:142–150. doi: 10.1054/math.2000.0354. [DOI] [PubMed] [Google Scholar]
- Cushnaghan J, McCarthy C, Dieppe P. Taping the patella medially: a new treatment for osteoarthritis of the knee? BMJ. 1995;308:753–755. doi: 10.1136/bmj.308.6931.753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mungovan S F, Henley E C, Renton A L, Turner G R. The effect of patellofemoral taping on EMG activity and torques produced about the knee during standing up from a seated position. Proceedings of the 11th World Confederation of Physical Therapists October 1991; London, England: 1991. pp. 1304–1306.
- Werner S, Knutsson E, Eriksson E. Effect of taping the patella on concentric and eccentric torque and EMG of knee extensor and flexor muscles in patients with patellofemoral pain syndrome. Knee Surg Sports Traumatol Arthrosc. 1993;1:169–177. doi: 10.1007/BF01560200. [DOI] [PubMed] [Google Scholar]
- Lephart S M. The role of proprioception in the treatment of sports injuries. Sports Exerc Inj. 1995;1:96–102. [Google Scholar]
- Lephart S M, Fu F H, editors. Proprioception and Neuromuscular Control in Joint Stability. Human Kinetics; Champaign, IL: 2000. [Google Scholar]
- Barrack R L, Lund P J, Skinner H B. Knee joint proprioception revisited. J Sport Rehabil. 1994;3:18–42. [Google Scholar]
- Corrigan J P, Cashman W F, Brady M P. Proprioception in the cruciate deficient knee. J Bone Joint Surg Br. 1992;74:247–250. doi: 10.1302/0301-620X.74B2.1544962. [DOI] [PubMed] [Google Scholar]
- Barrett D S, Cobb A G, Bentley G. Joint proprioception in the normal, osteoarthritic and replaced knee. J Bone Joint Surg Br. 1991;73:53–56. doi: 10.1302/0301-620X.73B1.1991775. [DOI] [PubMed] [Google Scholar]
- Guido J, Jr, Voight M L, Blackburn T B, Kidder J D, Nord S. The effects of chronic effusion on knee joint proprioception: a case study. J Orthop Sports Phys Ther. 1997;25:208–212. doi: 10.2519/jospt.1997.25.3.208. [DOI] [PubMed] [Google Scholar]
- Prymka M, Schmidt K, Jerosch J. Proprioception in patients suffering from chondropathia patellae. Int J Sports Med. 1998;19:S60. [Google Scholar]
- Kramer J, Handfield T, Keifer G, Forwell L, Birmingham T B. Comparisons of weight-bearing and non-weight-bearing tests of knee proprioception performed by patients with patello-femoral pain syndrome and asymptomatic individuals. Clin J Sport Med. 1997;7:113–118. doi: 10.1097/00042752-199704000-00007. [DOI] [PubMed] [Google Scholar]
- Perlau R, Frank C, Fick G. The effect of elastic bandages on human knee proprioception on the uninjured population. Am J Sports Med. 1995;23:251–255. doi: 10.1177/036354659502300221. [DOI] [PubMed] [Google Scholar]
- Jerosch J, Prymka M. Knee joint proprioception in patients with posttraumatic recurrent patellar dislocation. Knee Surg Sports Traumatol Arthrosc. 1996;4:14–18. doi: 10.1007/BF01565991. [DOI] [PubMed] [Google Scholar]
- Wilson A S, Lee H B. Hypothesis relevant to defective position sense in a damaged knee. J Neurol Neurosurg Psychiatry. 1986;49:1462–1463. doi: 10.1136/jnnp.49.12.1462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jerosch J, Prymka M. Knee joint proprioception in normal volunteers and patients with anterior cruciate ligament tears taking special account of the effect of a knee bandage. Arch Orthop Trauma Surg. 1996;115:162–166. doi: 10.1007/BF00434546. [DOI] [PubMed] [Google Scholar]
- Friden T, Roberts D, Zatterstrom R, Lindstrand A, Moritz U. Proprioception of the nearly extended knee: measurements of position and movement in healthy individuals and in symptomatic anterior cruciate ligament injured patients. Knee Surg Sports Traumatol Arthrosc. 1996;4:217–224. doi: 10.1007/BF01567966. [DOI] [PubMed] [Google Scholar]
- Beynnon B D, Ryder S H, Konradsen L, Johnson R J, Johnson K, Renström P A. The effect of anterior cruciate ligament trauma and bracing on knee proprioception. Am J Sports Med. 1999;27:150–155. doi: 10.1177/03635465990270020601. [DOI] [PubMed] [Google Scholar]
- Birmingham T B, Kramer J F, Inglis J T, et al. Effect of a neoprene sleeve on knee joint position sense during sitting open kinetic chain and supine closed kinetic chain tests. Am J Sports Med. 1998;26:562–566. doi: 10.1177/03635465980260041601. [DOI] [PubMed] [Google Scholar]
- Lephart S M, Kocher M S, Fu F H, Borsa P A, Harner C D. Proprioception characteristics following ACL reconstruction. J Sport Rehabil. 1992;1:188–196. [Google Scholar]
- Lephart S M, Pincivero D M, Rozzi S L. Proprioception of the ankle and knee. Sports Med. 1998;25:149–155. doi: 10.2165/00007256-199825030-00002. [DOI] [PubMed] [Google Scholar]


