Abstract
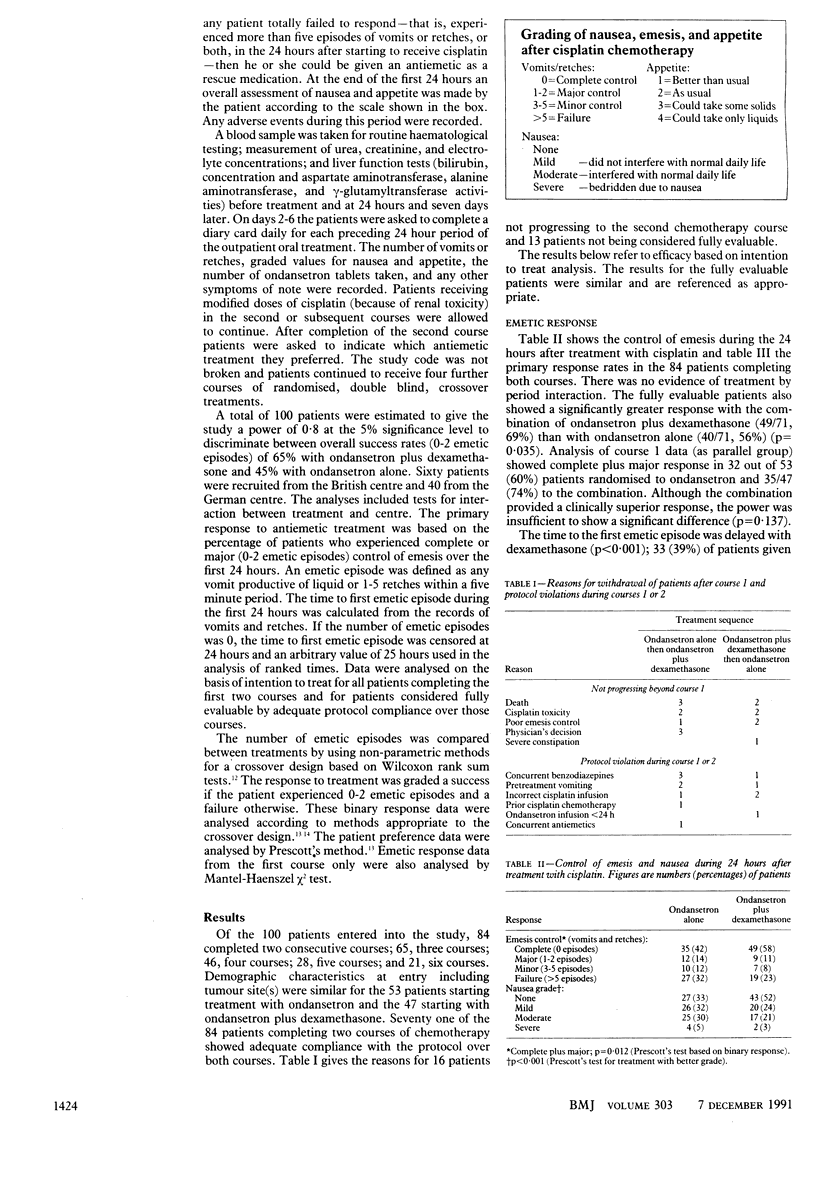
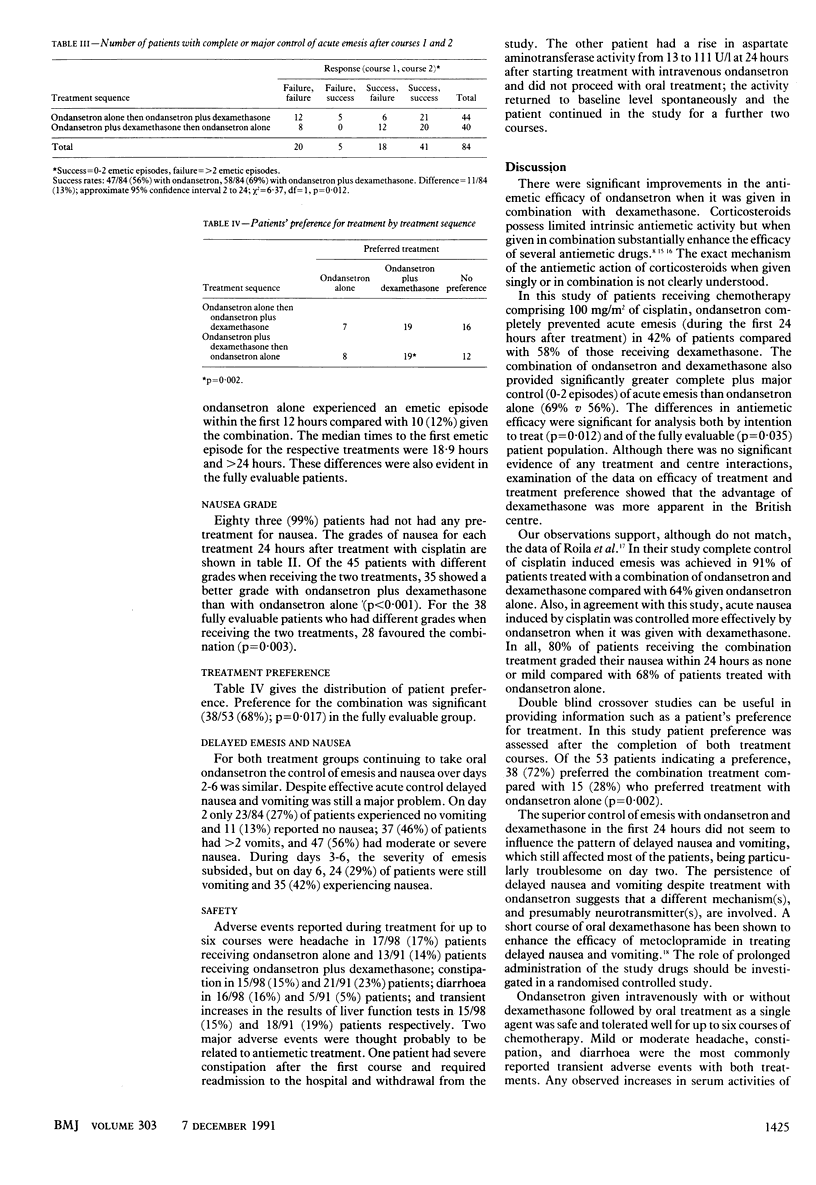
OBJECTIVE--To determine the contribution of dexamethasone to the efficacy of the 5-hydroxytryptamine antagonist ondansetron in control of cisplatin induced nausea and vomiting. DESIGN--Randomised double blind crossover study. SETTING--Two cancer centres in teaching hospitals, one in the United Kingdom and the other in Germany. SUBJECTS--100 patients (53 men and 47 women) new to cisplatin chemotherapy, 84 of whom completed two consecutive courses of chemotherapy. INTERVENTIONS--Patients were given intravenous dexamethasone (20 mg) or physiological saline with intravenous ondansetron 8 mg before cisplatin, then ondansetron 1 mg/h for 24 hours. Oral ondansetron 8 mg was taken three times daily on days 2-6. MAIN OUTCOME MEASURES--Incidence of complete or major control of emesis (0-2 episodes in the 24 hours after chemotherapy). RESULTS--Complete or major control was obtained in 49 out of 71 (69%) of patients after receiving ondansetron plus dexamethasone compared with 40 out of 71 (56%) when they were given ondansetron alone (p = 0.012). This effect was most pronounced in the first 12 hours after chemotherapy. Patients receiving the combination also had significantly less nausea. Of the 53 patients who expressed a preference, 38 (72%) preferred the combination treatment (p = 0.002) to ondansetron alone. The effect of ondansetron on delayed emesis was less pronounced. CONCLUSIONS--Dexamethasone makes a significant contribution to the efficacy of ondansetron in the control of acute platinum induced emesis.
Full text
PDF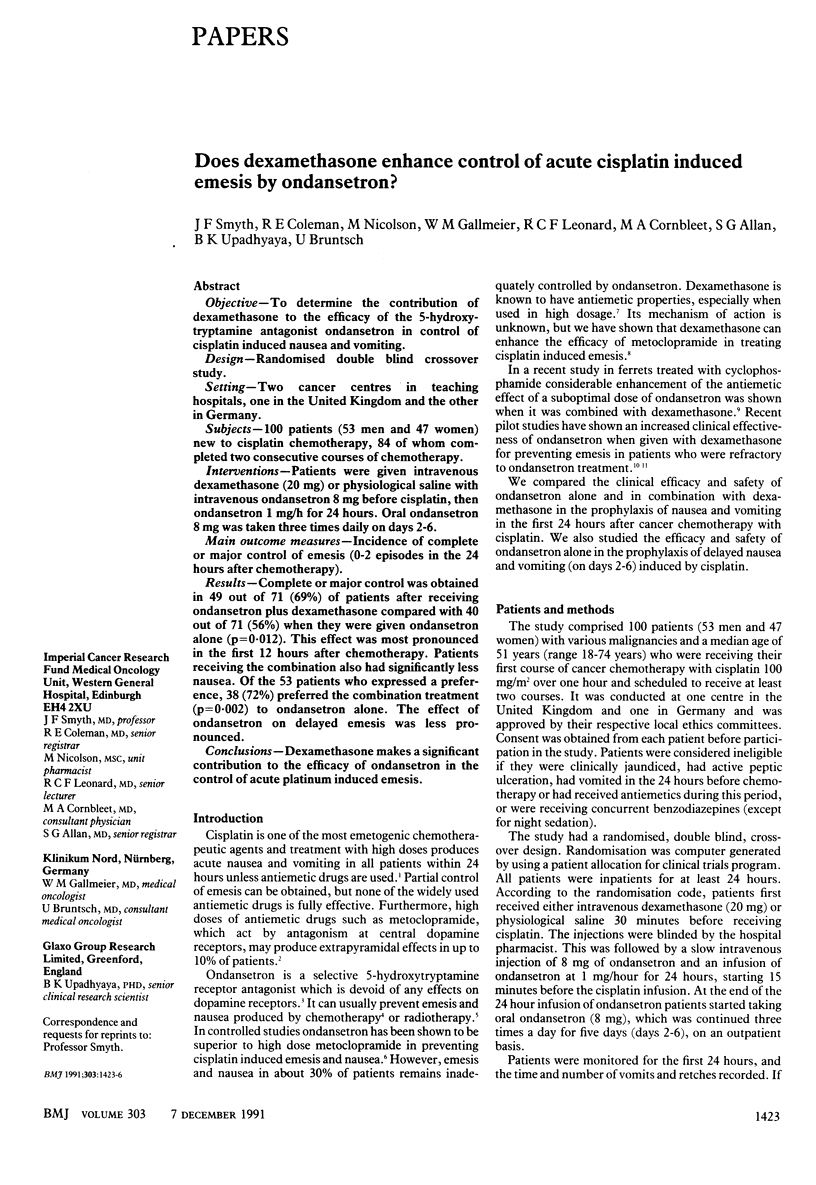

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Aapro M. S., Alberts D. S. High-dose dexamethasone for prevention of cis-platin-induced vomiting. Cancer Chemother Pharmacol. 1981;7(1):11–14. doi: 10.1007/BF00258206. [DOI] [PubMed] [Google Scholar]
- Allan S. G., Cornbleet M. A., Lockhart S. P., Warrington P. S., Leonard R. C., Smyth J. F. Emesis due to cancer chemotherapy: results of a prospective, randomised, double-blind trial of varying doses of metoclopramide in the management of cis-platinum-induced vomiting. Eur J Cancer Clin Oncol. 1984 Dec;20(12):1481–1484. doi: 10.1016/0277-5379(84)90140-8. [DOI] [PubMed] [Google Scholar]
- Allan S. G., Cornbleet M. A., Warrington P. S., Golland I. M., Leonard R. C., Smyth J. N. Dexamethasone and high dose metoclopramide: efficacy in controlling cisplatin induced nausea and vomiting. Br Med J (Clin Res Ed) 1984 Oct 6;289(6449):878–879. doi: 10.1136/bmj.289.6449.878-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allan S. G., Farquhar D. F., Harrison D. J., Leonard R. C. Anti-emetic efficacy of dexamethasone in combination for out-patients receiving cytotoxic chemotherapy. Cancer Chemother Pharmacol. 1986;18(1):86–87. doi: 10.1007/BF00253072. [DOI] [PubMed] [Google Scholar]
- Benrubi G. I., Norvell M., Nuss R. C., Robinson H. The use of methylprednisolone and metoclopramide in control of emesis in patients receiving cis-platinum. Gynecol Oncol. 1985 Jul;21(3):306–313. doi: 10.1016/0090-8258(85)90268-9. [DOI] [PubMed] [Google Scholar]
- Cunningham D., Turner A., Hawthorn J., Rosin R. D. Ondansetron with and without dexamethasone to treat chemotherapy-induced emesis. Lancet. 1989 Jun 10;1(8650):1323–1323. doi: 10.1016/s0140-6736(89)92711-6. [DOI] [PubMed] [Google Scholar]
- Hawthorn J., Cunningham D. Dexamethasone can potentiate the anti-emetic action of a 5HT3 receptor antagonist on cyclophosphamide induced vomiting in the ferret. Br J Cancer. 1990 Jan;61(1):56–60. doi: 10.1038/bjc.1990.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hills M., Armitage P. The two-period cross-over clinical trial. Br J Clin Pharmacol. 1979 Jul;8(1):7–20. doi: 10.1111/j.1365-2125.1979.tb05903.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koch G. G. The use of non-parametric methods in the statistical analysis of the two-period change-over design. Biometrics. 1972 Jun;28(2):577–584. [PubMed] [Google Scholar]
- Kris M. G., Gralla R. J., Tyson L. B., Clark R. A., Cirrincione C., Groshen S. Controlling delayed vomiting: double-blind, randomized trial comparing placebo, dexamethasone alone, and metoclopramide plus dexamethasone in patients receiving cisplatin. J Clin Oncol. 1989 Jan;7(1):108–114. doi: 10.1200/JCO.1989.7.1.108. [DOI] [PubMed] [Google Scholar]
- Laszlo J., Lucas V. S., Jr Emesis as a critical problem in chemotherapy. N Engl J Med. 1981 Oct 15;305(16):948–949. doi: 10.1056/NEJM198110153051609. [DOI] [PubMed] [Google Scholar]
- Marty M. Ondansetron in the prophylaxis of acute cisplatin-induced nausea and vomiting. Eur J Cancer Clin Oncol. 1989;25 (Suppl 1):S41–S45. [PubMed] [Google Scholar]
- Marty M., Pouillart P., Scholl S., Droz J. P., Azab M., Brion N., Pujade-Lauraine E., Paule B., Paes D., Bons J. Comparison of the 5-hydroxytryptamine3 (serotonin) antagonist ondansetron (GR 38032F) with high-dose metoclopramide in the control of cisplatin-induced emesis. N Engl J Med. 1990 Mar 22;322(12):816–821. doi: 10.1056/NEJM199003223221205. [DOI] [PubMed] [Google Scholar]
- Priestman T. J. Clinical studies with ondansetron in the control of radiation-induced emesis. Eur J Cancer Clin Oncol. 1989;25 (Suppl 1):S29–S33. [PubMed] [Google Scholar]
- Smith D. B., Newlands E. S., Spruyt O. W., Begent R. H., Rustin G. J., Mellor B., Bagshawe K. D. Ondansetron (GR38032F) plus dexamethasone: effective anti-emetic prophylaxis for patients receiving cytotoxic chemotherapy. Br J Cancer. 1990 Feb;61(2):323–324. doi: 10.1038/bjc.1990.62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tyers M. B., Bunce K. T., Humphrey P. P. Pharmacological and anti-emetic properties of ondansetron. Eur J Cancer Clin Oncol. 1989;25 (Suppl 1):S15–S19. [PubMed] [Google Scholar]


