Abstract
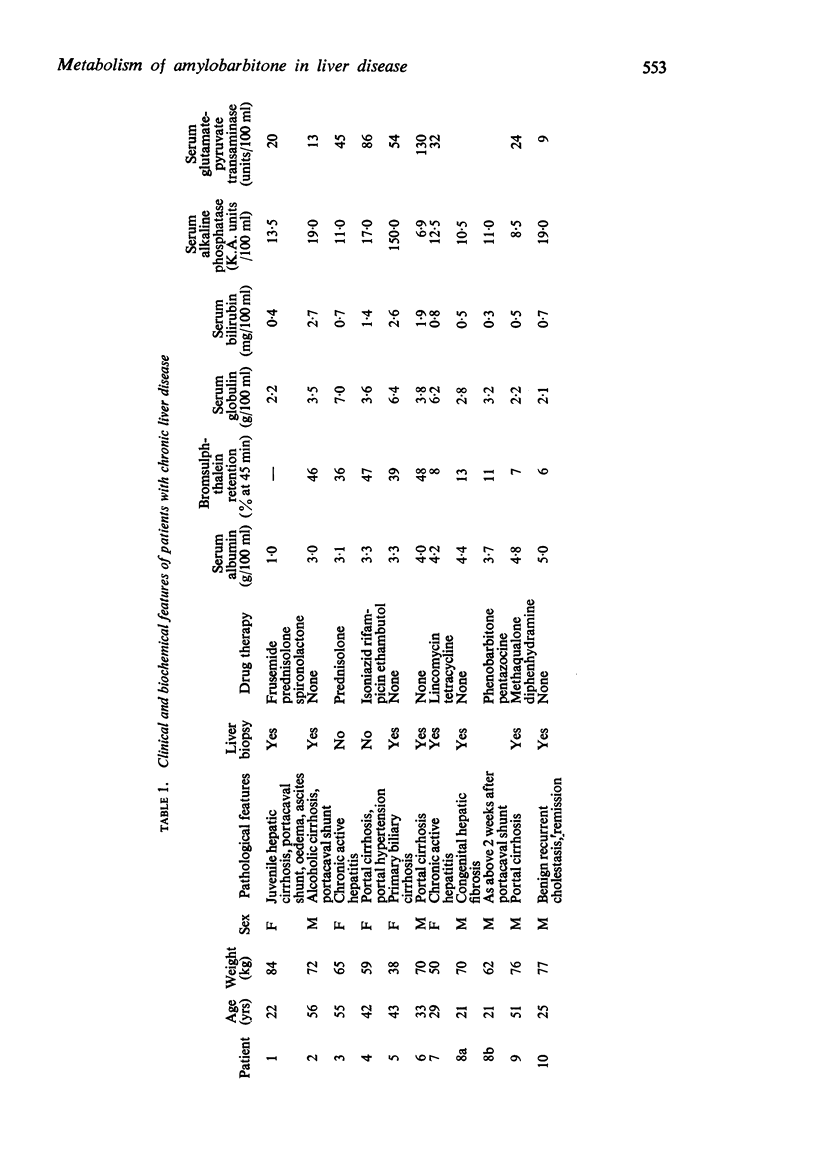
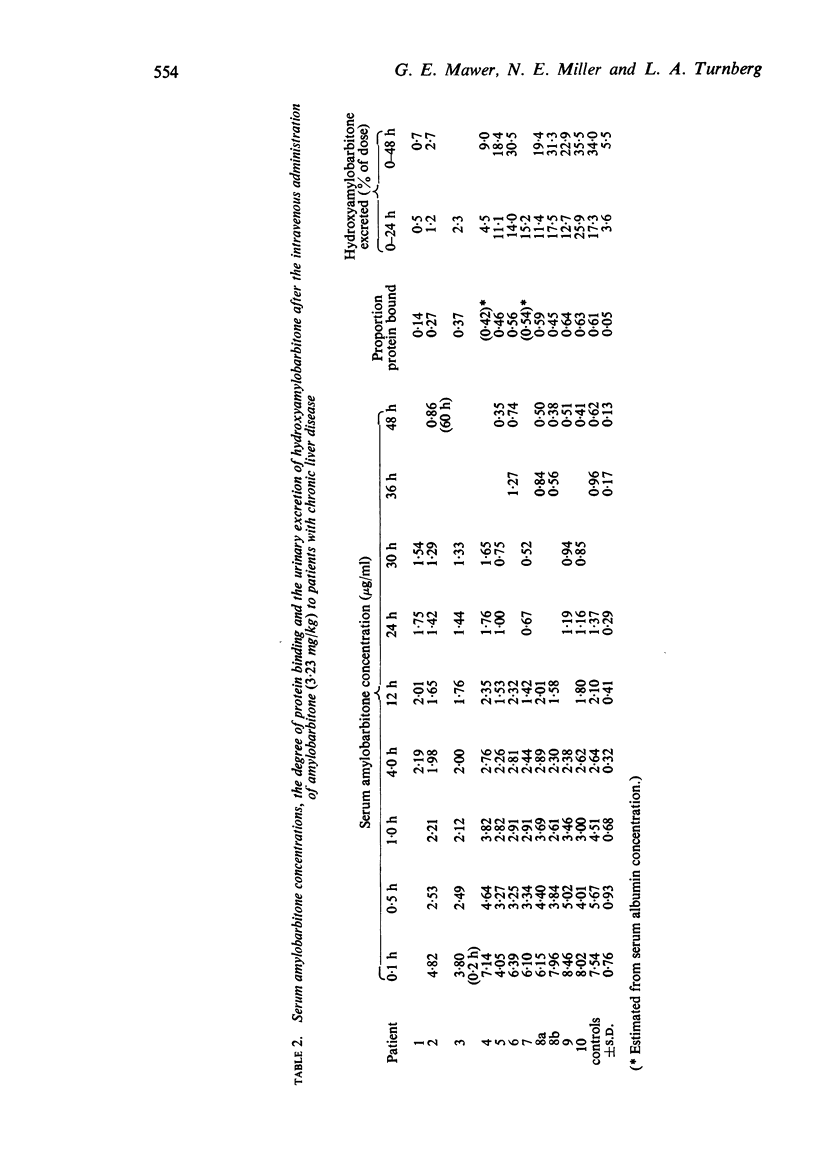
1. A single dose of amylobarbitone (3·23 mg/kg) was given by intravenous injection to each of ten healthy controls and two groups of five patients with chronic liver disease. A curve of serum amylobarbitone concentration against time was prepared for each subject and the proportion of the serum amylobarbitone bound to protein determined. The urinary excretion of the metabolite hydroxyamylobarbitone, ethyl (3 hydroxyisoamyl) barbituric acid was measured.
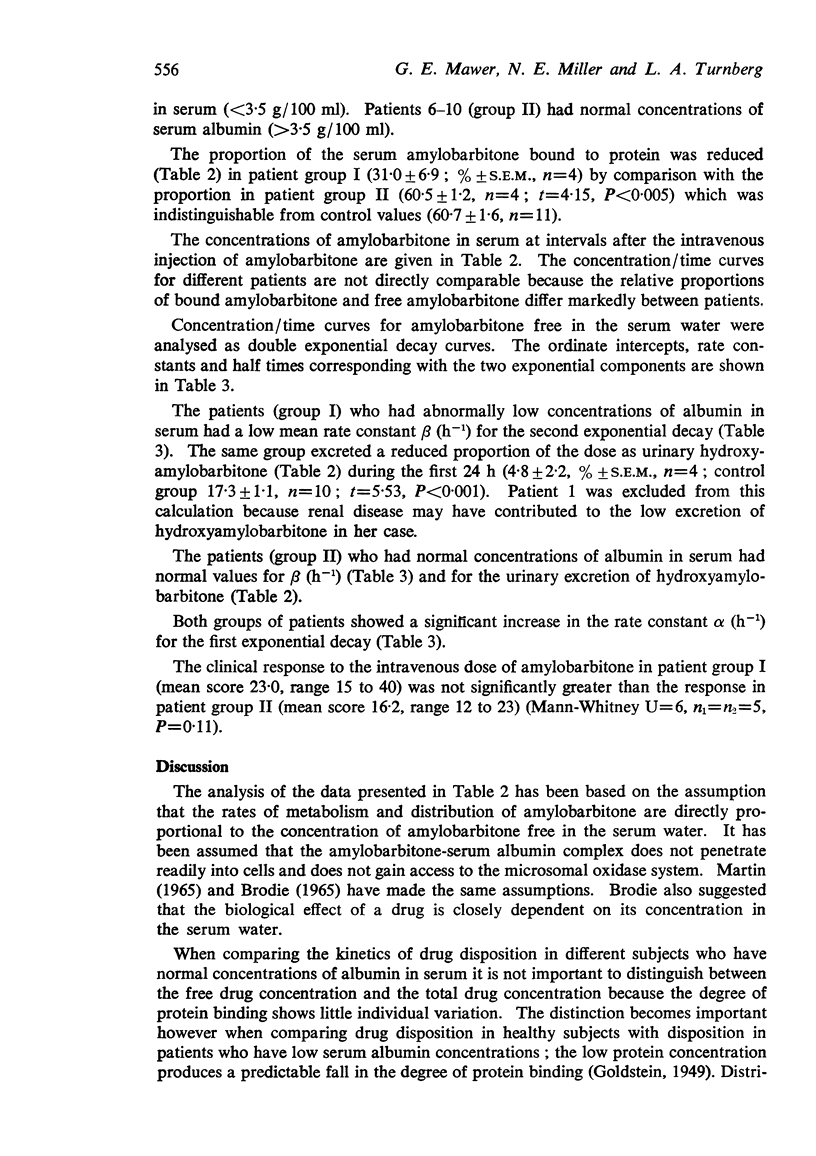
2. The degree of protein binding of serum amylobarbitone was reduced in the five patients (group I) with abnormally low concentrations of albumin in serum (<3·5 g/100 ml) but was normal in the five patients (group II) with normal serum albumin concentrations (>3·5 g/100 ml).
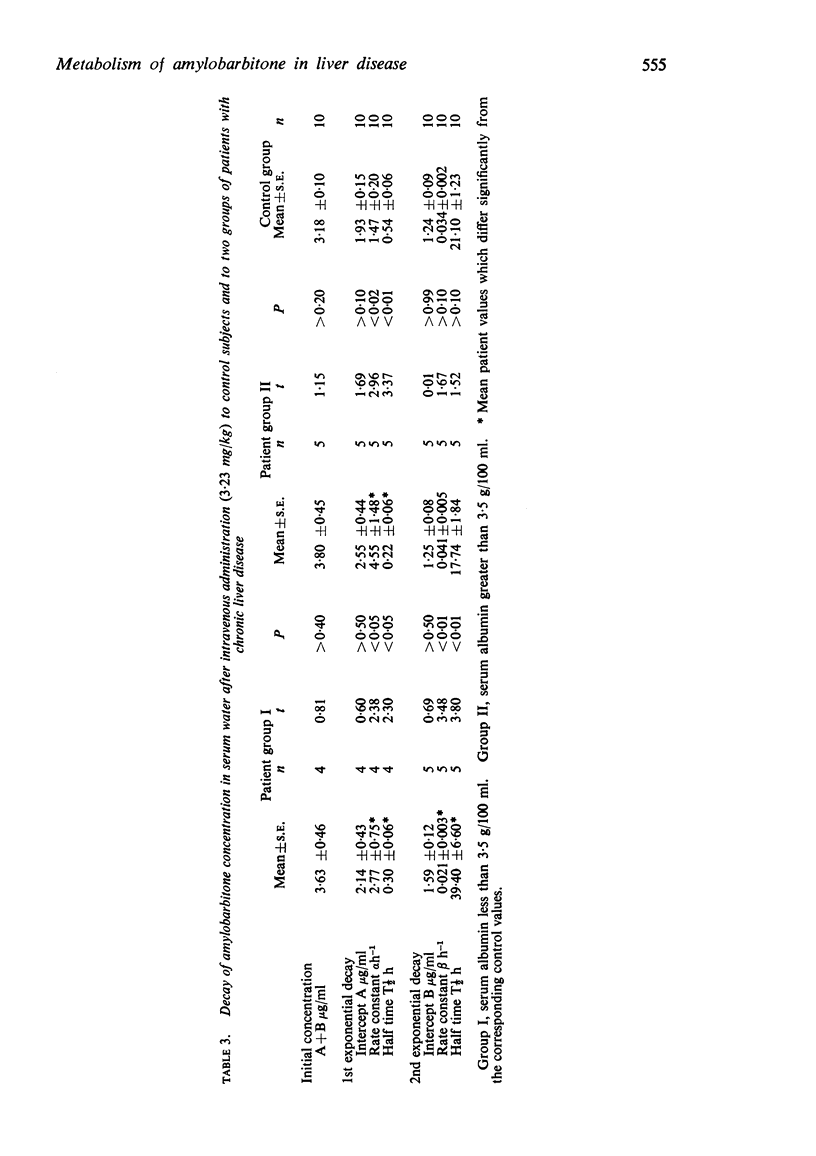
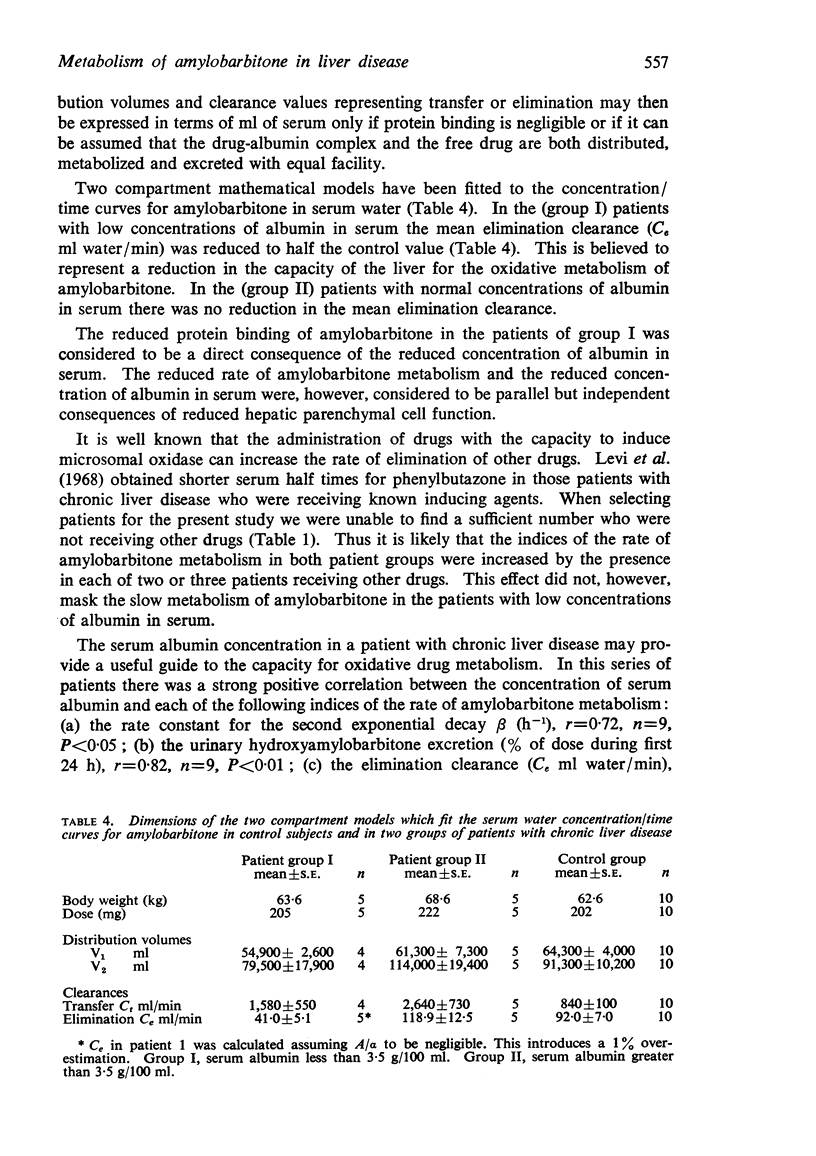
3. The equation for a double exponential decay was fitted to the concentration/time curves for amylobarbitone free in the serum water. The mean intercepts and rate constants were used to calculate the dimensions of mathematical models based on a two compartment open system.
4. The five patients (group I) who had abnormally low concentrations of albumin in serum showed impairment of amylobarbitone metabolism; the rate constant β(h-1) for the second exponential decay of serum amylobarbitone concentration was reduced (P<0·01), the urinary excretion of hydroxyamylobarbitone was reduced (P<0·001) and the mean serum water clearance (C, ml/min) representing amylobarbitone elimination by metabolism was reduced.
5. The five patients (group II) who had normal concentrations of albumin in serum showed no impairment of amylobarbitone metabolism. Within the total patient group there were strong and significant positive correlations between the serum albumin concentration and each of the indices of the rate of amylobarbitone metabolism.
6. Both patient groups showed an increase in the first dispositional rate constant α(h-1) and in the clearance (Ct ml/min) representing transfer between central and peripheral compartments. The physiological basis for this observation is uncertain.
7. The clinical response to the single intravenous dose of amylobarbitone was not significantly greater (P=0·11) in the patient group (I) with slow amylobarbitone metabolism than in the patient group (II) with a normal rate of amylobarbitone metabolism.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- BRODIE B. B., AXELROD J., COOPER J. R., GAUDETTE L., LA DU B. N., MITOMA C., UDENFRIEND S. Detoxication of drugs and other foreign compounds by liver microsomes. Science. 1955 Apr 22;121(3147):603–604. doi: 10.1126/science.121.3147.603. [DOI] [PubMed] [Google Scholar]
- Balasubramaniam K., Lucas S. B., Mawer G. E., Simons P. J. The kinetics of amylobarbitone metabolism in healthy men and women. Br J Pharmacol. 1970 Jul;39(3):564–572. doi: 10.1111/j.1476-5381.1970.tb10364.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balasubramaniam K., Mawer G. E., Rodgers E. M. The estimation of amylobarbitone and hydroxyamylobarbitone in serum by gas liquid chromatography. Br J Pharmacol. 1969 Oct;37(2):546P–547P. [PMC free article] [PubMed] [Google Scholar]
- Brodie B. B. Displacement of one drug by another from carrier or receptor sites. Proc R Soc Med. 1965 Nov;58(11 Pt 2):946–955. [PMC free article] [PubMed] [Google Scholar]
- Bush M. T., Sanders E. Metabolic fate of drugs: barbiturates and closely related compounds. Annu Rev Pharmacol. 1967;7:57–76. doi: 10.1146/annurev.pa.07.040167.000421. [DOI] [PubMed] [Google Scholar]
- DUNDEE J. W. Thiopentone narcosis in the presence of hepatic dysfunction. Br J Anaesth. 1952 Apr;24(2):81–100. doi: 10.1093/bja/24.2.81. [DOI] [PubMed] [Google Scholar]
- FOUTS J. R. The metabolism of drugs by subfractions of hepatic microsomes. Biochem Biophys Res Commun. 1961 Dec 20;6:373–378. doi: 10.1016/0006-291x(61)90148-6. [DOI] [PubMed] [Google Scholar]
- KATO R., CHIESARA E., VASSANELLI P. Factors influencing induction of hepatic microsomal drug-metabolizing enzymes. Biochem Pharmacol. 1962 Mar;11:211–220. doi: 10.1016/0006-2952(62)90076-x. [DOI] [PubMed] [Google Scholar]
- KONTOS H. A., SHAPIRO W., MAUCK H. P., PATTERSON J. L., Jr GENERAL AND REGIONAL CIRCULATORY ALTERATIONS IN CIRRHOSIS OF THE LIVER. Am J Med. 1964 Oct;37:526–535. doi: 10.1016/0002-9343(64)90066-x. [DOI] [PubMed] [Google Scholar]
- Kamm J. J., Van Loon E. J. Amobarbital metabolism in man. A gas chromatographic method for the estimation of hydroxyamobarbital in human urine. Clin Chem. 1966 Nov;12(11):789–796. [PubMed] [Google Scholar]
- LAIDLAW J., READ A. E., SHERLOCK S. Morphine tolerance in hepatic cirrhosis. Gastroenterology. 1961 Mar;40:389–396. [PubMed] [Google Scholar]
- Levi A. J., Sherlock S., Walker D. Phenylbutazone and isoniazid metabolism in patients with liver disease in relation to previous drug therapy. Lancet. 1968 Jun 15;1(7555):1275–1279. doi: 10.1016/s0140-6736(68)92292-7. [DOI] [PubMed] [Google Scholar]
- Martin B. K. Potential effect of the plasma on drug distribution. Nature. 1965 Jul 17;207(994):274–276. doi: 10.1038/207274a0. [DOI] [PubMed] [Google Scholar]
- Mawer G. W., Miller N. E., Turnberg L. A. Preliminary observations on the elimination of amylobarbitone by patients with chronic liver disease. Br J Pharmacol. 1970 Nov;40(3):579P–580P. [PMC free article] [PubMed] [Google Scholar]
- Maynert E. W. The alcoholic metabolites of pentobarbital and amobarbital in man. J Pharmacol Exp Ther. 1965 Oct;150(1):118–121. [PubMed] [Google Scholar]
- RAVENTOS J. The distribution in the body and metabolic fate of barbiturates. J Pharm Pharmacol. 1954 Apr;6(4):217–235. [PubMed] [Google Scholar]
- REDEKER A. G., GELLER H. M., REYNOLDS T. B. Hepatic wedge pressure, blood flow, vascular resistance and oxygen consumption in cirrhosis before and after end-to-side portacaval shunt. J Clin Invest. 1958 Apr;37(4):606–618. doi: 10.1172/JCI103643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riegelman S., Loo J. C., Rowland M. Shortcomings in pharmacokinetic analysis by conceiving the body to exhibit properties of a single compartment. J Pharm Sci. 1968 Jan;57(1):117–123. doi: 10.1002/jps.2600570123. [DOI] [PubMed] [Google Scholar]
- SCHMID K., CORNU F., IMHOF P., KEBERLE H. DIE BIOCHEMISCHE DEUTUNG DER GEWOEHNUNG AN SCHLAFMITTEL. Schweiz Med Wochenschr. 1964 Feb 15;94:235–240. [PubMed] [Google Scholar]
- SESSIONS J. T., Jr, MINKEL H. P., BULLARD J. C., INGELFINGER F. J. The effect of barbiturates in patients with liver disease. J Clin Invest. 1954 Aug;33(8):1116–1127. doi: 10.1172/JCI102985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- UEDA H., SAKURAI T., OTA M., NAKAJIMA A., KAMII K., MAEZAWA H. DISAPPEARANCE RATE OF TOLBUTAMIDE IN NORMAL SUBJECTS AND IN DIABETES MELLITUS, LIVER CIRRHOSIS, AND RENAL DISEASE. Diabetes. 1963 Sep-Oct;12:414–419. doi: 10.2337/diab.12.5.414. [DOI] [PubMed] [Google Scholar]
- Walker W. H. Simple ultrafiltration apparatus. J Clin Pathol. 1967 Sep;20(5):786–787. doi: 10.1136/jcp.20.5.786. [DOI] [PMC free article] [PubMed] [Google Scholar]


