Abstract
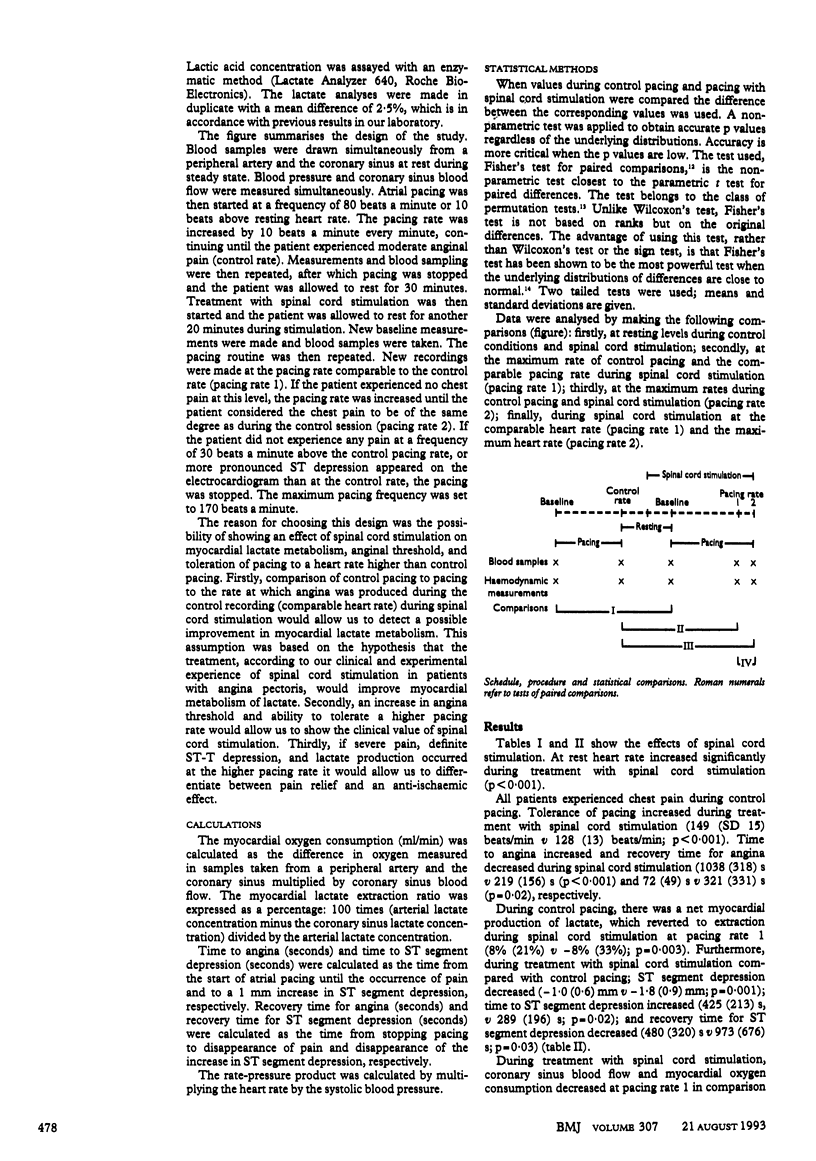
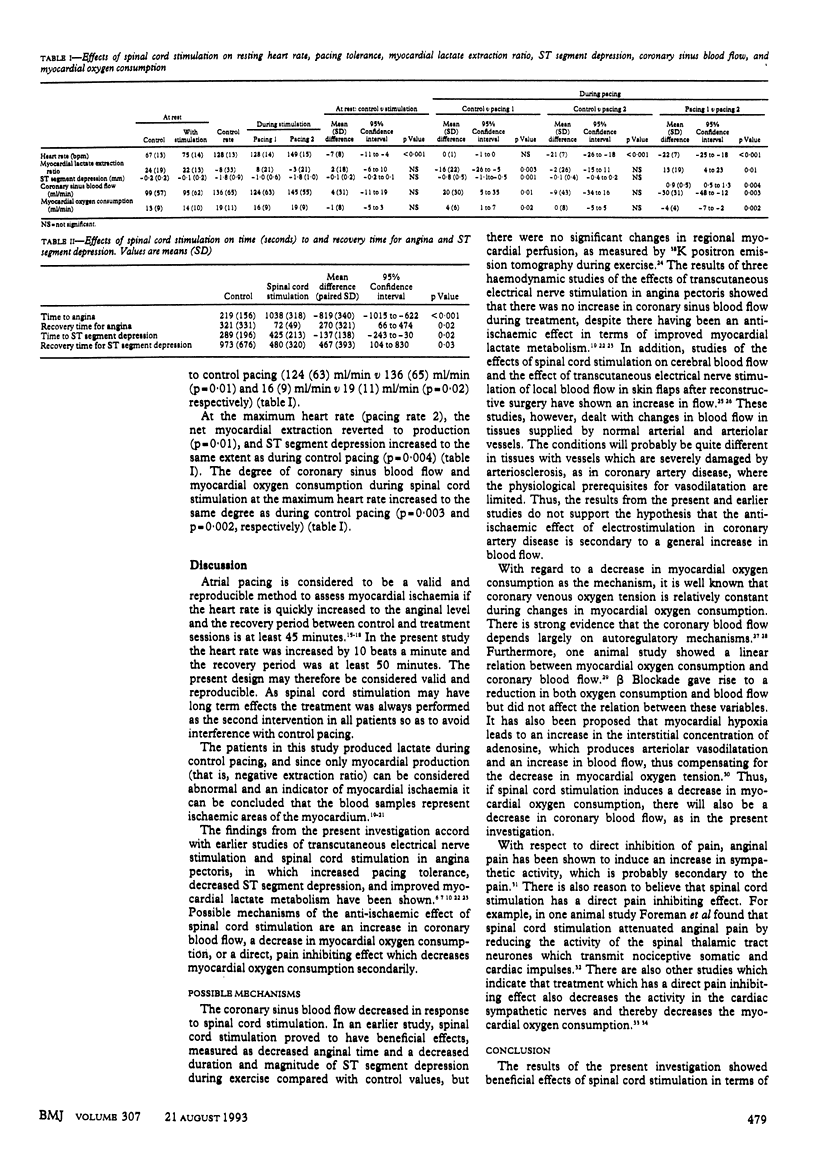
OBJECTIVE--To investigate the effects of spinal cord stimulation on myocardial ischaemia, coronary blood flow, and myocardial oxygen consumption in angina pectoris induced by atrial pacing. DESIGN--The heart was paced to angina during a control phase and treatment with spinal cord stimulation. Blood samples were drawn from a peripheral artery and the coronary sinus. SETTING--Multidisciplinary pain centre, department of medicine, Ostra Hospital, and Wallenberg Research Laboratory, Sahlgrenska Hospital, Gothenburg, Sweden. SUBJECTS--Twenty patients with intractable angina pectoris, all with a spinal cord stimulator implanted before the study. RESULTS--Spinal cord stimulation increased patients' tolerance to pacing (p < 0.001). At the pacing rate comparable to that producing angina during the control recording, myocardial lactate production during control session turned into extraction (p = 0.003) and, on the electrocardiogram, ST segment depression decreased, time to ST depression increased, and time to recovery from ST depression decreased (p = 0.01; p < 0.05, and p < 0.05, respectively). Spinal cord stimulation also reduced coronary sinus blood flow (p = 0.01) and myocardial oxygen consumption (p = 0.02). At the maximum pacing rate during treatment, all patients experienced anginal pain. Myocardial lactate extraction reverted to production (p < 0.01) and the magnitude and duration of ST segment depression increased to the same values as during control pacing, indicating that myocardial ischaemia during treatment with spinal cord stimulation gives rise to anginal pain. CONCLUSIONS--Spinal cord stimulation has an anti-anginal and anti-ischaemic effect in severe coronary artery disease. These effects seem to be secondary to a decrease in myocardial oxygen consumption. Furthermore, myocardial ischemia during treatment gives rise to anginal pain. Thus, spinal cord stimulation does not deprive the patient of a warning signal.
Full text
PDF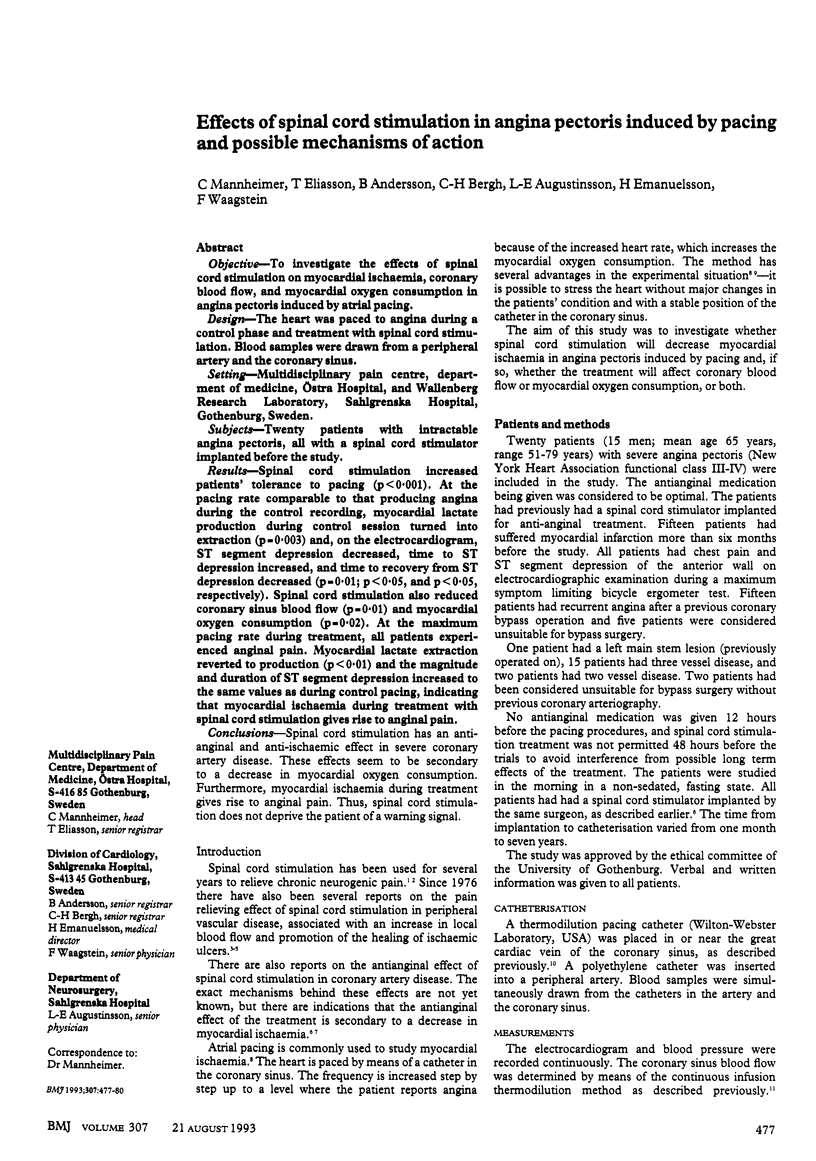

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Augustinsson L. E., Carlsson C. A., Holm J., Jivegård L. Epidural electrical stimulation in severe limb ischemia. Pain relief, increased blood flow, and a possible limb-saving effect. Ann Surg. 1985 Jul;202(1):104–110. doi: 10.1097/00000658-198507000-00017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blomberg S., Curelaru I., Emanuelsson H., Herlitz J., Pontén J., Ricksten S. E. Thoracic epidural anaesthesia in patients with unstable angina pectoris. Eur Heart J. 1989 May;10(5):437–444. doi: 10.1093/oxfordjournals.eurheartj.a059507. [DOI] [PubMed] [Google Scholar]
- Chandler M. J., Brennan T. J., Garrison D. W., Kim K. S., Schwartz P. J., Foreman R. D. A mechanism of cardiac pain suppression by spinal cord stimulation: implications for patients with angina pectoris. Eur Heart J. 1993 Jan;14(1):96–105. doi: 10.1093/eurheartj/14.1.96. [DOI] [PubMed] [Google Scholar]
- Cohen L. S., Elliott W. C., Klein M. D., Gorlin R. Coronary heart disease. Clinical, cinearteriographic and metabolic correlations. Am J Cardiol. 1966 Feb;17(2):153–168. doi: 10.1016/0002-9149(66)90347-x. [DOI] [PubMed] [Google Scholar]
- Cook A. W., Oygar A., Baggenstos P., Pacheco S., Kleriga E. Vascular disease of extremities. Electric stimulation of spinal cord and posterior roots. N Y State J Med. 1976 Mar;76(3):366–368. [PubMed] [Google Scholar]
- Emanuelsson H., Mannheimer C., Waagstein F., Wilhelmsson C. Catecholamine metabolism during pacing-induced angina pectoris and the effect of transcutaneous electrical nerve stimulation. Am Heart J. 1987 Dec;114(6):1360–1366. doi: 10.1016/0002-8703(87)90537-0. [DOI] [PubMed] [Google Scholar]
- Feigl E. O. Coronary physiology. Physiol Rev. 1983 Jan;63(1):1–205. doi: 10.1152/physrev.1983.63.1.1. [DOI] [PubMed] [Google Scholar]
- Forrester J. S., Helfant R. H., Pasternac A., Amsterdam E. A., Most A. S., Kemp H. G., Gorlin R. Atrial pacing in coronary heart disease. Effect on hemodynamics, metabolism and coronary circulation. Am J Cardiol. 1971 Mar;27(3):237–243. doi: 10.1016/0002-9149(71)90296-7. [DOI] [PubMed] [Google Scholar]
- Ganz W., Tamura K., Marcus H. S., Donoso R., Yoshida S., Swan H. J. Measurement of coronary sinus blood flow by continuous thermodilution in man. Circulation. 1971 Aug;44(2):181–195. doi: 10.1161/01.cir.44.2.181. [DOI] [PubMed] [Google Scholar]
- Gertz E. W., Wisneski J. A., Neese R., Houser A., Korte R., Bristow J. D. Myocardial lactate extraction: multi-determined metabolic function. Circulation. 1980 Feb;61(2):256–261. doi: 10.1161/01.cir.61.2.256. [DOI] [PubMed] [Google Scholar]
- Gybels J., Kupers R. Central and peripheral electrical stimulation of the nervous system in the treatment of chronic pain. Acta Neurochir Suppl (Wien) 1987;38:64–75. doi: 10.1007/978-3-7091-6975-9_10. [DOI] [PubMed] [Google Scholar]
- Hosobuchi Y. Electrical stimulation of the cervical spinal cord increases cerebral blood flow in humans. Appl Neurophysiol. 1985;48(1-6):372–376. doi: 10.1159/000101161. [DOI] [PubMed] [Google Scholar]
- Ihlen H., Simonsen S., Vatne K. Reproducibility of ischaemic lactate metabolism during atrial pacing in man. Cardiology. 1983;70(4):177–183. doi: 10.1159/000173591. [DOI] [PubMed] [Google Scholar]
- Jackson G., Atkinson L., Oram S. Improvement of myocardial metabolism in coronary arterial disease by beta-blockade. Br Heart J. 1977 Aug;39(8):829–833. doi: 10.1136/hrt.39.8.829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobs M. J., Jörning P. J., Beckers R. C., Ubbink D. T., van Kleef M., Slaaf D. W., Reneman R. S. Foot salvage and improvement of microvascular blood flow as a result of epidural spinal cord electrical stimulation. J Vasc Surg. 1990 Sep;12(3):354–360. [PubMed] [Google Scholar]
- Knabb R. M., Ely S. W., Bacchus A. N., Rubio R., Berne R. M. Consistent parallel relationships among myocardial oxygen consumption, coronary blood flow, and pericardial infusate adenosine concentration with various interventions and beta-blockade in the dog. Circ Res. 1983 Jul;53(1):33–41. doi: 10.1161/01.res.53.1.33. [DOI] [PubMed] [Google Scholar]
- Kröger K., Schipke J., Thämer V., Heusch G. Poststenotic ischaemic myocardial dysfunction induced by peripheral nociceptive stimulation. Eur Heart J. 1989 Nov;10 (Suppl F):179–182. doi: 10.1093/eurheartj/10.suppl_f.179. [DOI] [PubMed] [Google Scholar]
- MOSHER P., ROSS J., Jr, MCFATE P. A., SHAW R. F. CONTROL OF CORONARY BLOOD FLOW BY AN AUTOREGULATORY MECHANISM. Circ Res. 1964 Mar;14:250–259. doi: 10.1161/01.res.14.3.250. [DOI] [PubMed] [Google Scholar]
- Mannheimer C., Augustinsson L. E., Carlsson C. A., Manhem K., Wilhelmsson C. Epidural spinal electrical stimulation in severe angina pectoris. Br Heart J. 1988 Jan;59(1):56–61. doi: 10.1136/hrt.59.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mannheimer C., Carlsson C. A., Emanuelsson H., Vedin A., Waagstein F., Wilhelmsson C. The effects of transcutaneous electrical nerve stimulation in patients with severe angina pectoris. Circulation. 1985 Feb;71(2):308–316. doi: 10.1161/01.cir.71.2.308. [DOI] [PubMed] [Google Scholar]
- Mannheimer C., Emanuelsson H., Waagstein F., Wilhelmsson C. Influence of naloxone on the effects of high frequency transcutaneous electrical nerve stimulation in angina pectoris induced by atrial pacing. Br Heart J. 1989 Jul;62(1):36–42. doi: 10.1136/hrt.62.1.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller W. L., Belardinelli L., Bacchus A., Foley D. H., Rubio R., Berne R. M. Canine myocardial adenosine and lactate production, oxygen consumption, and coronary blood flow during stellate ganglia stimulation. Circ Res. 1979 Dec;45(6):708–718. doi: 10.1161/01.res.45.6.708. [DOI] [PubMed] [Google Scholar]
- Neill W. A., Kremkau E. L. Criteria for detecting ischemic myocardial hypoxia from lactate and pyruvate data during atrial pacing in humans. J Lab Clin Med. 1974 Mar;83(3):428–435. [PubMed] [Google Scholar]
- Robertson R. M., Bernard Y., Robertson D. Arterial and coronary sinus catecholamines in the course of spontaneous coronary artery spasm. Am Heart J. 1983 Jun;105(6):901–906. doi: 10.1016/0002-8703(83)90387-3. [DOI] [PubMed] [Google Scholar]
- Sanderson J. E., Brooksby P., Waterhouse D., Palmer R. B., Neubauer K. Epidural spinal electrical stimulation for severe angina: a study of its effects on symptoms, exercise tolerance and degree of ischaemia. Eur Heart J. 1992 May;13(5):628–633. doi: 10.1093/oxfordjournals.eurheartj.a060226. [DOI] [PubMed] [Google Scholar]
- Siegfried J., Lazorthes Y. Long-term follow-up of dorsal cord stimulation for chronic pain syndrome after multiple lumbar operations. Appl Neurophysiol. 1982;45(1-2):201–204. doi: 10.1159/000101599. [DOI] [PubMed] [Google Scholar]
- Sowton G. E., Balcon R., Cross D., Frick M. H. Measurement of the angina threshold using atrial pacing. A new technique for the study of angina pectoris. Cardiovasc Res. 1967 Oct;1(4):301–307. doi: 10.1093/cvr/1.4.301. [DOI] [PubMed] [Google Scholar]
- Thadani U., Lewis J. R., Mathew T. M., West R. O., Parker J. O. Reproducibility of clinical and hemodynamic parameters during pacing stress testing in patients with angina pectoris. Circulation. 1979 Nov;60(5):1036–1044. doi: 10.1161/01.cir.60.5.1036. [DOI] [PubMed] [Google Scholar]
- Zaret B. L., Wackers F. J., Terrin M. L., Ross R., Weiss M., Slater J., Morrison J., Bourge R. C., Passamani E., Knatterud G. Assessment of global and regional left ventricular performance at rest and during exercise after thrombolytic therapy for acute myocardial infarction: results of the Thrombolysis in Myocardial Infarction (TIMI) II Study. Am J Cardiol. 1992 Jan 1;69(1):1–9. doi: 10.1016/0002-9149(92)90667-n. [DOI] [PubMed] [Google Scholar]


