Abstract
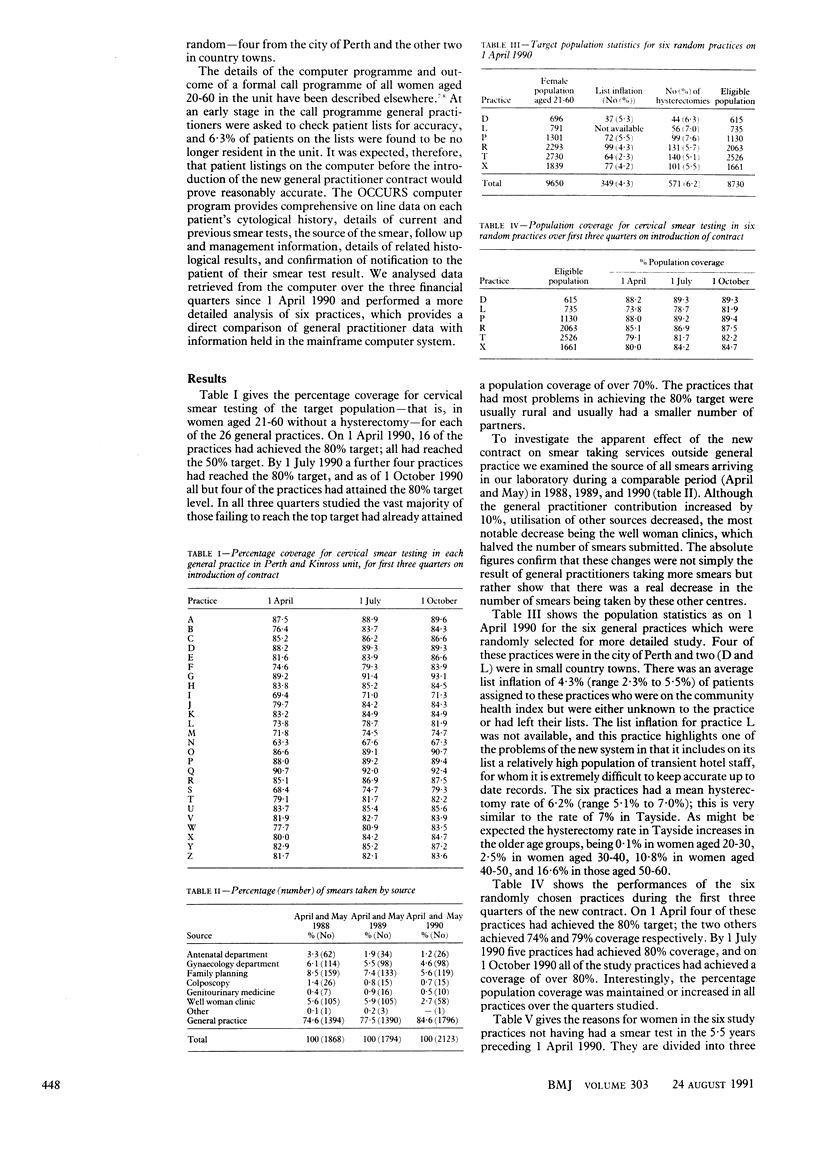
OBJECTIVE--To determine changes in the cervical screening service since the introduction of the new general practitioner contract on 1 April 1990. DESIGN--Analysis of computerised records of cervical screening both before and after introduction of the new contract. SETTING--General practices in Perth and Kinross Unit, Tayside. PATIENTS--A total of 30,071 women aged 21-60 on 26 general practitioner partnership lists. MAIN OUTCOME MEASURES--Percentage average of target population for cervical screening in each practice for first three quarters on introduction of the contract. RESULTS--Perth and Kinross Unit completed a computerised cervical screening call programme in July 1989, which produced an increase from 71% to 78% in the mean percentage of women aged 20-60 who had had cervical smear tests within 5.5 years. Six months after the introduction of the new general practitioner contract the mean population coverage was increased to 85% in women aged 21-60 and only four practices had not attained the 80% upper target compared with 10 on 1 April 1990. Detailed examination of randomly selected practices immediately before the new contract was introduced showed an average artificial list inflation of 4.3% in health board records when compared with practice records, a hysterectomy rate of 6.2%, and an additional 3% of women who were considered to be ineligible for smear testing due to putative virginity or illness or infirmity, or both. There was a considerable shift away from use of well woman clinics (2.7% of smears in 1990 compared with 5.6% in 1988) for taking cervical smears, potentially threatening the long term viability of the clinics. CONCLUSION--The introduction of the new contract for general practitioners has brought about a further sustained increase in population coverage for cervical screening in a small Scottish unit with a stable population, well motivated general practitioners, and a fully integrated computerised call and recall system based on the community health index. To optimise the screening service revision of the targets levels is necessary.
Full text
PDF


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Chamberlain J. Failures of the cervical cytology screening programme. Br Med J (Clin Res Ed) 1984 Oct 6;289(6449):853–854. doi: 10.1136/bmj.289.6449.853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chomet J., Chomet J. Cervical screening in general practice: a "new" scenario. BMJ. 1990 Jun 9;300(6738):1504–1506. doi: 10.1136/bmj.300.6738.1504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gemmell J., Holmes D. M., Duncan I. D. How frequently need vaginal smears be taken after hysterectomy for cervical intraepithelial neoplasia? Br J Obstet Gynaecol. 1990 Jan;97(1):58–61. doi: 10.1111/j.1471-0528.1990.tb01717.x. [DOI] [PubMed] [Google Scholar]
- Robertson A. J., Reid G. S., Stoker C. A., Bissett C., Waugh N., Fenton I., Rowan J., Halkerston R. How complete can cervical screening be? The outcome of a call screening programme for women aged 20-60 years in Perth and Kinross. Cytopathology. 1990;1(1):3–12. doi: 10.1111/j.1365-2303.1990.tb00320.x. [DOI] [PubMed] [Google Scholar]
- Shroff K. J., Corrigan A. M., Bosher M., Edmonds M. P., Sacks D., Coleman D. V. Cervical screening in an inner city area: response to a call system in general practice. BMJ. 1988 Nov 19;297(6659):1317–1318. doi: 10.1136/bmj.297.6659.1317. [DOI] [PMC free article] [PubMed] [Google Scholar]


