Abstract
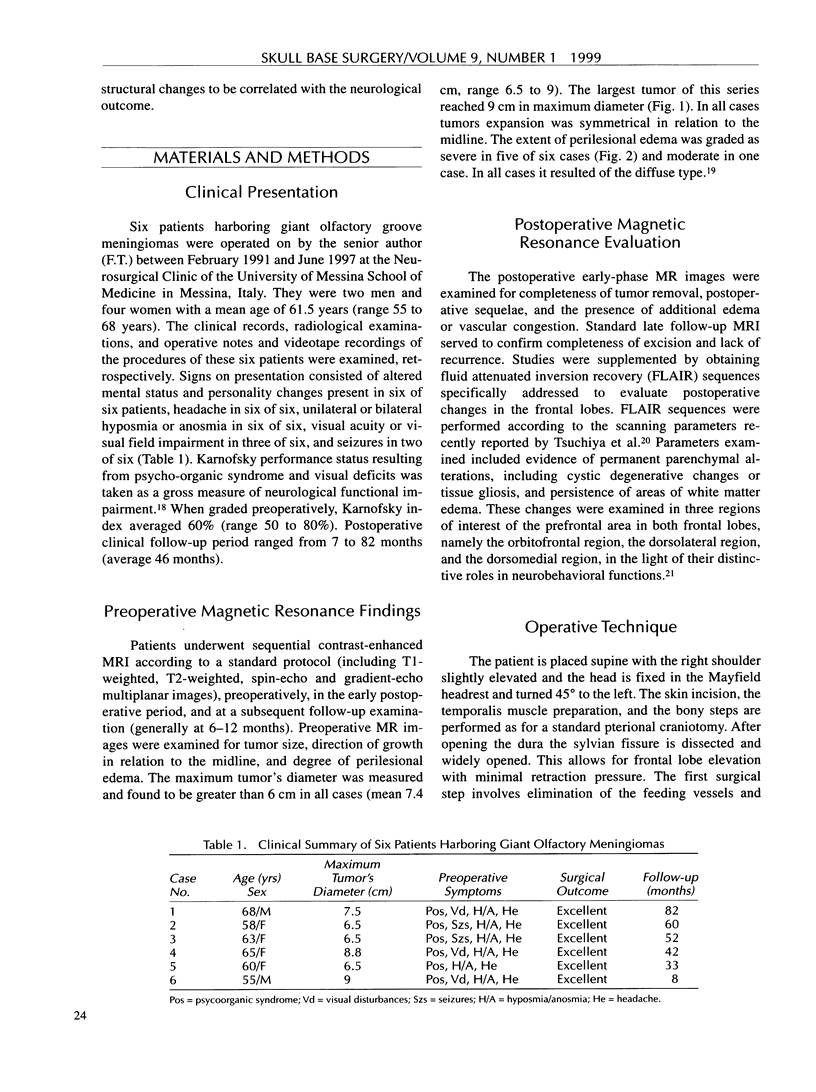
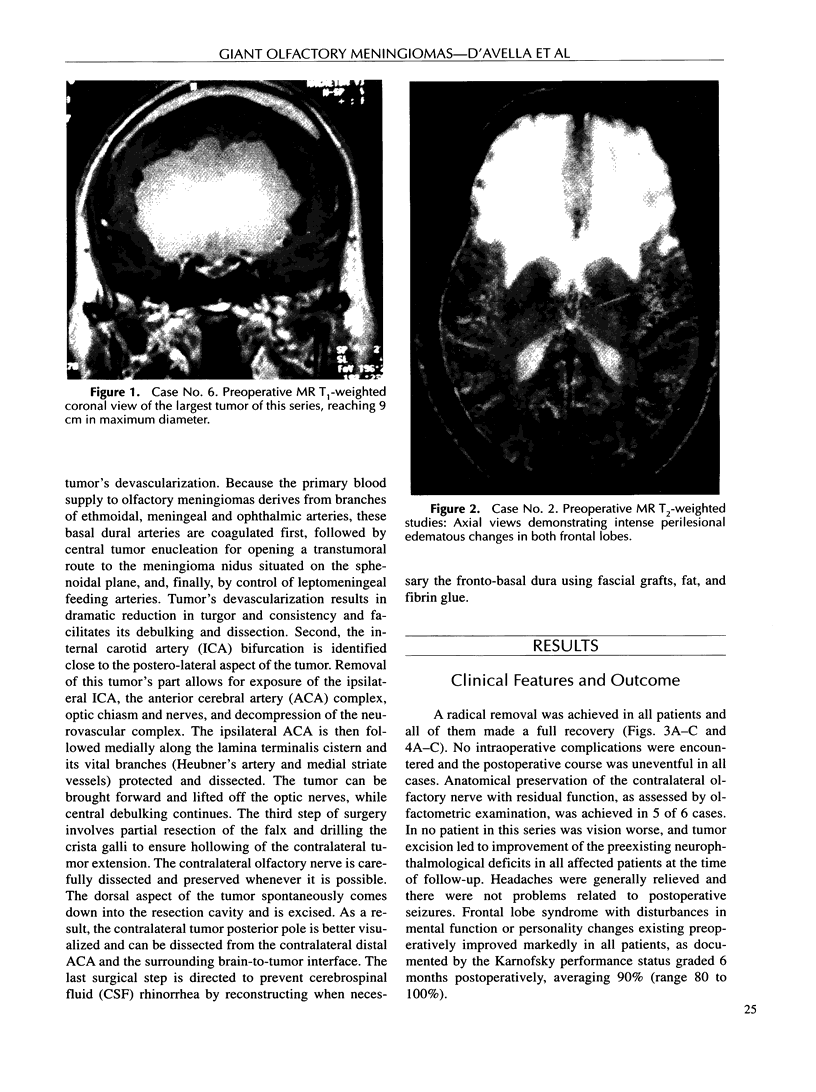
Olfactory groove meningiomas may attain surprisingly large size. The subfrontal approach is currently the route preferred by most neurosurgeons for their excision. The pterional-transsylvian route represents an alternate exposure for microsurgery of frontobasal tumors. Although this approach has been already described for olfactory meningiomas, tumors of giant size were not specifically addressed in the literature. We report the application of the pterional-transsylvian approach in six patients with giant olfactory meningiomas. This series is unique because it includes only patients with tumors exceeding 6 cm in diameter with bilateral symmetrical development. A radical removal was achieved in all patients and all of them made a full recovery. To investigate the relevance of the pterional-transsylvian approach for minimizing surgical morbidity, a magnetic resonance imaging protocol was designed to characterize even subtle postoperative frontal lobe structural changes. These changes, limited to the frontal lobe ipsilateral to exposure and localized in specific anatomical domains of the prefrontal area, included cystic degenerative alterations, parenchymal gliosis, and associated persistent white matter edema. Results from the present series strengthen the usefulness of the pterional-transsylvian approach as a safe surgical route for lesions affecting the anterior skull base, even with huge bilateral symmetrical expansion, such as giant olfactory meningiomas.
Full text
PDF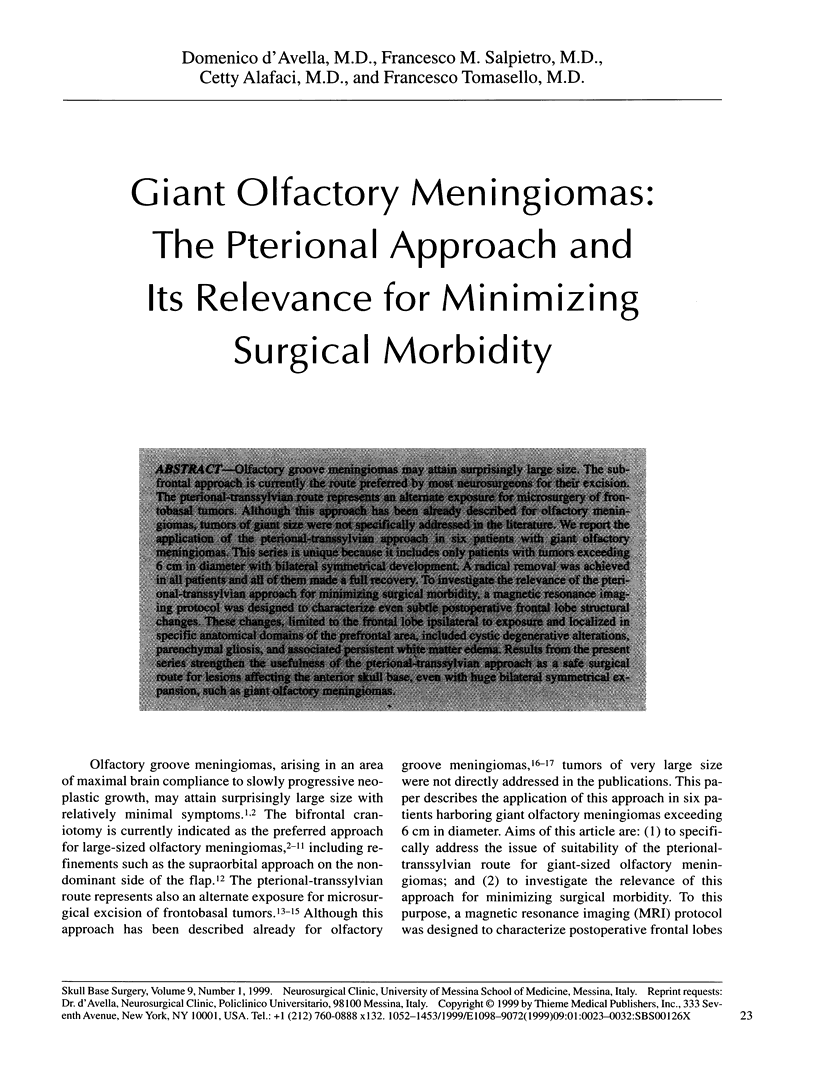


Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Alaywan M., Sindou M. Facteurs pronostiques dans la chirurgie des méningiomes intracrâniens. Rôle de la taille de la tumeur et de sa vascularisation artérielle d'origine pie-mérienne. Etude sur 150 cas. Neurochirurgie. 1993;39(6):337–347. [PubMed] [Google Scholar]
- Babu R., Barton A., Kasoff S. S. Resection of olfactory groove meningiomas: technical note revisited. Surg Neurol. 1995 Dec;44(6):567–572. doi: 10.1016/0090-3019(95)00196-4. [DOI] [PubMed] [Google Scholar]
- Bakay L. Olfactory meningiomas. The missed diagnosis. JAMA. 1984 Jan 6;251(1):53–55. [PubMed] [Google Scholar]
- De Coene B., Hajnal J. V., Gatehouse P., Longmore D. B., White S. J., Oatridge A., Pennock J. M., Young I. R., Bydder G. M. MR of the brain using fluid-attenuated inversion recovery (FLAIR) pulse sequences. AJNR Am J Neuroradiol. 1992 Nov-Dec;13(6):1555–1564. [PMC free article] [PubMed] [Google Scholar]
- Hassler W., Zentner J. Pterional approach for surgical treatment of olfactory groove meningiomas. Neurosurgery. 1989 Dec;25(6):942–947. [PubMed] [Google Scholar]
- Hassler W., Zentner J. Pterional approach for surgical treatment of olfactory groove meningiomas. Neurosurgery. 1989 Dec;25(6):942–947. [PubMed] [Google Scholar]
- KARNOFSKY D. A., BURCHENAL J. H., ARMISTEAD G. C., Jr, SOUTHAM C. M., BERNSTEIN J. L., CRAVER L. F., RHOADS C. P. Triethylene melamine in the treatment of neoplastic disease; a compound with nitrogen-mustardlike activity suitable for oral and intravenous use. AMA Arch Intern Med. 1951 Apr;87(4):477–516. doi: 10.1001/archinte.1951.03810040002001. [DOI] [PubMed] [Google Scholar]
- Kadis G. N., Mount L. A., Ganti S. R. The importance of early diagnosis and treatment of the meningiomas of the planum sphenoidale and tuberculum sellae: a retrospective study of 105 cases. Surg Neurol. 1979 Nov;12(5):367–371. [PubMed] [Google Scholar]
- Mayfrank L., Gilsbach J. M. Interhemispheric approach for microsurgical removal of olfactory groove meningiomas. Br J Neurosurg. 1996 Dec;10(6):541–545. doi: 10.1080/02688699646835. [DOI] [PubMed] [Google Scholar]
- Ojemann R. G., Thornton A. F., Harsh G. R. Management of anterior cranial base and cavernous sinus neoplasms with conservative surgery alone or in combination with fractionated photon or stereotactic proton radiotherapy. Clin Neurosurg. 1995;42:71–98. [PubMed] [Google Scholar]
- Salpietro F. M., Alafaci C., Lucerna S., Iacopino D. G., Todaro C., Tomasello F. Peritumoral edema in meningiomas: microsurgical observations of different brain tumor interfaces related to computed tomography. Neurosurgery. 1994 Oct;35(4):638–642. doi: 10.1227/00006123-199410000-00009. [DOI] [PubMed] [Google Scholar]
- Schaller C., Rohde V., Hassler W. Microsurgical Removal of Olfactory Groove Meningiomas via the Pterional Approach. Skull Base Surg. 1994;4(4):189–192. doi: 10.1055/s-2008-1058954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solero C. L., Giombini S., Morello G. Suprasellar and olfactory meningiomas. Report on a series of 153 personal cases. Acta Neurochir (Wien) 1983;67(3-4):181–194. doi: 10.1007/BF01401420. [DOI] [PubMed] [Google Scholar]
- Stuss D. T., Benson D. F. Neuropsychological studies of the frontal lobes. Psychol Bull. 1984 Jan;95(1):3–28. [PubMed] [Google Scholar]
- Symon L., Rosenstein J. Surgical management of suprasellar meningioma. Part 1: The influence of tumor size, duration of symptoms, and microsurgery on surgical outcome in 101 consecutive cases. J Neurosurg. 1984 Oct;61(4):633–641. doi: 10.3171/jns.1984.61.4.0633. [DOI] [PubMed] [Google Scholar]
- Tsuchiya K., Mizutani Y., Hachiya J. Preliminary evaluation of fluid-attenuated inversion-recovery MR in the diagnosis of intracranial tumors. AJNR Am J Neuroradiol. 1996 Jun-Jul;17(6):1081–1086. [PMC free article] [PubMed] [Google Scholar]