Abstract
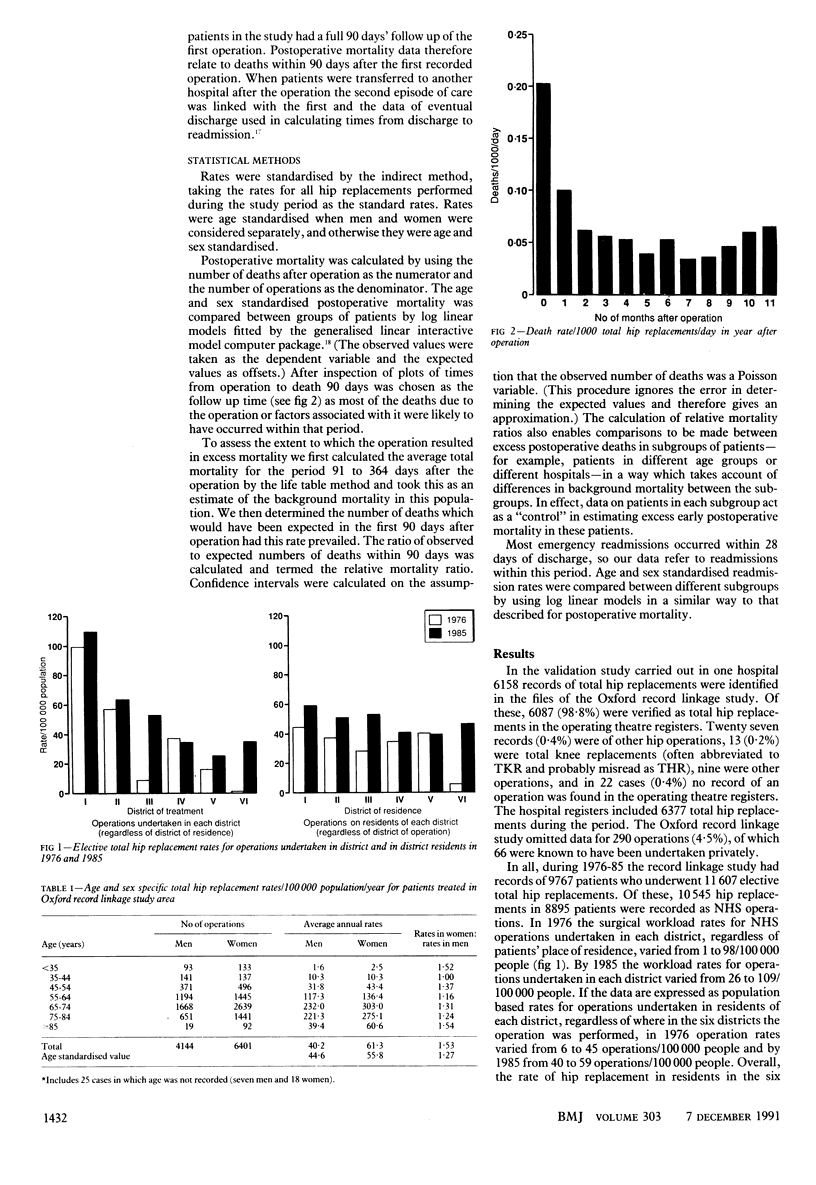
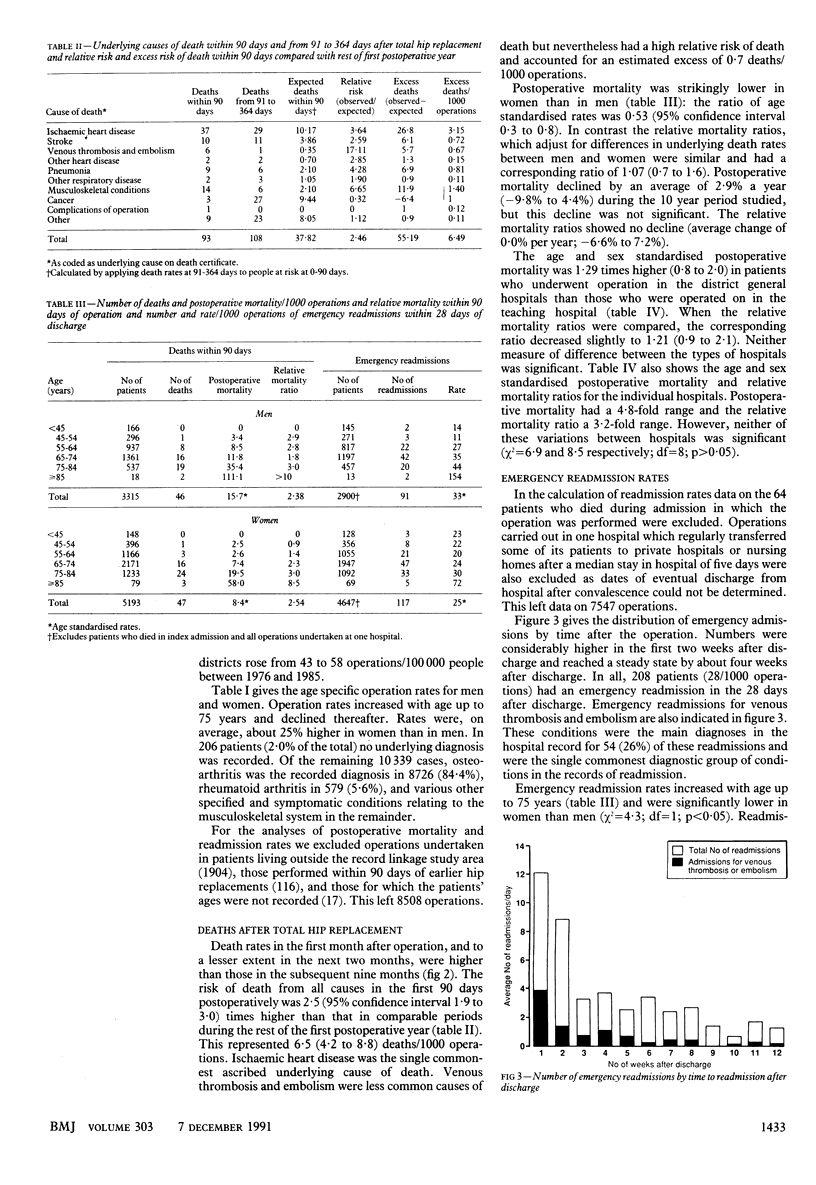
OBJECTIVES--To report the incidence of elective total hip replacement and postoperative mortality, emergency readmission rates, and the demographic factors associated with these rates in a large defined population. DESIGN--Analysis of linked, routine abstracts of hospital inpatient records and death certificates. SETTING--10 hospitals in six districts in Oxford Regional Health Authority covered by the Oxford record linkage study. SUBJECTS--Records for 11,607 total hip replacements performed electively in 1976-85. MAIN OUTCOME MEASURES--Incidence of operation, postoperative mortality, relative mortality ratios, and incidence of emergency readmission. RESULTS--NHS operation rates increased over time from 43 to 58 operations/100,000 population. Variation in operation rates between districts reduced over time. Operation rates were on average 25% higher in women than men. There were 93 deaths (11/1000 operations) within 90 days of the operation and 208 emergency readmissions (28/1000 operations) within 28 days of discharge. Postoperative mortality and emergency readmission rates increased with age. No significant trend with time was found. Mortality in the 90 days after the operation was 2.5-fold higher (1.9 to 3.0) than in the rest of the first postoperative year. This represented an estimated excess of 6.5 (4.2 to 8.8) early postoperative deaths/1000 operations. Most deaths were ascribed to cardiovascular events. Thromboembolic disease was the commonest reason for emergency readmission. CONCLUSIONS--The pronounced increase in operations in districts with initially low rates suggests a trend towards greater equity in the local provision of NHS hip arthroplasty. The early postoperative clusters of deaths attributed to cardiovascular disease and of readmissions for thromboembolic disease suggest that there is scope for investigating ways of reducing the incidence of major adverse postoperative events.
Full text
PDF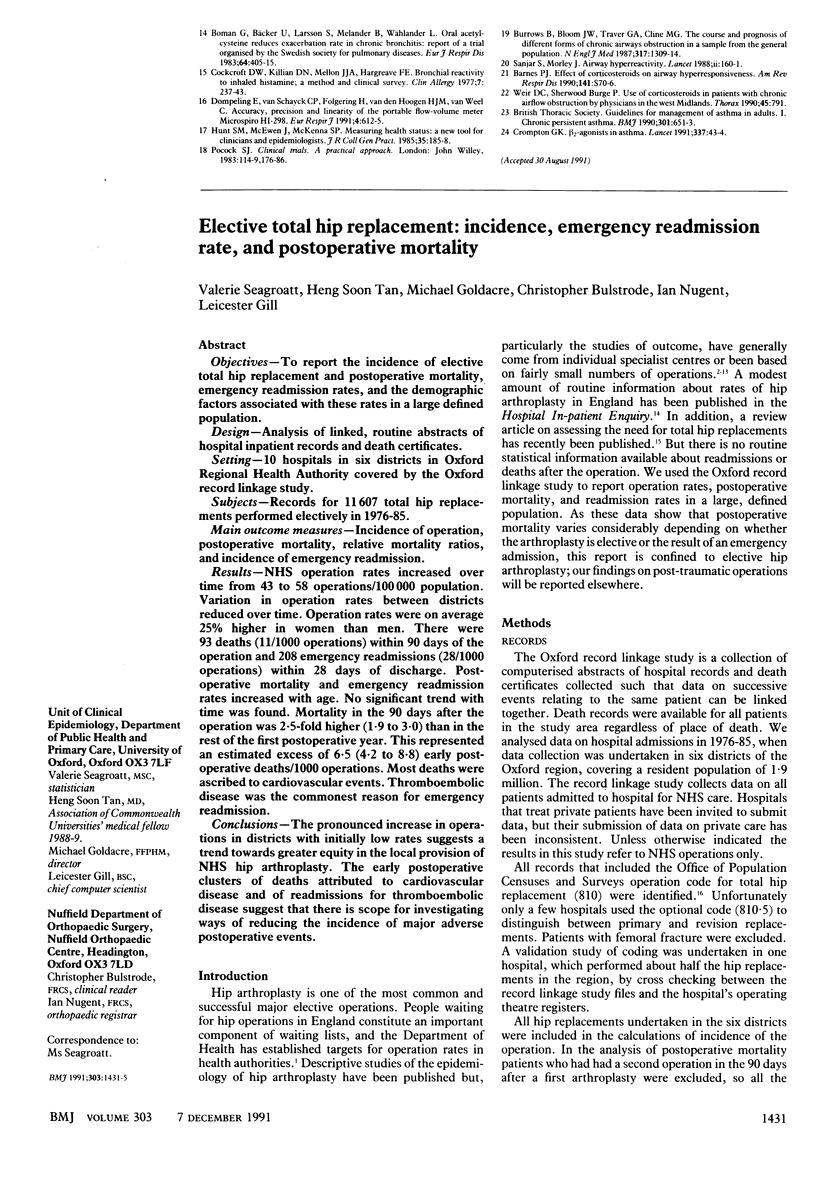

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Brady L. P., McCutchen J. W. A ten-year follow-up study of 170 Charnley total hip arthroplasties. Clin Orthop Relat Res. 1986 Oct;(211):51–54. [PubMed] [Google Scholar]
- Chandler H. P., Reineck F. T., Wixson R. L., McCarthy J. C. Total hip replacement in patients younger than thirty years old. A five-year follow-up study. J Bone Joint Surg Am. 1981 Dec;63(9):1426–1434. [PubMed] [Google Scholar]
- Charnley J. Fracture of femoral prostheses in total hip replacement. A clinical study. Clin Orthop Relat Res. 1975 Sep;(111):105–120. doi: 10.1097/00003086-197509000-00014. [DOI] [PubMed] [Google Scholar]
- Cornell C. N., Ranawat C. S. Survivorship analysis of total hip replacements. Results in a series of active patients who were less than fifty-five years old. J Bone Joint Surg Am. 1986 Dec;68(9):1430–1434. [PubMed] [Google Scholar]
- Dorr L. D., Takei G. K., Conaty J. P. Total hip arthroplasties in patients less than forty-five years old. J Bone Joint Surg Am. 1983 Apr;65(4):474–479. [PubMed] [Google Scholar]
- Gustilo R. B., Burnham W. H. Long-term results of total hip arthroplasty in young patients. Hip. 1982:27–33. [PubMed] [Google Scholar]
- Henderson J., Goldacre M. J., Graveney M. J., Simmons H. M. Use of medical record linkage to study readmission rates. BMJ. 1989 Sep 16;299(6701):709–713. doi: 10.1136/bmj.299.6701.709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lassen M. R., Borris L. C. Mobilisation after hip surgery and efficacy of thromboprophylaxis. Lancet. 1991 Mar 9;337(8741):618–618. doi: 10.1016/0140-6736(91)91686-o. [DOI] [PubMed] [Google Scholar]
- Nicholl J. P., Beeby N. R., Williams B. T. Role of the private sector in elective surgery in England and Wales, 1986. BMJ. 1989 Jan 28;298(6668):243–247. doi: 10.1136/bmj.298.6668.243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nicholl J. P., Thomas K. J., Williams B. T., Knowelden J. Contribution of the private sector to elective surgery in England and Wales. Lancet. 1984 Jul 14;2(8394):89–92. doi: 10.1016/s0140-6736(84)90253-8. [DOI] [PubMed] [Google Scholar]
- Older J. Low-friction arthroplasty of the hip. A 10-12-year follow-up study. Clin Orthop Relat Res. 1986 Oct;(211):36–42. [PubMed] [Google Scholar]
- Ranawat C. S., Atkinson R. E., Salvati E. A., Wilson P. D., Jr Conventional total hip arthroplasty for degenerative joint disease in patients between the ages of forty and sixty years. J Bone Joint Surg Am. 1984 Jun;66(5):745–752. [PubMed] [Google Scholar]
- Salvati E. A., Wilson P. D., Jr, Jolley M. N., Vakili F., Aglietti P., Brown G. C. A ten-year follow-up study of our first one hundred consecutive Charnley total hip replacements. J Bone Joint Surg Am. 1981 Jun;63(5):753–767. [PubMed] [Google Scholar]
- Terayama K. Experience with Charnley low-friction arthroplasty in Japan. Clin Orthop Relat Res. 1986 Oct;(211):79–84. [PubMed] [Google Scholar]
- Wroblewski B. M. 15-21-year results of the Charnley low-friction arthroplasty. Clin Orthop Relat Res. 1986 Oct;(211):30–35. [PubMed] [Google Scholar]
- Wroblewski B. M. Charnley low-friction arthroplasty. Review of the past, present status, and prospects for the future. Clin Orthop Relat Res. 1986 Sep;(210):37–42. [PubMed] [Google Scholar]


