The diagnosis of acute rheumatic fever is a clinical challenge and depends on the possibility of the disease being borne in mind. Although the complete eradication of rheumatic fever from the Western world has not been achieved, the disease is often forgotten in the differential diagnosis of a patient with fever and polyarthralgia or arthritis. Rheumatic fever remains an important acquired cardiac disease in low and middle income countries and among poorly resourced communities in high income countries. Rheumatic heart disease places a heavy economic burden on the healthcare system in low and middle income countries because of the costs of medical treatment and heart valve surgery and also because it is a disease of young adults, who are the most economically active group of any population. Management is complex and involves different levels of care. The only new advances in the management of acute rheumatic fever to date are in the development of vaccines.
Summary points
Rheumatic heart disease is a major cause of morbidity and mortality in low and middle income countries and among underprivileged communities in high income countries
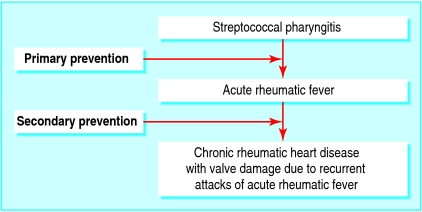
Primary prevention of acute rheumatic fever requires adequate antibiotic treatment of streptococcal throat infections
Secondary prevention entails prevention of recurrent episodes of acute rheumatic fever and is the most effective way of preventing rheumatic heart disease
Corticosteroids do not reduce the risk of developing heart valve lesions after one year
Surgery may be a life saving measure in patients with acute rheumatic fever and major valve lesions
Sources and search criteria
Modern management strategies for rheumatic fever were sourced from PubMed publications, 2000-6
Search terms included “acute rheumatic fever”, “rheumatic heart disease”, “management”, and “treatment”
Systematic Cochrane reviews provided the evidence for primary and secondary prophylaxis and anti-inflammatory treatment of acute carditis in patients with acute rheumatic fever
Additional references were identified through reviewed articles
What populations are at risk?
Acute rheumatic fever remains highly prevalent in developing countries, where overcrowding and poor access to health care persist. The true incidence of acute rheumatic fever and prevalence of rheumatic heart disease in these areas is not known because relevant epidemiological data are not available. The highest incidence of acute rheumatic fever published in recent times is among the indigenous populations of Australia and New Zealand. The estimated annual number of cases in young people aged 5-14 years is 374 per 100 000 population. Around 60% of these patients develop rheumatic heart disease.1 In contrast, in high income countries the incidence has dropped to fewer than 1 per 100 000 population.2 The highest calculated regional prevalence of rheumatic heart disease among schoolchildren is in sub-Saharan Africa (5.7 cases per 1000), the Pacific and indigenous populations of Australia and New Zealand (3.5 cases per 1000), and south central Asia (2.2 cases per 1000).1
What is the pathogenesis?
Although it is well established that a group A β haemolytic streptococcus is the agent leading to acute rheumatic fever, the pathogenesis and immune mechanisms are still not completely understood. The clinical manifestation of the response and its severity in an individual is determined by host susceptibility, the virulence of the infecting organism, and a conducive environment. Briefly, it seems that a combined humoral and cell mediated immune response occurs to the bacterium's antigens, which cross reacts with human tissue, such as cardiac tissue, joints, skin, and the central nervous system, through molecular mimicry.3 w1 w2
Only certain strains of the group A streptococcus have been associated with acute rheumatic fever. This potential to rheumatogenicity was thought to be determined by the M protein or antiphagocytic component of the bacterium's cell wall. The classic rheumatogenic M serotype hypothesis has been disputed by the discovery of other serotypes in communities where rheumatic fever and rheumatic heart disease are common.4 w3
The noticeably decreased incidence of acute rheumatic fever in the United States over the past 50 years is correlated with the replacement of rheumatogenic types by non-rheumatogenic types in cases of streptococcal pharyngitis in children. The reasons underlying the observed change in distribution of M types and virulence of the group A streptococcus needs elucidation.5 The resurgence of rheumatic fever during the mid-1980s in the intermountain area of Salt Lake City, Utah was believed to be associated with an increased number of mucoid strains of Streptococcus pyogenes M type 18 within the community.6 Only a few people (0.3-3%) with acute streptococcal pharyngitis develop acute rheumatic fever.2 A genetic predisposition is certain. The presence of HLA class II alleles and haplotypes in some people has been associated with risk or protection from rheumatic heart disease, and these associations have been more evident in patients with mitral valve disease.7
A new emerging hypothesis is that group A streptococcal pyoderma rather than pharyngitis may be responsible for the development of acute rheumatic fever in some communities. Colonisation of the throat with group A streptococci among certain groups with a high incidence of acute rheumatic fever, such as Aborigines, is rare. Instead, streptococcal pyoderma is the main manifestation of group A streptococci.8 If confirmed this relation has important implications for the primary prevention of acute rheumatic fever and the development of a vaccine.
How is acute rheumatic fever diagnosed?
The modified Jones criteria are commonly used to diagnose the initial attack of acute rheumatic fever (box).9 The probability of acute rheumatic fever is high when there is evidence of a preceding streptococcal infection, usually measured by an increase in the antistreptolysin O titre together with two major manifestations or one major and two minor manifestations. Permanent damage to heart valves may result from recurrences of rheumatic fever. The other major manifestations are transient and do not lead to permanent damage but are important in the diagnosis.2 The differential diagnosis of acute rheumatic fever should include diseases with similar clinical manifestations such as septic arthritis, connective tissue diseases, Lyme disease, sickle cell anaemia, infective endocarditis, leukaemia, and lymphoma.2
Modified Jones criteria for diagnosis of acute rheumatic fever, updated 1992
Major criteria
Carditis
Polyarthritis
Subcutaneous nodules
Erythema marginatum
Chorea
Minor criteria
Prolonged PR interval on electrocardiogram
Arthralgia
Fever
Acute phase reactants: raised erythrocyte sedimentation rate or raised C reactive protein levels
Plus supporting evidence of a preceding streptococcal infection for both major and minor criteria
The 2002-3 criteria from the World Health Organization (table 1) allow for the diagnosis of recurrent acute rheumatic fever in patients with established rheumatic heart disease and chronic rheumatic heart disease.2
Table 1.
Summary of 2002-3 World Health Organization criteria for diagnosis of rheumatic fever and rheumatic heart disease (based on revised Jones criteria)
| Diagnostic categories | Criteria |
|---|---|
| Primary episode of rheumatic fever | Two major or one major and two minor manifestations plus evidence of a preceding group A streptococcal infection |
| Recurrent attack of rheumatic fever in patients without established rheumatic heart disease | Two major or one major and two minor manifestations plus evidence of a preceding group A streptococcal infection |
| Recurrent attack of rheumatic fever in patients with established rheumatic heart disease | Two minor manifestations plus evidence of a preceding group A streptococcal infection |
| Rheumatic chorea. Insidious onset rheumatic carditis | Other major manifestations or evidence of group A streptococcal infection not required |
| Chronic valve lesions of rheumatic heart disease (patients presenting for first time with pure mitral stenosis, mixed mitral valve disease, and aortic valve disease) | Do not require any other criteria to be diagnosed as having rheumatic heart disease |
How does echocardiography help?
Echocardiography supports the diagnosis of acute rheumatic fever, allowing the identification of important valve lesions and exclusion of non-rheumatic causes of valvular involvement.2 Typical valvular lesions such as valve leaflet and chordal thickening, leaflet shortening, mitral annular dilation, leaflet prolapse, coaptation failure, and chordal elongation are easily identified.10 Echocardiography is essential for determining the timing of surgery in patients with chronic rheumatic heart disease. For example, surgery is recommended in adults with severe mitral incompetence if they have symptoms or if they have a reduced left ventricular function or a left ventricular end systolic diameter of 40 mm or greater.11 Similar measurements for children have not been established.
What medical treatments are available?
Few new treatments are available for acute rheumatic fever. The evidence for some well established treatments for acute rheumatic fever (for example, aspirin and corticosteroids) originates from poorly designed randomised controlled trials carried out more than 40 years ago before the advent of echocardiography and which tested corticosteroids not commonly used today, such as intramuscular cortisone and corticotrophin. A recent Cochrane review based on these studies identified no significant difference in the risk of cardiac disease at one year in groups treated with corticosteroids or with aspirin.12 Similarly the use of prednisone or intravenous immunoglobulins compared with placebo failed to reduce the risk of heart valve lesions at one year. The use of corticosteroids to treat acute cardiac decompensation in patients with acute rheumatic fever is anecdotal and is not based on objective evidence.
Data on the successful use of other non-steroidal anti-inflammatory agents such as naproxen13 and high dose methylprednisone14 to treat the acute inflammatory process in patients with rheumatic fever have been published, but none has been the subject of randomised controlled trials.
Widely practised concomitant treatments such as bed rest and penicillin during the acute attack have also not been adequately studied. The benefits of giving oral penicillin to eradicate group A streptococci from the pharynx of patients with acute rheumatic fever is largely based on anecdotal evidence. It has not been shown in controlled studies to change the outcome one year after the primary event.15 w4 Bed rest to control rheumatic activity was first prescribed in the 1940s but has not been adequately scrutinised since.16 Common clinical practice is that physical activity should be restricted until the acute phase reactants have normalised and then begun gradually.w5
Does valve surgery have a role?
Occasionally, costly open heart surgery may be the only option to manage severe heart valve lesions that occur in patients with rheumatic heart disease. The timing of valve surgery is significant because the presence of active rheumatic carditis at the time of surgery is an important predictor of valve failure and the need for reoperation.17
Several studies have shown that valvular regurgitation and not myocarditis is the cause of heart failure in patients with active rheumatic carditis. Although aggressive medical therapy may provide temporary improvement, surgical treatment of severe valve lesions in patients with acute carditis and heart failure may be a lifesaving measure.16 w6 w7 Valve replacement under these circumstances may be the preferred surgical option.
Repair of a damaged valve is the procedure of choice overall because it avoids the risk of many of the complications of prosthetic valves, including thromboemboli, bleeding, and teratogenic events associated with warfarin administration, and also the poor durability of bioprosthetic valves in younger patients.w5 All patients undergoing surgery require secondary prophylaxis.
Do preventive measures work?
Primary prevention
Apart from eradicating poverty and overcrowding and improving access to medical care the only way to prevent first attacks of rheumatic fever is to treat the preceding episode of group A streptococcal pharyngitis or infection (figure). A recent systematic review concluded that giving antibiotics to patients with sore throats and symptoms suggestive of a streptococcal infection (pharyngeal exudates and enlarged tender cervical lymph nodes) reduced the risk of rheumatic fever by 70%. Intramuscular penicillin reduced the risk further, to 80%.18 Although oral penicillin for 10 days has been shown to eradicate group A streptococcus from the upper respiratory tract,19 few trials have tested the efficacy of oral penicillin in preventing rheumatic fever. The same applies to oral cephalosporins and macrolides, where there is little evidence to show protection against rheumatic fever, although clinical trials have shown that they are effective in the treatment of streptococcal pharyngitis.20 w8 w9 The possibility of resistance to erythromycin should be borne in mind, which is prevalent in some countries and has resulted in treatment failures.w10 w11 Despite concerted efforts to promote community based diagnosis of sore throat and antibiotic treatment, some trials have shown that such programmes may not effectively reduce the incidence of acute rheumatic fever within these communities.21 Until other tested strategies have been developed, such as cost effective vaccines, and other hypothesised associated causes of acute rheumatic fever are proved (for example, skin infections associated with group A streptococci), treating sore throats with antibiotics to prevent rheumatic fever should continue.w4 Therefore in communities where acute rheumatic fever is common all young people aged 5-15 years with a sore throat should be considered to have a streptococcal infection and be treated with an antibiotic (table 2).2 Microbiological confirmation is often difficult in under-resourced settings but should be carried out if laboratory services are available.2 w4
Prevention of acute rheumatic fever and rheumatic heart disease
Table 2.
Antibiotics used in primary prevention and treatment of group A streptococcal throat infection (World Health Organization guidelines)
| Antibiotic | Route of administration and dosage | Dose |
|---|---|---|
| Benzathine benzylpenicillin | Intramuscular injection; childen should be kept under observation for 30 minutes | Single dose 1.2 million U; <27 kg, 600 000 U |
| Phenoxymethylpenicillin (penicillin V) | Oral, 2-4 times daily for 10 days | Children 250 mg twice or three times daily, adolescents or adults 250 mg three or four times daily or 500 mg twice daily |
| Amoxicillin | Oral, 2-3 times daily for 10 days | 25-50 mg/kg/d in three doses; total adult dose 750-1500 mg/d |
| First generation cephalosporins | Oral, 2-3 times daily for 10 days | Varies with formulation |
| Erythromycin if allergic to penicillin | Oral, 4 times daily for 10 days | Varies with formulation |
Secondary prevention
Prevention of recurrent attacks of rheumatic fever is the most cost effective way of preventing rheumatic heart disease (figure).2 w4 Penicillin remains the antibiotic of choice. Intramuscular penicillin is preferred as it is more effective than oral penicillin and results in better compliance. A recent Cochrane meta-analysis confirmed that injections every two or three weeks were more effective than injections every four weeks. The evidence, however, is based on poor quality trials.22 Prospective data from New Zealand showed that few, if any, recurrences occurred among patients who adhered to a regimen of every four weeks.23 The study concluded that injections every four weeks can be prescribed for most patients, and injections every three weeks are recommended in a few highly motivated patients who have severe cardiac lesions and have shown good compliance with the four weekly injections.23 w4 Table 3 shows WHO guidelines for secondary prevention. WHO recommendations for the duration of secondary prophylaxis are for at least five years after a diagnosis of acute rheumatic fever or until the age of 18 years without proved carditis, for 10 years in a patient with mild mitral regurgitation or until 25 years of age, and lifelong for severe valve disease and after valve surgery.2
Table 3.
Antibiotics used in secondary prevention of rheumatic fever (World Health Organization guidelines)
| Antibiotic | Route of administration | Dose |
|---|---|---|
| Benzathine benzylpenicillin | Intramuscular injection, every 3-4 weeks | ≥30 kg, 1.2 million U; <30 kg, 600 000 U |
| Phenoxymethyl penicillin (penicillin V) | Oral | 250 mg twice daily |
| Erythromycin if allergic to penicillin | Oral | 250 mg twice daily |
Future developments
The occurrence of numerous M protein serotypes that are rheumatogenic has complicated the development of vaccines, and research is ongoing. Vaccines such as the 26 valent type specific one are already in phase II human trials,24 and the C region M protein peptide vaccine, which is almost ready for trials in humans, may offer some hope for protection against streptococcal pharyngitis in the future.25 A more recent study in animals showed that giving antisurface bound C5a peptidase serum by the intranasal route protected mice against streptococcal infection. Its use in humans may prevent colonisation and infection of the human pharynx, thereby eliminating potential reservoirs that maintain endemic disease.w12
Do public health measures make a difference?
Appropriate public health control programmes and optimal medical care do reduce the burden of acute rheumatic fever.2 The implementation of a comprehensive prevention plan for the control of acute rheumatic fever and rheumatic heart disease in Africa, such as the proposed awareness surveillance advocacy prevention (ASAP) initiative, is essential in the control of acute rheumatic fever and rheumatic heart disease. The initiative is based on several established preventive programme models from other countries.26 Awareness entails education about rheumatic fever and rheumatic heart disease among critical community members such as teachers and healthcare workers. Surveillance involves the collection of epidemiological data to identify groups of people at risk and therefore appropriately direct and concentrate control efforts. Advocacy is needed to bring into the public spotlight the devastating effects of rheumatic fever and rheumatic heart disease on the health of children. The final phase of the programme is the reinforcement of primary and secondary prevention strategies within these communities. The implementation of the programme needs the input and endorsement of health departments and other key stakeholders such as nurses, doctors, microbiologists, and epidemiologists.
Additional educational resources
Del Mar CB, Glasziou PP, Spinks AB. Antibiotics for sore throat. Cochrane Database Syst Rev 2004;(2):CD000023
World Heart Federation (www.worldheart.org)—contains resources related to training materials and has generic downloadable registers for rheumatic heart disease; no registration required
The internet journal of cardiology (www.ispub.com/ostia/index.php?xmlFilePath=journals/ijc/vol2n1/rheumatic.xml)—contains general information on rheumatic fever for physicians; no registration required
Information for patients
Kids health (http://kidshealth.org.nz/index.php/ps-pagename/centralpage/pi-id/58)—provides a booklet (PDF format) on rheumatic fever for parents (published by the National Heart Foundation of New Zealand); no registration required
Some unanswered research questions
Do corticosteroids and other anti-inflammatory agents prevent or attenuate valvular damage in patients with acute rheumatic fever?
Do corticosteroids alleviate heart failure in patients with acute rheumatic fever?
Does bed rest during an episode of acute rheumatic fever reduce rheumatic carditis activity?
Does streptococcal pyoderma result in acute rheumatic fever?
Does 10 days of oral antibiotic treatment for streptococcal throat infections prevent rheumatic fever?
Supplementary Material
References
- 1.Carapetis JR, Steer AC, Mulholland EK, Weber M. The global burden of group A streptococcal diseases. Lancet Infect Dis 2005;5:685-94. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization. Rheumatic fever and rheumatic heart disease: report of a WHO expert consultation, Geneva. WHO, 29 Oct to 1 Nov, 2001. WHO Tech Rep Ser 2001;923. www.who.int/cardiovascular_diseases/resources/trs923/en/
- 3.Kaplan MH, Bolande R. Rakaita L, Blair J. Presence of bound immunoglobulins and complement in the myocardium in acute rheumatic fever. N Engl J Med 1964;271:637-45. [DOI] [PubMed] [Google Scholar]
- 4.Martin DR, Voss LM, Walker SJ, Lennon D. Acute rheumatic fever in Auckland, New Zealand: spectrum of associated group A streptococci different from expected. Pediatr Infect Dis J 1994;13:264-9. [DOI] [PubMed] [Google Scholar]
- 5.Shulman T, Stollerman G, Beall B, Dale J, Tanz RR. Temporal changes in streptococcal M protein types and the near-disappearance of acute rheumatic fever in the United States. Clin Infect Dis 2006;42:441-7. [DOI] [PubMed] [Google Scholar]
- 6.Veasy LG, Tani LY, Daly JA, Korgenski K, Miner L, Bale J, et al. Temporal association of the appearance of mucoid strains of Streptococcus pyogenes with continuing high incidence of rheumatic fever in Utah. Pediatrics 2004;113:e168-72. [DOI] [PubMed] [Google Scholar]
- 7.Guedez Y, Kotby A, El-Demellawy M, Galal A, Thomson G, Zaher S, et al. HLA class II associations with rheumatic heart disease are more evident and consistent among clinically homogenous patients. Circulation 1999;99:2784-90. [DOI] [PubMed] [Google Scholar]
- 8.McDonald M, Currie BJ, Carapetis JR. Acute rheumatic fever: a chink in the chain that links the heart to the throat? Lancet Infect Dis 2004;4:240-5. [DOI] [PubMed] [Google Scholar]
- 9.Special writing group of the committee on rheumatic fever, endocarditis, and Kawasaki disease of the council on cardiovascular disease in the young of the American Heart Association. Guidelines for the diagnosis of rheumatic fever: Jones criteria, 1992 update. JAMA 1992;268:2069-73. [PubMed] [Google Scholar]
- 10.Vasan RS, Shrivastava S, Vijayakumar M, Narang R, Lister BC, Narula J. Echocardiographic evaluation of patients with acute rheumatic fever and rheumatic carditis. Circulation 1996;94:73-82. [DOI] [PubMed] [Google Scholar]
- 11..Wisenbaugh T, Skudicky D, Sareli P. Prediction of outcome after valve replacement for rheumatic mitral regurgitation in the era of chordal preservation. Circulation 1994;89:191-7. [DOI] [PubMed] [Google Scholar]
- 12.Cilliers AM, Manyemba J, Saloojee H. Anti-inflammatory treatment for carditis in acute rheumatic fever. Cochrane Database Syst Rev 2003;(2):CD003176. [DOI] [PubMed]
- 13.Uziel Y, Hashkes PJ, Kassem E, Padeh S, Goldman R, Vollach B. The use of naproxen in the treatment of children with rheumatic fever. J Pediatr 2000;137:269-71. [DOI] [PubMed] [Google Scholar]
- 14.Herdy GVH, Pinto CA, Oliviaes MC, Carvalho EA, Tchou H, Cosendey R, et al. Rheumatic carditis treated with high doses of pulse therapy methylprednisolone. Arq Bras Cardiol 1999;72:601-6. [DOI] [PubMed] [Google Scholar]
- 15.Mortimer EA Jr, Vaisman S, Vigneau A. The effect of penicillin on acute rheumatic fever and valvular heart disease. N Engl J Med 1959;260:101-12. [DOI] [PubMed] [Google Scholar]
- 16.Barlow JB, Marcus RH, Pocock WA, Barlow CW, Essop R, Sareli P. Mechanisms and management of heart failure in active rheumatic carditis. S Afr Med J 1990;78:181-6. [PubMed] [Google Scholar]
- 17.Skoularigis J, Sinovich V, Joubert G, Sareli P. Evaluation of the long-term results of mitral valve repair in 254 young patients with rheumatic mitral regurgitation. Circulation 1994;90:167-74. [PubMed] [Google Scholar]
- 18.Robertson KA, Volmink JA, Mayosi BM. Antibiotics for the primary prevention of acute rheumatic fever: a meta-analysis. BMC Cardiovasc Disord 2005;5:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zwart S, Rovers MM, de Melker RA, Hoes AW. Penicillin for acute sore throat in children: randomized, double blind trial. BMJ 2003;327:1324-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shulman ST. Evaluation of penicillin, cephalosporins and macrolides for therapy of streptococcal pharyngitis. Pediatrics 1996;97:955-9. [PubMed] [Google Scholar]
- 21.Lennon DR. The decline of acute rheumatic fever: unrelated to sore throat management? 42nd interscience conference on antimicrobial agents and chemotherapy, San Diego, Sept 2002;G-1481.
- 22.Manyemba J, Mayosi MB. Penicillin for secondary prevention of rheumatic fever. Cochrane Database Syst Rev 2002;(3):CD002227. [DOI] [PMC free article] [PubMed]
- 23.Spinetto H. Recurrences of rheumatic fever in Auckland, 1993-1999 [dissertation for Master of Health Sciences]. Auckland, New Zealand: University of Auckland, 2003.
- 24.Olive C, Ho M-F, Dyer J, Lincoln D, Barozzi N, Toth I, et al. Immunization with a tetraepitipic lipid core peptide vaccine construct induces broadly protective immune reponses against group A streptococcus. J Infect Dis 2006;193:1666-76. [DOI] [PubMed] [Google Scholar]
- 25.McNeil SA, Halperin SA, Langley JM, Smith B, Warren A, Sharratt GP, et al. Safety and immunogenicity of 26-valent group A streptococcus vaccine in healthy adult volunteers. Clin Infect Dis 2005;41:1114-22. [DOI] [PubMed] [Google Scholar]
- 26.Robertson KA, Volmink JA, Mayosi BM. Towards a uniform plan for the control of rheumatic fever and rheumatic heart disease in Africa—the Awareness Surveillance Advocacy Prevention (A.S.A.P.) Programme. S Afr Med J 2006;96:242-5. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.