Abstract
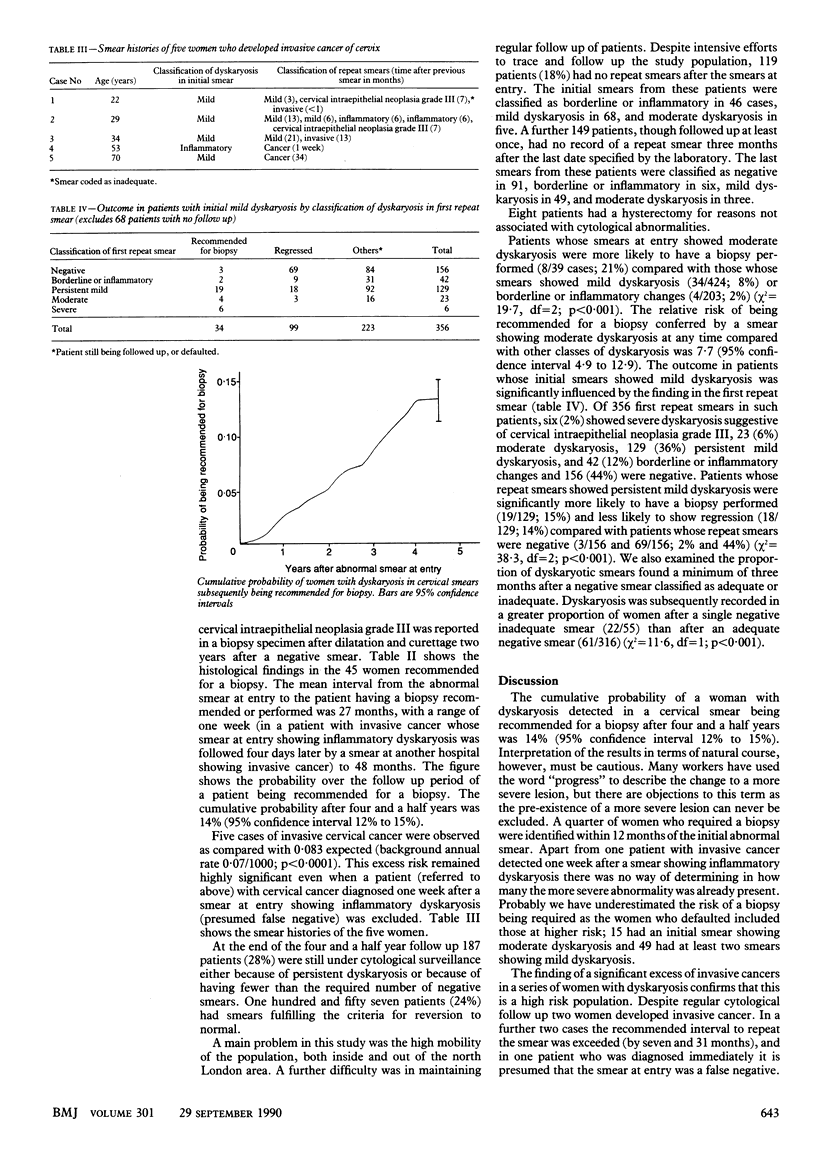
OBJECTIVE--To determine the proportion of women with mild or moderate dyskaryosis in cervical smears who (a) progress to cervical intraepithelial neoplasia grade III or worse or (b) regress. DESIGN--Four and a half year cytological follow up study of women with mild or moderate dyskaryosis in cervical smears. SETTING--666 Women (mean age 28 (SD 8) years; range 14-74) found to have borderline, mild, or moderate dyskaryosis on routine screening. RESULTS--45 Women (6.8%) had a cone biopsy recommended on the basis of an abnormal follow up smear (severe dyskaryosis suggestive of cervical intraepithelial neoplasia grade III or invasive cancer), and in one patient cervical intraepithelial neoplasia grade III was reported in a biopsy specimen after dilatation and curettage. Life table analysis gave a 14% probability of a patient being recommended for a biopsy after four and a half years of follow up (95% confidence interval 12% to 15%). There was a significant excess incidence of invasive cancer of the cervix in the series compared with the general population (five cases observed compared with less than 0.1 expected). 157 Patients (24%) showed reversion to a normal cell pattern sustained in several smears over more than 18 months but a single negative smear was an unreliable indicator of apparent regression. Having two successive smears showing mild dyskaryosis or a smear at any time showing moderate dyskaryosis was a significant predictor of a subsequent severely dyskaryotic smear. CONCLUSIONS--Women found to have mild or moderate dyskaryosis in cervical smears should be kept under regular surveillance. The optimum management of these patients--by cytology or colposcopy--needs to be determined by randomised controlled trials.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Berget A. Epithelial dysplasia of the cervix uteri. The population screening for cervical carcinoma in the County of Maribo, 1967-69. Dan Med Bull. 1974 Aug;21(5):169–171. [PubMed] [Google Scholar]
- Bounds W., Grubb C., Metaxas N., Vessey M. A randomized comparative trial of the performance of the Ayre and the Armovical cervical spatulae. Br J Obstet Gynaecol. 1976 Dec;83(12):981–987. doi: 10.1111/j.1471-0528.1976.tb00785.x. [DOI] [PubMed] [Google Scholar]
- Campion M. J., McCance D. J., Cuzick J., Singer A. Progressive potential of mild cervical atypia: prospective cytological, colposcopic, and virological study. Lancet. 1986 Aug 2;2(8501):237–240. doi: 10.1016/s0140-6736(86)92067-2. [DOI] [PubMed] [Google Scholar]
- Campion M. J., Singer A., Mitchell H. S. Complacency in diagnosis of cervical cancer. Br Med J (Clin Res Ed) 1987 May 23;294(6583):1337–1339. doi: 10.1136/bmj.294.6583.1337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook G. A., Draper G. J. Trends in cervical cancer and carcinoma in situ in Great Britain. Br J Cancer. 1984 Sep;50(3):367–375. doi: 10.1038/bjc.1984.185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fox H. Cervical smears: new terminology and new demands. Br Med J (Clin Res Ed) 1987 May 23;294(6583):1307–1308. doi: 10.1136/bmj.294.6583.1307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hulka B. S. Cytologic and histologic outcome following an atypical cervical smear. Am J Obstet Gynecol. 1968 May 15;101(2):190–199. doi: 10.1016/0002-9378(68)90187-7. [DOI] [PubMed] [Google Scholar]
- Hulka B. S., Redmond C. K. Factors related to progression of cervical atypias. Am J Epidemiol. 1971 Jan;93(1):23–32. doi: 10.1093/oxfordjournals.aje.a121225. [DOI] [PubMed] [Google Scholar]
- Husain O. A., Butler E. B., Evans D. M., Macgregor J. E., Yule R. Quality control in cervical cytology. J Clin Pathol. 1974 Dec;27(12):935–944. doi: 10.1136/jcp.27.12.935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- KOSS L. G., STEWART F., FOOTE F. W., JORDAN M. J., BADER G. M., DAY E. SOME HISTOLOGICAL ASPECTS OF BEHAVIOR OF EPIDERMOID CARCINOMA IN SITU AND RELATED LESIONS OF THE UTERINE CERVIX. A LONG-TERM PROSPECTIVE STUDY. Cancer. 1963 Sep;16:1160–1211. doi: 10.1002/1097-0142(196309)16:9<1160::aid-cncr2820160910>3.0.co;2-4. [DOI] [PubMed] [Google Scholar]
- Nasiell K., Nasiell M., Vaćlavinková V. Behavior of moderate cervical dysplasia during long-term follow-up. Obstet Gynecol. 1983 May;61(5):609–614. [PubMed] [Google Scholar]
- Parkin D. M., Leach K., Cobb P., Clayden A. D. Cervical cytology screening in two Yorkshire areas: results of testing. Public Health. 1982 Jan;96(1):3–14. doi: 10.1016/s0033-3506(82)80023-1. [DOI] [PubMed] [Google Scholar]
- Robertson J. H., Woodend B. E., Crozier E. H., Hutchinson J. Risk of cervical cancer associated with mild dyskaryosis. BMJ. 1988 Jul 2;297(6640):18–21. doi: 10.1136/bmj.297.6640.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singer A. The abnormal cervical smear. Br Med J (Clin Res Ed) 1986 Dec 13;293(6561):1551–1556. doi: 10.1136/bmj.293.6561.1551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spriggs A. I., Boddington M. M. Progression and regression of cervical lesions. Review of smears from women followed without initial biopsy or treatment. J Clin Pathol. 1980 Jun;33(6):517–522. doi: 10.1136/jcp.33.6.517. [DOI] [PMC free article] [PubMed] [Google Scholar]


