Abstract
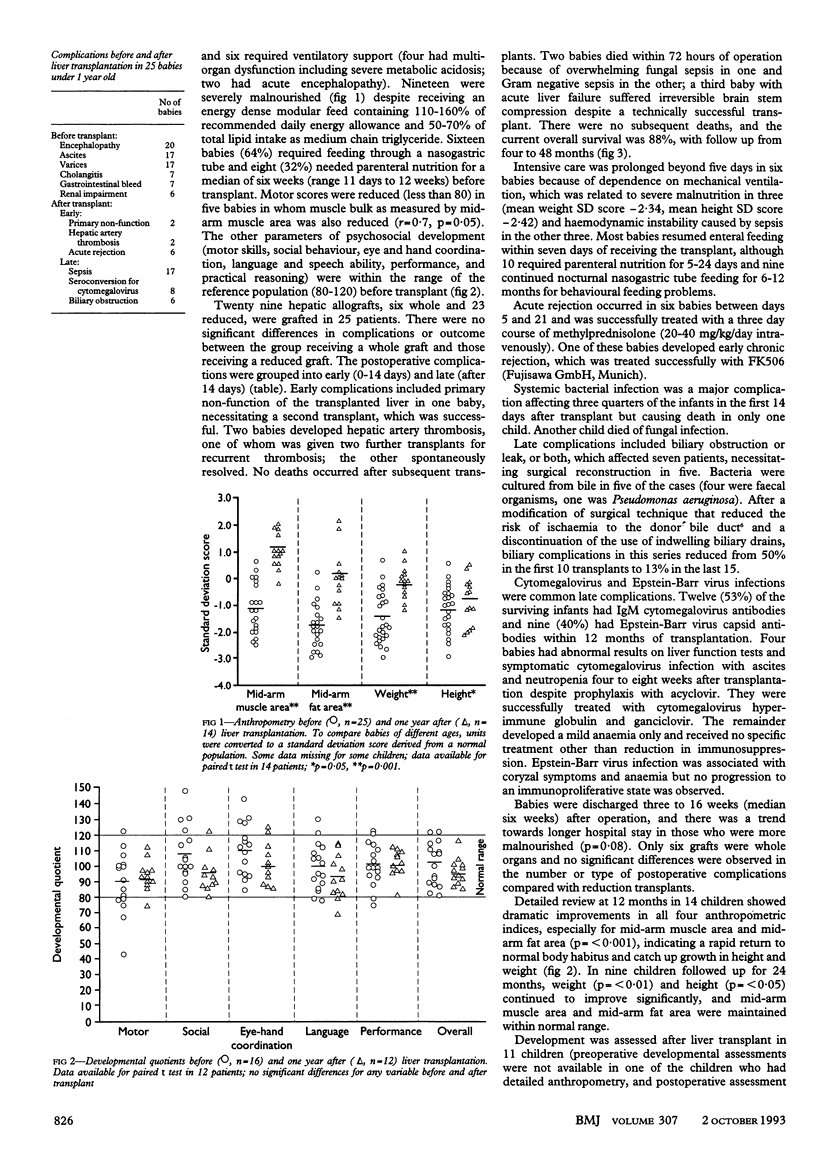
OBJECTIVE--To review the outcome of liver transplantation in babies aged less than 1 year. DESIGN--Prospective evaluation of survival, clinical complications, and nutritional and developmental status before and one year after liver transplantation. SETTING--The Children's Hospital and Queen Elizabeth Hospital, Birmingham. SUBJECTS--All 25 babies who received liver transplantation from January 1989 to December 1992 were included. Median age was 9 months and median weight was 7.0 kg. Seven babies were assessed but were not given transplants because they died while on the waiting list (two) or had severe extrahepatic disease (five). RESULTS--24 babies had severe decompensated liver disease and 20 were severely malnourished despite nutritional support. Six babies received a whole liver graft and 19 received a reduction hepatectomy. Postoperative complications included primary nonfunction of the transplanted liver (one baby), hepatic artery thrombosis (two), biliary obstruction (seven), acute and chronic rejection (six), and sepsis (18). Three babies required a second transplant; all survived. Three babies, two of whom presented with fulminant hepatic failure, died. The overall actuarial survival rate (4 months to 4 years) is 88%. Review at 12 months showed a dramatic improvement in growth (p < 0.001) and normal psychosocial development with good quality of life. CONCLUSION--The improvement in survival rates and quality of life in this group of very sick babies is related not only to the development of reduction hepatectomy but also to advances in medical and nursing expertise. Early referral for liver transplantation is justified even if babies are critically ill.
Full text
PDF


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Badger I. L., Czerniak A., Beath S., Tisone G., Deakin M., Sherlock D. J., Kelly D. A., McMaster P., Buckels J. A. Hepatic transplantation in children using reduced size allografts. Br J Surg. 1992 Jan;79(1):47–49. doi: 10.1002/bjs.1800790115. [DOI] [PubMed] [Google Scholar]
- Buckels J. A., Tisone G., Gunson B. K., McMaster P. Low haematocrit reduces hepatic artery thrombosis after liver transplantation. Transplant Proc. 1989 Feb;21(1 Pt 2):2460–2461. [PubMed] [Google Scholar]
- Chin S. E., Shepherd R. W., Cleghorn G. J., Patrick M. K., Javorsky G., Frangoulis E., Ong T. H., Balderson G., Koido Y., Matsunami H. Survival, growth and quality of life in children after orthotopic liver transplantation: a 5 year experience. J Paediatr Child Health. 1991 Dec;27(6):380–385. doi: 10.1111/j.1440-1754.1991.tb00424.x. [DOI] [PubMed] [Google Scholar]
- Chiyende J., Mowat A. P. Liver transplantation. Arch Dis Child. 1992 Sep;67(9):1124–1127. doi: 10.1136/adc.67.9.1124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esquivel C. O., Koneru B., Karrer F., Todo S., Iwatsuki S., Gordon R. D., Makowka L., Marsh W. J., Jr, Starzl T. E. Liver transplantation before 1 year of age. J Pediatr. 1987 Apr;110(4):545–548. doi: 10.1016/s0022-3476(87)80545-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frisancho A. R. New norms of upper limb fat and muscle areas for assessment of nutritional status. Am J Clin Nutr. 1981 Nov;34(11):2540–2545. doi: 10.1093/ajcn/34.11.2540. [DOI] [PubMed] [Google Scholar]
- Houssin D., Soubrane O., Boillot O., Dousset B., Ozier Y., Devictor D., Bernard O., Chapuis Y. Orthotopic liver transplantation with a reduced-size graft: an ideal compromise in pediatrics? Surgery. 1992 May;111(5):532–542. [PubMed] [Google Scholar]
- Kalayoglu M., Stratta R. J., Sollinger H. W., Hoffmann R. M., D'Alessandro A. M., Pirsch J. D., Belzer F. O. Liver transplantation in infants and children. J Pediatr Surg. 1989 Jan;24(1):70–76. doi: 10.1016/s0022-3468(89)80305-7. [DOI] [PubMed] [Google Scholar]
- Kaufman S. S., Murray N. D., Wood R. P., Shaw B. W., Jr, Vanderhoof J. A. Nutritional support for the infant with extrahepatic biliary atresia. J Pediatr. 1987 May;110(5):679–686. doi: 10.1016/s0022-3476(87)80002-1. [DOI] [PubMed] [Google Scholar]
- Lynch S. V., Akiyama T., Ong T. H., Pillay S. P., Balderson G. A., Matsunami H., Shepherd R. W., Cleghorn G. J., Patrick M. K., Strong R. W. Transplantation in children with biliary atresia. Transplant Proc. 1992 Feb;24(1):186–188. [PubMed] [Google Scholar]
- Malatack J. J., Schaid D. J., Urbach A. H., Gartner J. C., Jr, Zitelli B. J., Rockette H., Fischer J., Starzl T. E., Iwatsuki S., Shaw B. W. Choosing a pediatric recipient for orthotopic liver transplantation. J Pediatr. 1987 Oct;111(4):479–489. doi: 10.1016/s0022-3476(87)80105-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miyawaki T., Moriya N., Nagaoki T., Taniguchi N. Maturation of B-cell differentiation ability and T-cell regulatory function in infancy and childhood. Immunol Rev. 1981;57:61–87. doi: 10.1111/j.1600-065x.1981.tb00442.x. [DOI] [PubMed] [Google Scholar]
- Moukarzel A. A., Najm I., Vargas J., McDiarmid S. V., Busuttil R. W., Ament M. E. Effect of nutritional status on outcome of orthotopic liver transplantation in pediatric patients. Transplant Proc. 1990 Aug;22(4):1560–1563. [PubMed] [Google Scholar]
- Otte J. B., de Ville de Goyet J., Sokal E., Alberti D., Moulin D., de Hemptinne B., Veyckemans F., van Obbergh L., Carlier M., Clapuyt P. Size reduction of the donor liver is a safe way to alleviate the shortage of size-matched organs in pediatric liver transplantation. Ann Surg. 1990 Feb;211(2):146–157. doi: 10.1097/00000658-199002000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryckman F. C., Flake A. W., Fisher R. A., Tchervenkov J. I., Pedersen S. H., Balistreri W. F. Segmental orthotopic hepatic transplantation as a means to improve patient survival and diminish waiting-list mortality. J Pediatr Surg. 1991 Apr;26(4):422–428. doi: 10.1016/0022-3468(91)90989-7. [DOI] [PubMed] [Google Scholar]
- Salt A., Noble-Jamieson G., Barnes N. D., Mowat A. P., Rolles K., Jamieson N., Johnston P., Friend P., Calne R. Y. Liver transplantation in 100 children: Cambridge and King's College Hospital series. BMJ. 1992 Feb 15;304(6824):416–421. doi: 10.1136/bmj.304.6824.416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sann L., Durand M., Picard J., Lasne Y., Bethenod M. Arm fat and muscle areas in infancy. Arch Dis Child. 1988 Mar;63(3):256–260. doi: 10.1136/adc.63.3.256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sokal E. M., Veyckemans F., de Ville de Goyet J., Moulin D., Van Hoorebeeck N., Alberti D., Buts J. P., Rahier J., Van Obbergh L., Clapuyt P. Liver transplantation in children less than 1 year of age. J Pediatr. 1990 Aug;117(2 Pt 1):205–210. doi: 10.1016/s0022-3476(05)80531-1. [DOI] [PubMed] [Google Scholar]
- Stewart S. M., Uauy R., Waller D. A., Kennard B. D., Benser M., Andrews W. S. Mental and motor development, social competence, and growth one year after successful pediatric liver transplantation. J Pediatr. 1989 Apr;114(4 Pt 1):574–581. doi: 10.1016/s0022-3476(89)80696-1. [DOI] [PubMed] [Google Scholar]
- Whitington P. F., Balistreri W. F. Liver transplantation in pediatrics: indications, contraindications, and pretransplant management. J Pediatr. 1991 Feb;118(2):169–177. doi: 10.1016/s0022-3476(05)80478-0. [DOI] [PubMed] [Google Scholar]


