Abstract
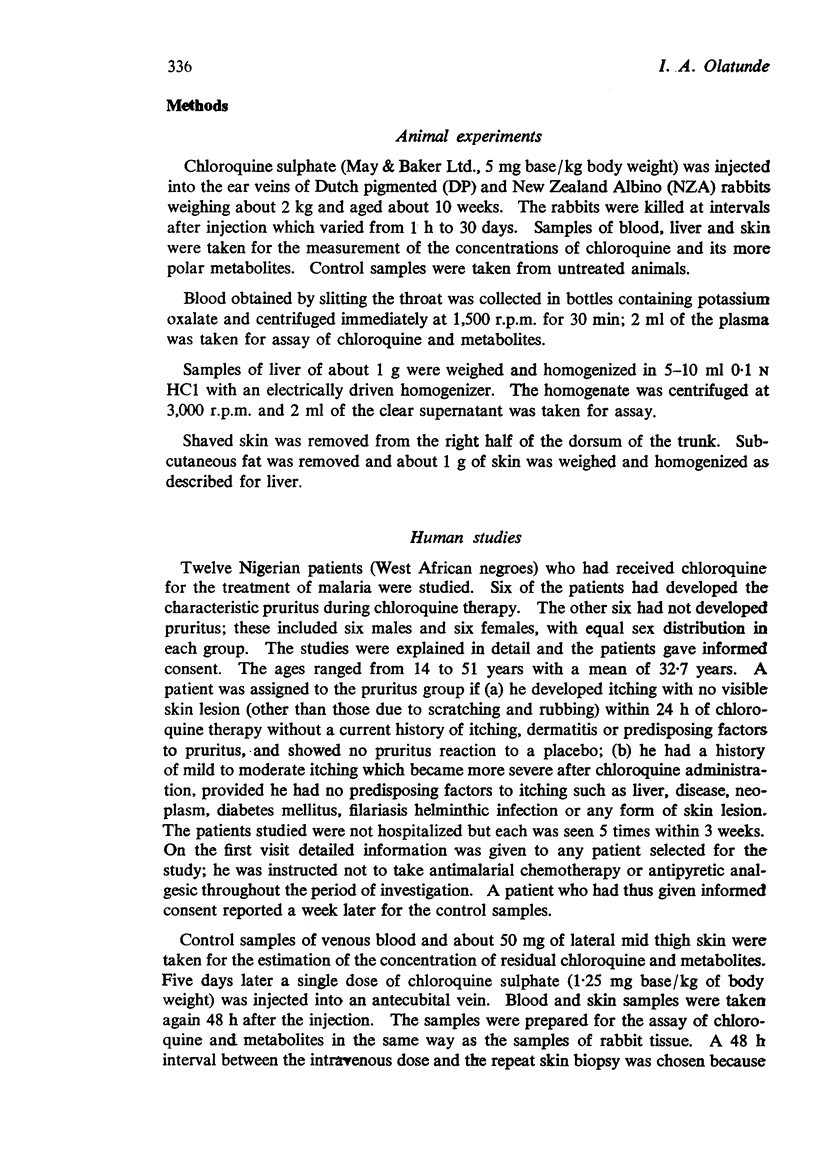
1. Chloroquine was given by a single intravenous injection to rabbits and to two groups of patients. The concentrations of the drug and its more polar metabolites in plasma and tissue were measured by a fluorometric method.
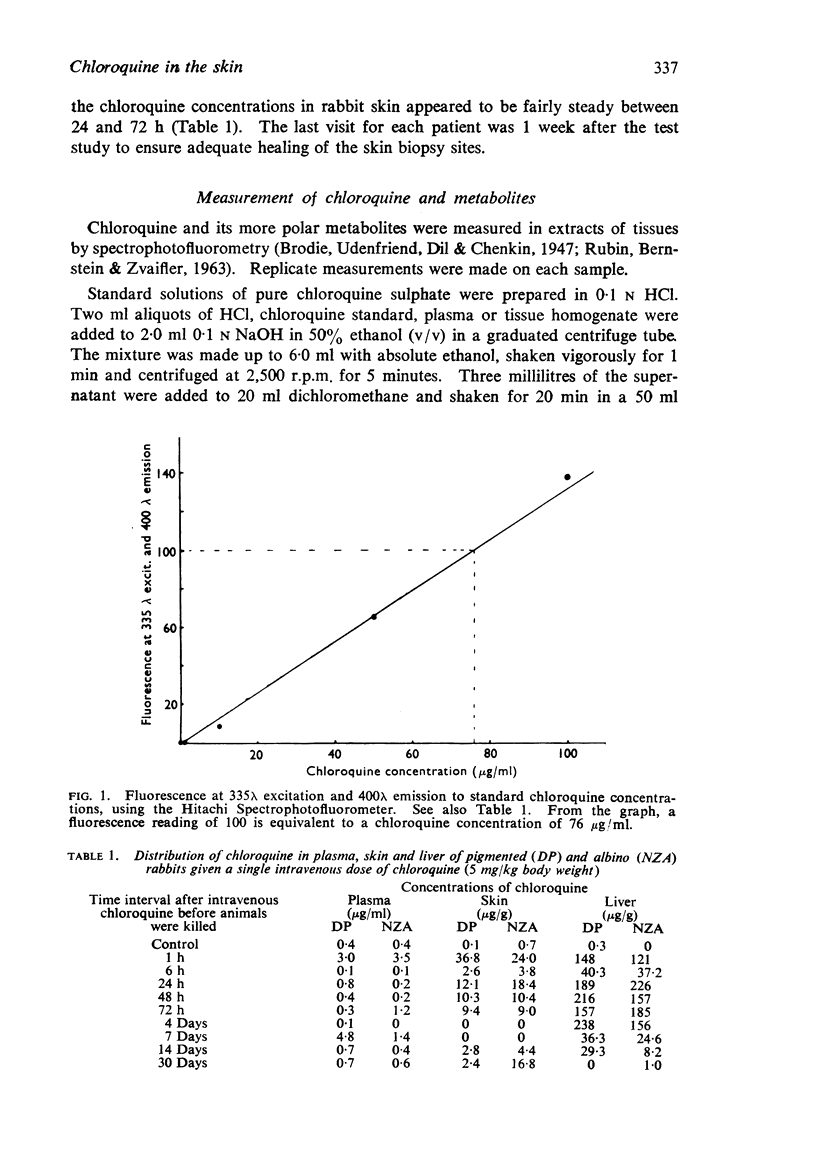
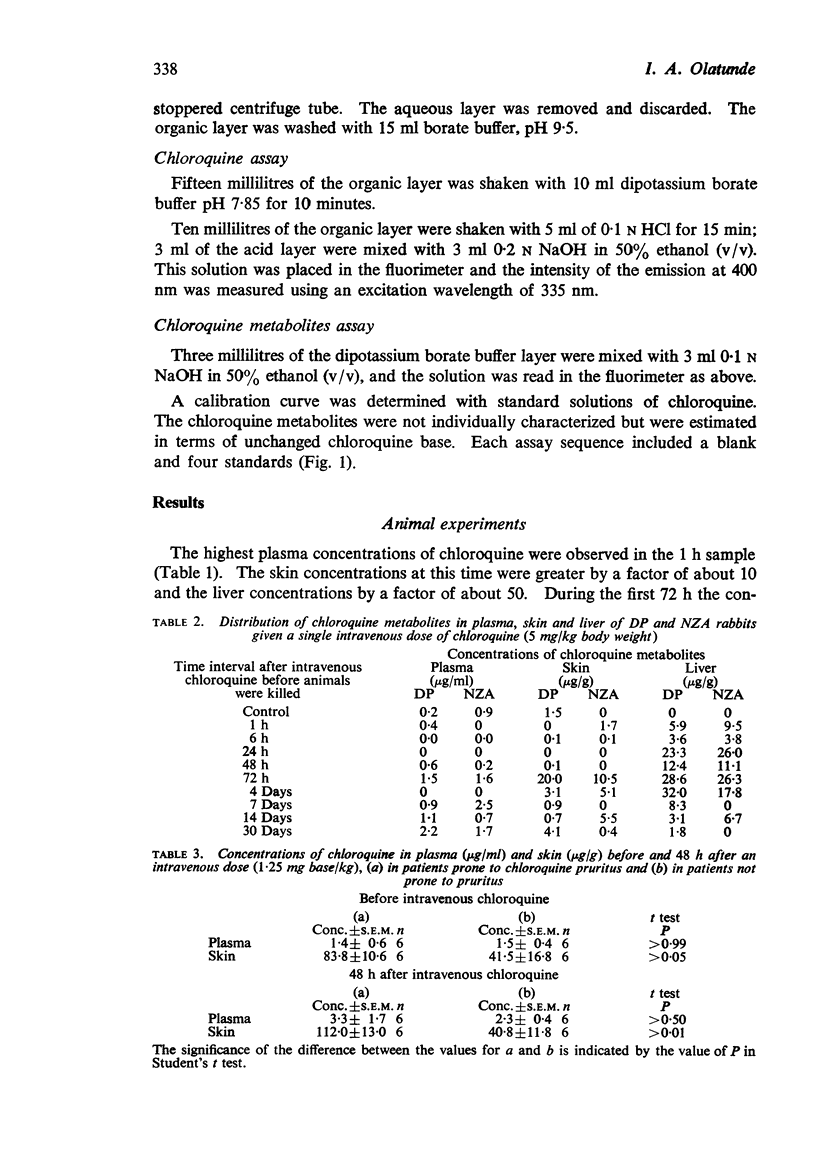
2. The concentrations of chloroquine in rabbit liver exceeded those in skin and these in turn exceeded those in plasma. Chloroquine concentrations in rabbit skin were fairly steady between 24 and 72 h after injection. Chloroquine was still present in skin 30 days after the injection. Metabolites of chloroquine were present in plasma, skin and liver.
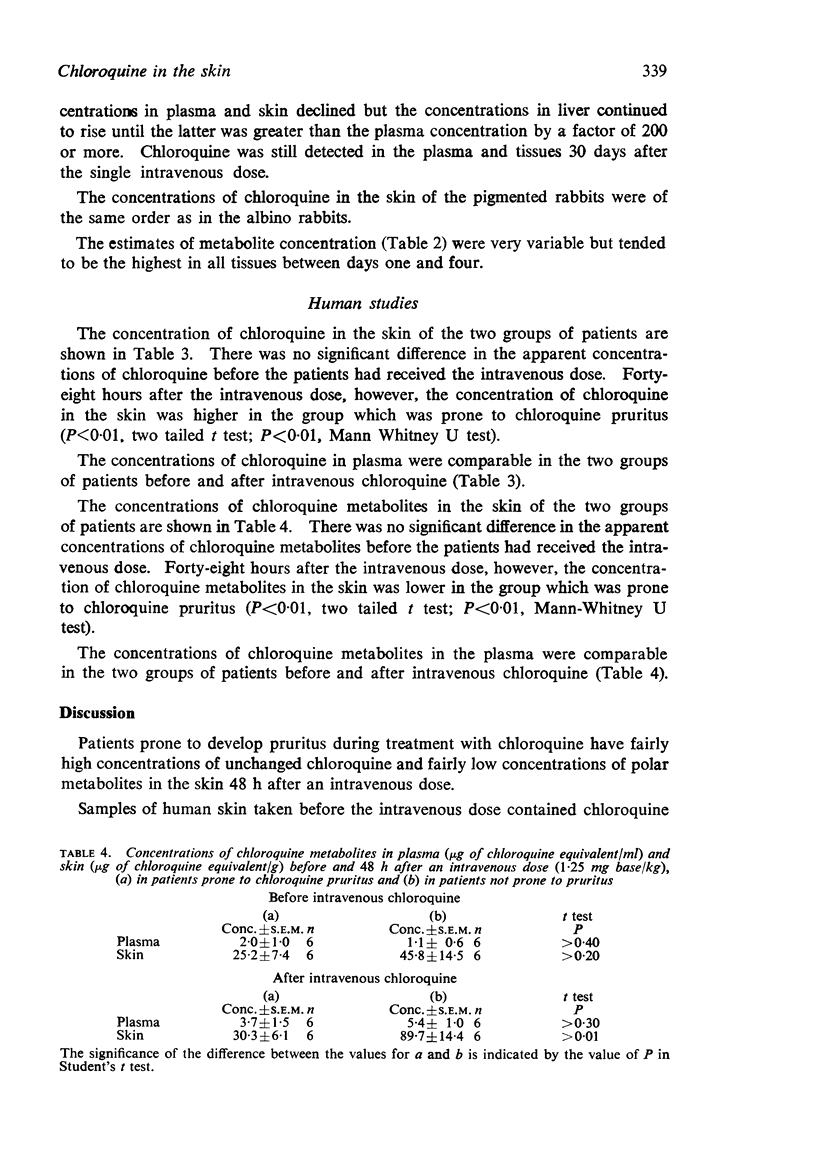
3. Skin was taken from patients 48 h after an intravenous dose of chloroquine (1·25 mg/kg). Skin from patients prone to chloroquine-induced pruritus contained higher concentrations of chloroquine (P<0·01) and lower concentrations of metabolites (P<0·01) than skin from other patients.
4. It is suggested that increased liability to chloroquine-induced pruritus may be associated with a lower rate of chloroquine metabolism.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Berliner R. W., Earle D. P., Taggart J. V., Zubrod C. G., Welch W. J., Conan N. J., Bauman E., Scudder S. T., Shannon J. A. STUDIES ON THE CHEMOTHERAPY OF THE HUMAN MALARIAS. VI. THE PHYSIOLOGICAL DISPOSITION, ANTIMALARIAL ACTIVITY, AND TOXICITY OF SEVERAL DERIVATIVES OF 4-AMINOQUINOLINE. J Clin Invest. 1948 May;27(3 Pt 2):98–107. doi: 10.1172/JCI101980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- EKPECHI O. L., OKORO A. N. A PATTERN OF PRURITUS DUE TO CHLOROQUINE. Arch Dermatol. 1964 Apr;89:631–632. doi: 10.1001/archderm.1964.01590280131024. [DOI] [PubMed] [Google Scholar]
- Knox J. M., Owens D. W. The chloroquine mystery. Arch Dermatol. 1966 Aug;94(2):205–214. [PubMed] [Google Scholar]
- MCCHESNEY E. W., NACHOD F. C., TAINTER M. L. Rationale for the treatment of lupus erythematosus with antimalarials. J Invest Dermatol. 1957 Aug;29(2):97–104. doi: 10.1038/jid.1957.76. [DOI] [PubMed] [Google Scholar]
- REES R. B., MAIBACH H. I. CHLOROQUINE. A REVIEW OF REACTIONS AND DERMATOLOGIC INDICATIONS. Arch Dermatol. 1963 Sep;88:280–289. doi: 10.1001/archderm.1963.01590210038006. [DOI] [PubMed] [Google Scholar]
- SHAFFER B., CAHN M. M., LEVY E. J. Absorption of antimalarial drugs in human skin; spectroscopic and chemical analysis in epidermis and corium. J Invest Dermatol. 1958 Jun;30(6):341–345. doi: 10.1038/jid.1958.63. [DOI] [PubMed] [Google Scholar]
- SHEE J. C., BARNARD P. J. PIGMENTATION FROM AMODIAQUINE SIMULATING CYANOSIS. Trans R Soc Trop Med Hyg. 1963 Sep;57:379–381. doi: 10.1016/0035-9203(63)90103-2. [DOI] [PubMed] [Google Scholar]
- Sams W. M., Jr, Epstein J. H. The affinity of melanin for chloroquine. J Invest Dermatol. 1965 Dec;45(6):482–487. doi: 10.1038/jid.1965.162. [DOI] [PubMed] [Google Scholar]
- TUFFANELLI D., ABRAHAM R. K., DUBOIS E. I. PIGMENTATION FROM ANTIMALARIAL THERAPY. ITS POSSIBLE RELATIONSHIP TO THE OCULAR LESIONS. Arch Dermatol. 1963 Oct;88:419–426. doi: 10.1001/archderm.1963.01590220051006. [DOI] [PubMed] [Google Scholar]


