Abstract
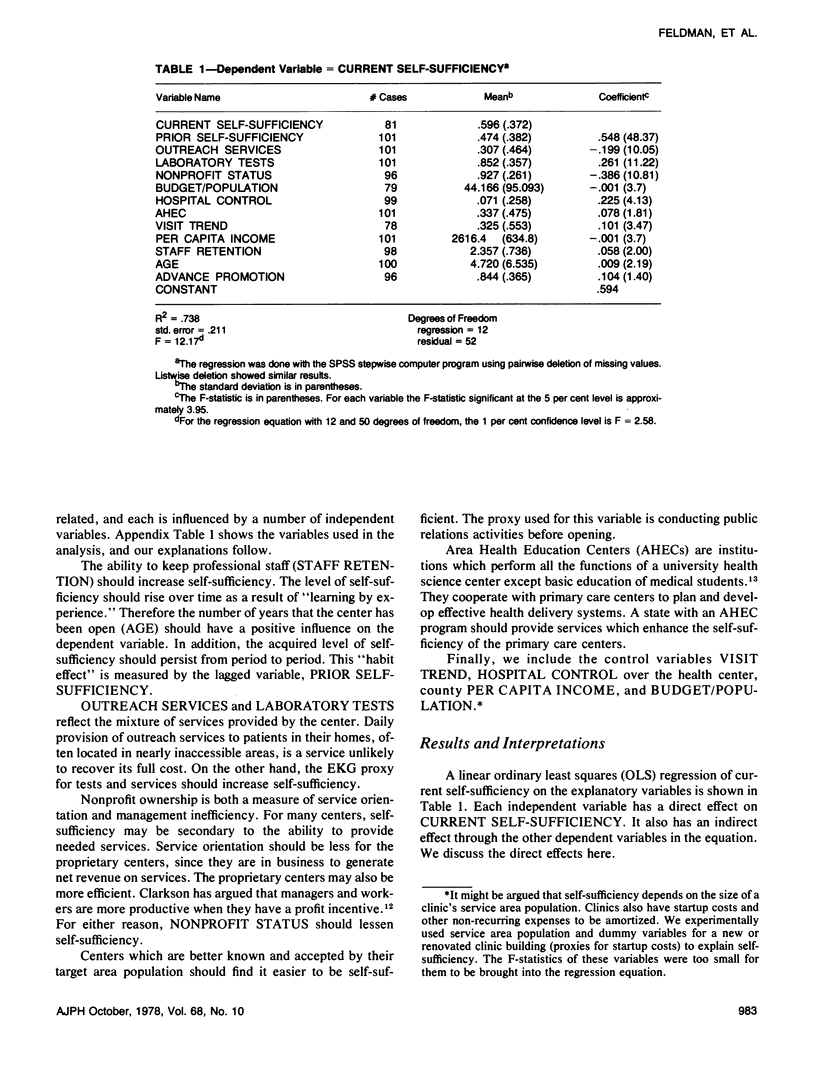
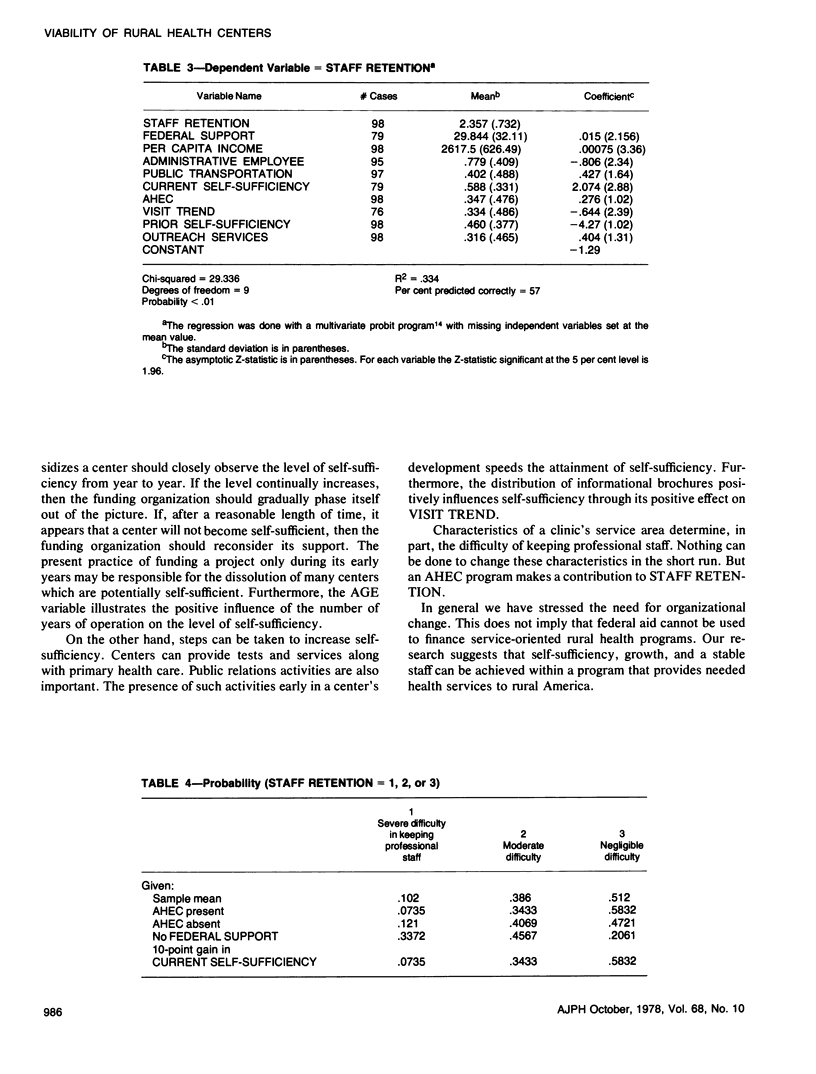
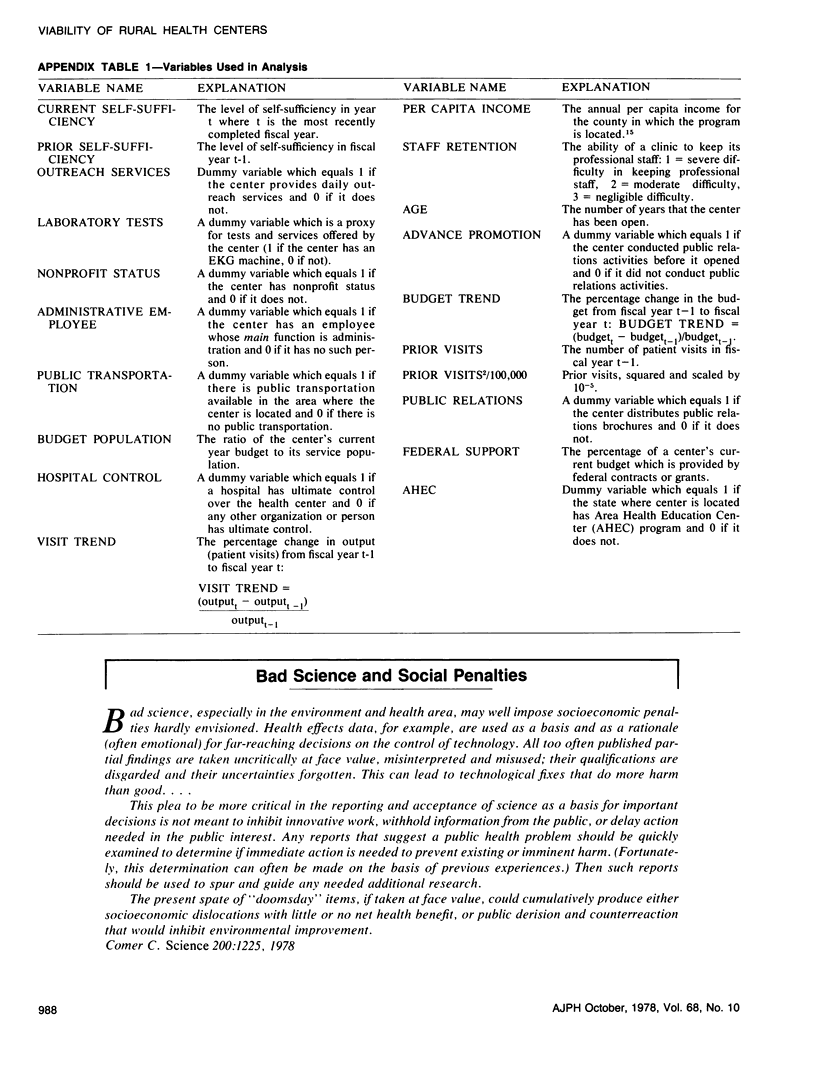
Primary health care centers have been proposed to meet the health care needs of rural America. Some centers become financially "self-sufficient", receiving their entire budgets from direct patient or third-party payments; others shut down when external funding is withdrawn. An explanation for this difference is important, because funding agencies may not wish to subsidize centers whose financial futures appear bleak. This study identifies the correlates of financial self-sufficiency. A survey conducted in late 1976 or 164 rural clinics provided 101 usable responses. Multiple regression analysis of the data shows that the longer a center has been in operation, the more self-sufficient it will become. Hospital control of the center and provision of laboratory tests increase self-sufficiency; outreach services and nonprofit status reduce it. Two variables related to financial self-sufficiency are separately examined. Clinics with a faster growth rate of patient visits are more self-sufficient, and smaller clinics tend to grow faster. More self-sufficient clinics experience less difficulty in keeping professional staff. The presence of a state Area Health Education Center (AHEC) program also eases the problem of staff retention.
Full text
PDF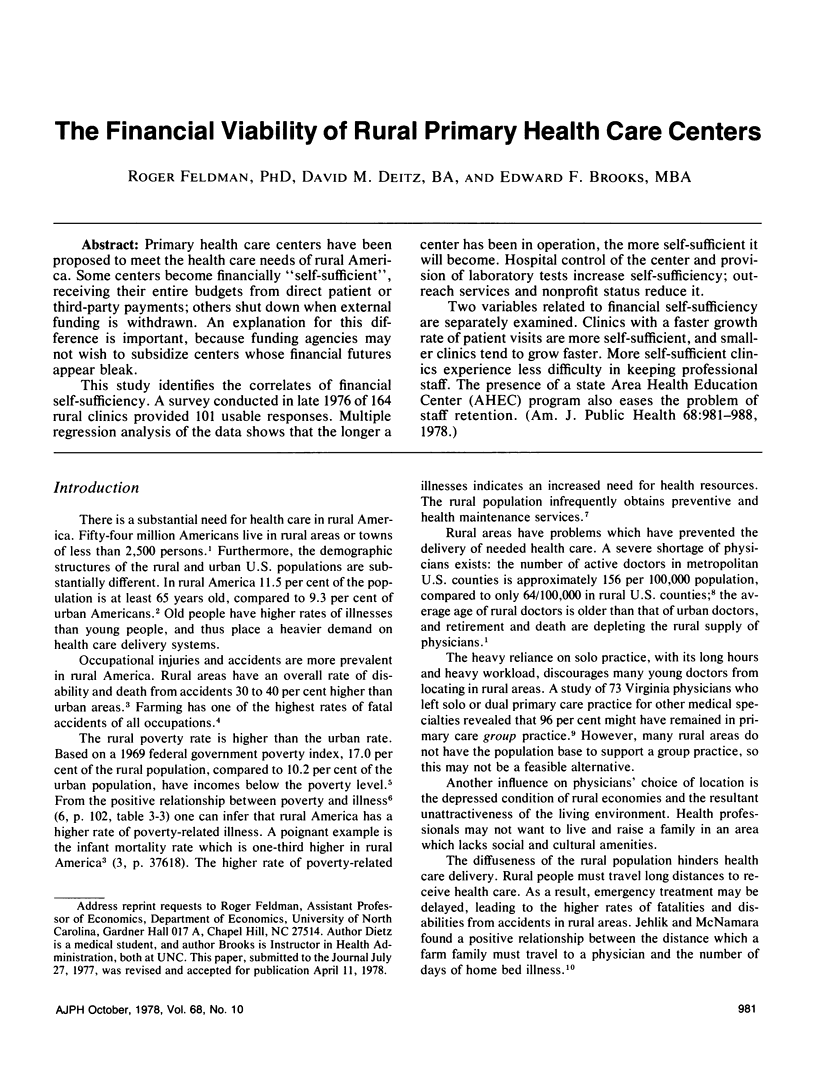

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Crawford R. L., McCormack R. C. Reasons physicians leave primary practice. J Med Educ. 1971 Apr;46(4):263–268. doi: 10.1097/00001888-197104000-00001. [DOI] [PubMed] [Google Scholar]
- Guillozet N. Rural medicine. Making it now, and the problems ahead. Calif Med. 1973 Apr;118(4):91–93. [PMC free article] [PubMed] [Google Scholar]
- Reiheld R. E. Statement of the American Medical Association before the Subcommittee on Rural Development. Committee on Agriculture U.S. House of Representatives. Ohio State Med J. 1975 Jan;71(1):44–46. [PubMed] [Google Scholar]


