Abstract
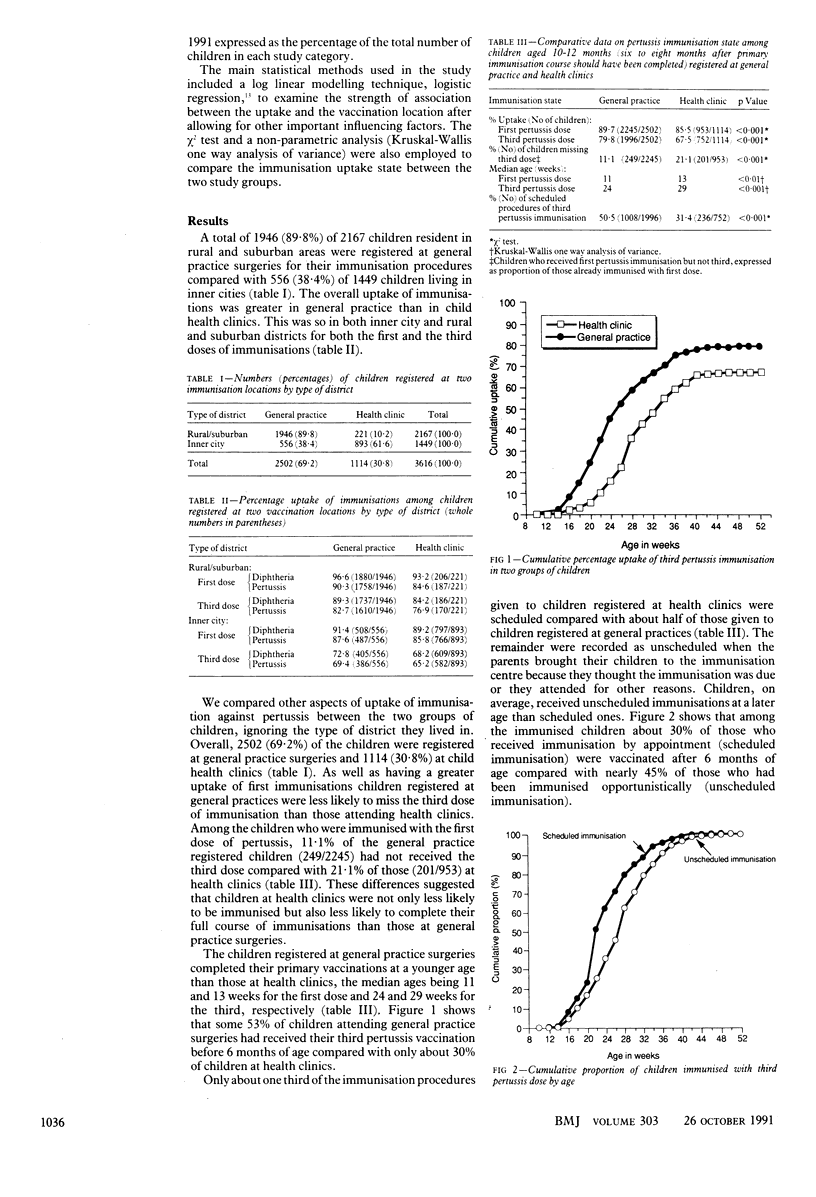
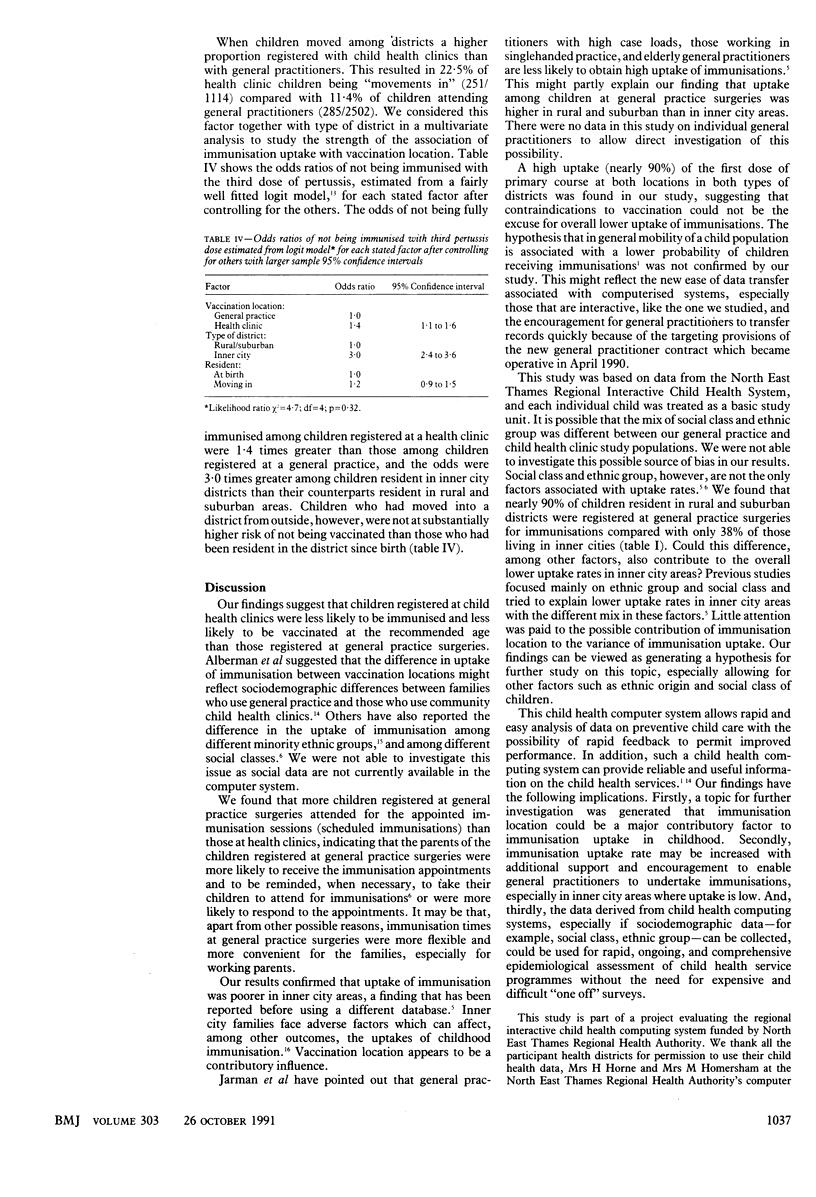
OBJECTIVE--To compare immunisation uptake rates in general practice surgeries and community child health clinics. DESIGN--Cohort study using data from a computerised child health system. SETTING--Four health districts of North East Thames Regional Health Authority. SUBJECTS--3616 children born January to March 1990 and resident in the four districts at the end of January 1991. MAIN OUTCOME MEASURES--Immunisation uptake rates at 10-12 months of age, age at immunisation, scheduling performance at the two locations, and odds ratios of outstanding immunisations. RESULTS--80% of children registered at general practices had completed their third dose of pertussis immunisation compared with 68% of those at health clinics. Median ages at the third dose were 24 weeks and 29 weeks at the two locations respectively. Scheduling was more effective at general practice surgeries. Unscheduled immunisations were more likely to be given after the recommended age. Overall, children resident in rural and suburban areas had greater uptakes than those in inner cities. Odds ratios for not being fully immunised among children registered at health clinics were 1.4 times those among children immunised in general practice and 3.0 times greater among children resident in inner cities than among those in rural and suburban districts. Children who moved into a district, however, were no less likely to be fully immunised than children who were born there. CONCLUSIONS--The immunisation uptake rate was better in general practices than in child health clinics in both inner city and rural and suburban areas. Uptake may be increased with additional support to enable general practitioners to undertake immunisations, especially in inner cities.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Alberman E., Watson E., Mitchell P., Day S. The development of performance and cost indicators for preschool immunisation. Arch Dis Child. 1986 Mar;61(3):251–256. doi: 10.1136/adc.61.3.251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker M. R., Bandaranayake R., Schweiger M. S. Differences in rate of uptake of immunisation among ethnic groups. Br Med J (Clin Res Ed) 1984 Apr 7;288(6423):1075–1078. doi: 10.1136/bmj.288.6423.1075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Begg N. T., Noah N. D. Immunisation targets in Europe and Britain. Br Med J (Clin Res Ed) 1985 Nov 16;291(6506):1370–1371. doi: 10.1136/bmj.291.6506.1370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- FOLEY J. F., GRAVELLE C. R., ENGLEHARD W. E., CHIN T. D. Achromobacter septicemia-fatalities in prematures. I. Clinical and epidemiological study. Am J Dis Child. 1961 Mar;101:279–288. [PubMed] [Google Scholar]
- Nicoll A., Elliman D., Begg N. T. Immunisation: causes of failure and strategies and tactics for success. BMJ. 1989 Sep 30;299(6703):808–812. doi: 10.1136/bmj.299.6703.808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riley D. J., Mughal M. Z., Roland J. Immunisation state of young children admitted to hospital and effectiveness of a ward based opportunistic immunisation policy. BMJ. 1991 Jan 5;302(6767):31–33. doi: 10.1136/bmj.302.6767.31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roper J., Day S. Uptake of immunisations in low birthweight infants. Arch Dis Child. 1988 May;63(5):518–521. doi: 10.1136/adc.63.5.518. [DOI] [PMC free article] [PubMed] [Google Scholar]


