Abstract
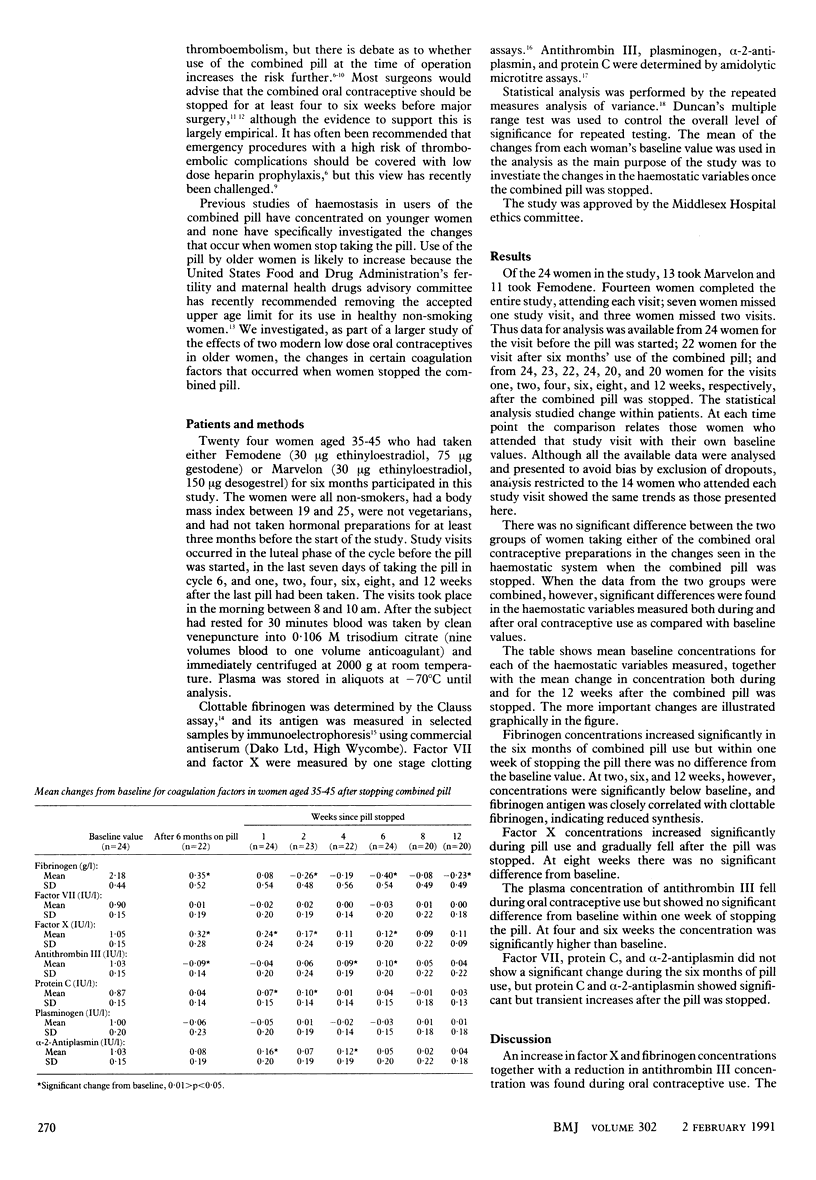
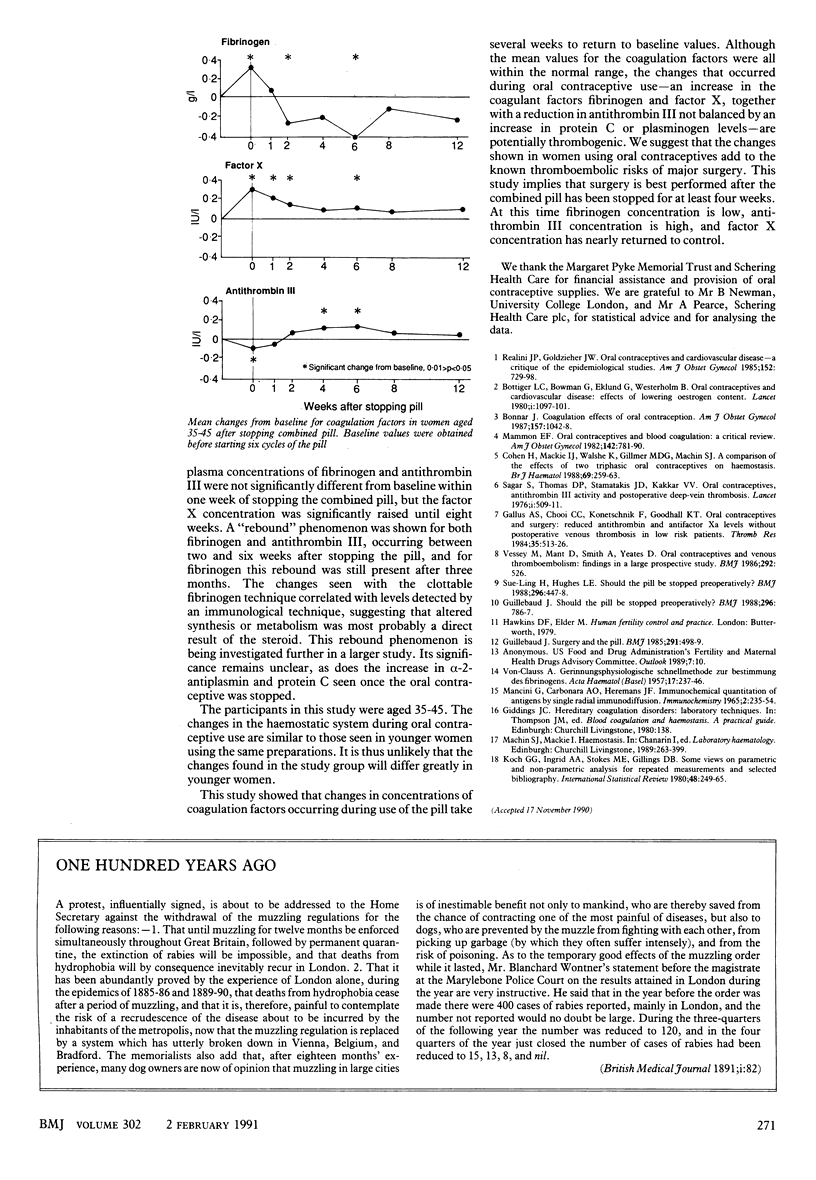
OBJECTIVE--To investigate the changes in haemostasis in the three months immediately after stopping the combined contraceptive pill. DESIGN--Prospective randomised study. SETTING--Family planning centre in London. SUBJECTS--24 women aged 35-45 investigated before, during, and after six months' use of combined oral contraceptives containing 30 micrograms ethinyl oestradiol together with the progestogens desogestrel or gestodene. MAIN OUTCOME MEASURES AND RESULTS--Blood samples were taken immediately before and after six months of oral contraceptive use and one, two, four, six, eight, and 12 weeks after the pill had been stopped. During the six months of oral contraceptive use the plasma concentration of factor X and fibrinogen increased and that of antithrombin III decreased. Between two and six weeks after stopping the pill a rebound phenomenon occurred with plasma concentrations of antithrombin III increasing (mean change from baseline at two weeks 0.06 IU/l and at six weeks 0.10 IU/l) and fibrinogen decreasing (0.26 g/l change at two weeks and 0.40 g/l at six weeks). Factor X concentrations fell gradually and the values at eight weeks were not significantly different from those found before the combined pill was started. CONCLUSION--The combined pill should be stopped at least four weeks before major surgery, which carries the risk of postoperative thrombosis, to allow the potentially prothrombotic haemostatic changes that occur during its use to be corrected.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bonnar J. Coagulation effects of oral contraception. Am J Obstet Gynecol. 1987 Oct;157(4 Pt 2):1042–1048. doi: 10.1016/s0002-9378(87)80129-1. [DOI] [PubMed] [Google Scholar]
- Böttiger L. E., Boman G., Eklund G., Westerholm B. Oral contraceptives and thromboembolic disease: effects of lowering oestrogen content. Lancet. 1980 May 24;1(8178):1097–1101. doi: 10.1016/s0140-6736(80)91550-0. [DOI] [PubMed] [Google Scholar]
- CLAUSS A. Gerinnungsphysiologische Schnellmethode zur Bestimmung des Fibrinogens. Acta Haematol. 1957 Apr;17(4):237–246. doi: 10.1159/000205234. [DOI] [PubMed] [Google Scholar]
- Cohen H., Mackie I. J., Walshe K., Gillmer M. D., Machin S. J. A comparison of the effects of two triphasic oral contraceptives on haemostasis. Br J Haematol. 1988 Jun;69(2):259–263. doi: 10.1111/j.1365-2141.1988.tb07631.x. [DOI] [PubMed] [Google Scholar]
- Guillebaud J. Surgery and the pill. Br Med J (Clin Res Ed) 1985 Aug 24;291(6494):498–499. doi: 10.1136/bmj.291.6494.498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mancini G., Carbonara A. O., Heremans J. F. Immunochemical quantitation of antigens by single radial immunodiffusion. Immunochemistry. 1965 Sep;2(3):235–254. doi: 10.1016/0019-2791(65)90004-2. [DOI] [PubMed] [Google Scholar]
- Realini J. P., Goldzieher J. W. Oral contraceptives and cardiovascular disease: a critique of the epidemiologic studies. Am J Obstet Gynecol. 1985 Jul 15;152(6 Pt 2):729–798. doi: 10.1016/s0002-9378(85)80001-6. [DOI] [PubMed] [Google Scholar]
- Sagar S., Stamatakis J. D., Thomas D. P., Kakkar V. V. Oral contraceptives, antithrombin- III activity, and postoperative deep-vein thrombosis. Lancet. 1976 Mar 6;1(7958):509–511. doi: 10.1016/s0140-6736(76)90296-8. [DOI] [PubMed] [Google Scholar]
- Sue-Ling H., Hughes L. E. Should the pill be stopped preoperatively? Br Med J (Clin Res Ed) 1988 Feb 13;296(6620):447–448. doi: 10.1136/bmj.296.6620.447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vessey M., Mant D., Smith A., Yeates D. Oral contraceptives and venous thromboembolism: findings in a large prospective study. Br Med J (Clin Res Ed) 1986 Feb 22;292(6519):526–526. doi: 10.1136/bmj.292.6519.526. [DOI] [PMC free article] [PubMed] [Google Scholar]


