Abstract
The authors, using a crossover design, randomly administered, in a single-blind manner, inferior alveolar nerve blocks using 36 mg of lidocaine with 18 μg of epinephrine or a combination of 36 mg of lidocaine with 18 μg epinephrine plus 36 mg meperidine with 18 μg of epinephrine, at 2 separate appointments, to 52 subjects. An electric pulp tester was used to test for anesthesia, in 4-minute cycles for 60 minutes, of the molars, premolars, and central and lateral incisors. Anesthesia was considered successful when 2 consecutive 80 readings were obtained within 15 minutes and the 80 reading was continuously sustained for 60 minutes. Using the lidocaine solution, successful pulpal anesthesia ranged from 8 to 58% from the central incisor to the second molar. Using the lidocaine/meperidine solution, successful pulpal anesthesia ranged from 0 to 17%. There was a significant difference (P < .05) between the lidocaine and lidocaine/meperidine solutions for the lateral incisors through the second molars. We conclude that the addition of meperidine to a standard lidocaine solution does not increase the success of the inferior alveolar nerve block.
Keywords: Meperidine, Inferior alveolar nerve block, Lidocaine
The inferior alveolar nerve (IAN) block is the most frequently used injection technique for achieving local anesthesia for mandibular restorative and surgical procedures. However, the IAN block does not always result in successful pulpal anesthesia.1–13 Failure rates of 7 to 75% have been reported in experimental studies.1–13 Clinical studies in endodontics14–20 have found failure with the IAN block occurring between 44 and 81% of the time. Therefore, it would be advantageous to improve the success rate of the IAN block.
Meperidine was first introduced in 1939 as an analgesic, sedative, and antispasmodic agent.21 It is also known as pethidine or Demerol. Meperidine is a phenylpiperidine derivative of the opioids.22,23 The molecular weight and pKa of meperidine are closer to lidocaine than other opioids.22
Clinically, meperidine has local anesthetic activity. A number of clinical and experimental studies24–36 have shown that meperidine induces spinal anesthesia and blocks action potentials, providing segmental and sensory blocks comparable to those provided by lidocaine. In medicine, it has been administered intrathecally,22,24,28,30,32 spinally,27,34 and as a saddle block,25 as well as locally for intravenous regional anesthesia,35 block,29 and infiltration36 for the effects of analgesia, anesthesia, or both.
The exact mechanism of meperidine's local anesthetic activity is unknown. It is possible that meperidine acts peripherally through opioid-specific receptors. However, Pang and colleagues37 found that meperidine was effective in reducing propofol injection pain, and this result was not reversible by the addition of naloxone. Jaffe and Rowe38 found that meperidine blocked conduction of myelinated and unmyelinated axons, and this was not reversed by naloxone. These 2 studies37,38 would suggest a nonopioid mechanism of local anesthetic activity. Hunter and Frank39 felt that the effect of meperidine was caused by 2 mechanisms: a nonspecific local anesthetic effect and an opiate receptor–mediated effect. Brau et al23 demonstrated that meperidine has a blocking effect on sodium channels in a similar concentration as lidocaine but does not compete for the same binding site as traditional local anesthetics.
Armstrong et al35 demonstrated an enhanced effect when meperidine was added to a local anesthetic for intravenous regional anesthesia. They found that meperidine increased the speed of onset and the extent of sensory and motor blockade and subjectively improved the quality of the block. Maurette et al34 also found a synergistic effect when meperidine was used in combination with a local anesthetic. No objective study has addressed the anesthetic efficacy of a combination lidocaine/meperidine anesthetic solution in IAN blocks.
The purpose of this prospective, randomized, single-blind, crossover study was to compare the degree of pulpal anesthesia obtained with 36 mg of lidocaine with 18 μg epinephrine with that of a combination of 36 mg of lidocaine with 18 μg epinephrine plus 36 mg meperidine with 18 μg epinephrine in IAN blocks. Additionally, we studied solution deposition pain and post-injection pain of the 2 solutions.
METHODS
Fifty-two adult subjects participated in this study. The subjects were in good health and were not taking any medications that would alter their perception of pain. The Ohio State University Human Subjects Review Committee approved the study and obtained written informed consent from each subject.
The 52 blinded subjects randomly received an IAN injection of either a lidocaine or a lidocaine/meperidine solution at 2 separate appointments spaced at least 1 week apart, in a crossover design. All subjects received IAN block injections using 1.8 mL of 36 mg of lidocaine (Xylocaine, Abbott Laboratories, North Chicago, Ill) with 18 μg epinephrine (Abbott Laboratories) or 3.6 mL of 36 mg of lidocaine with 18 μg epinephrine plus 36 mg of meperidine (Abbott Laboratories) with 18 μg epinephrine. With the crossover design, there were 104 total injections administered and each subject served as his or her own control. Fifty-two IAN injections were administered on the right side and 52 injections were administered on the left side. The same side randomly chosen for the first injection was used again for the second injection. The test teeth chosen for the experiment were the first and second molars, first and second pre-molars, and lateral and central incisors. The contralateral canine was used as the unanesthetized control to ensure that the pulp tester was operating properly and that the subject was responding appropriately during each experimental portion of the study. Clinical examinations indicated that all teeth were free of caries, large restorations, and periodontal disease; none had histories of trauma or sensitivity.
Under sterile conditions, the lidocaine and lidocaine/meperidine solutions were prepared each day of the appointment. For the lidocaine solution, 0.9 mL of solution was drawn from a vial of 4% lidocaine (40 mg/mL Xylocaine, Abbott Laboratories) using a sterile 3 mL Luer-Lok syringe (Becton Dickinson & Co, Franklin Lakes, NJ). Nine-tenths mL of sterile saline was drawn from a 10-mL vial (0.9% bacteriostatic sodium chloride, Abbott Laboratories, North Chicago, Ill) using a sterile 3-mL Luer-Lok syringe. The 2 solutions of lidocaine and saline were deposited into a sterile 5-mL Luer-Lok syringe and were mixed by inverting the syringe 10 times. Eighteen micrograms of epinephrine was withdrawn from a 1-mL ampule of 1 : 1000 epinephrine (1 mg/mL, Abbott Laboratories) using an Oxford Benchmate Pipette (Sherwood Medical, St Louis, Mo). The epinephrine was then added to the 5-mL syringe containing the lidocaine solution. The result was a solution of 36 mg of lidocaine with 18 μg epinephrine in 1.8 mL.
The combination lidocaine/meperidine solution was prepared as follows. For the lidocaine component of the solution, the same procedure was followed as outlined above. For the meperidine component of the solution, 0.72 mL of meperidine was drawn from a vial of 5% meperidine (50 mg/mL, Abbott Laboratories) using a sterile 3-mL Luer-Lok syringe. A 1.08-mL amount of sterile saline was drawn into a sterile syringe from a 10-mL vial of 0.9% bacteriostatic sodium chloride. The meperidine and saline solution were added to a sterile 5-mL Luer-Lok syringe and mixed by inverting the syringe. The lidocaine component was added to the same syringe and mixed. Eighteen micrograms of epinephrine was withdrawn from a 1-mL ampule of 1 : 1000 epinephrine using an Oxford Benchmate Pipette, and this was added to the 5 mL syringe. The result was a solution of 36 mg of lidocaine plus 36 mg of meperidine with 36 μg of epinephrine in 3.6 mL. The pH values for the lidocaine solution and for the lidocaine/meperidine solution were 6.6 and 6.5, respectively.
The 36-mg dose of meperidine was chosen because Reuben and colleagues,40 in a dose-response study of regional anesthesia, showed that the incidence of side effects was increased when the meperidine dose was above 40 mg.
Before the experiment, the 2 anesthetic solutions were randomly assigned 6-digit numbers from a random number table. Each subject was randomly assigned to 1 of the 2 solutions to determine which anesthetic solution was to be administered at each appointment. The appropriate Luer-Lok anesthetic syringes were masked with opaque labels that were labeled with the 6-digit numbers. Only the random numbers were recorded on the data collection and postinjection survey sheets, in order to blind the experiment.
At the beginning of each appointment and before any injections were given, the experimental teeth and control contralateral canine were tested 2 times with the pulp tester (Kerr, Analytic Technology Corp, Redmond, Wash) to record baseline vitality. After the tooth to be tested was isolated with cotton rolls and dried with gauze, toothpaste was applied to the probe tip, which was then placed midway between the gingival margin and the occlusal or incisal edge of the tooth. The current rate was set at 25 seconds to increase from no output (0) to the maximum output (80). The number associated with the initial sensation was recorded. Trained research personnel performed all preinjection and postinjection tests. The trained research assistants were dental or hygiene students specifically trained in conducting clinical trials.
Before the injection, each subject was informed of the pain rating for deposition of solution and shown the visual analog scale (VAS). A Heft-Parker VAS41 was used in this study (Figure 1). Immediately after the IAN injection, each subject rated the pain for solution deposition on the VAS. The VAS was a 170-mm line with various descriptive terms. The subjects placed a mark on the scale where it best described their pain level. To interpret the data, the VAS was divided into the following 4 categories. No pain corresponded to 0 mm on the scale. Mild pain was defined as greater than 0 mm and less than or equal to 54 mm. Mild pain included the descriptors of faint, weak, and mild pain. Moderate pain was defined as greater than 54 mm and less than 114 mm. Severe pain was defined as equal to or greater than 114 mm. Severe pain included the descriptors of strong, intense, and maximum possible.
Figure 1.
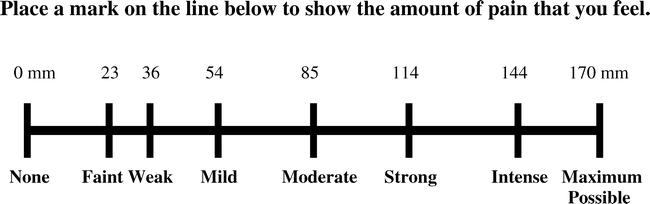
Heft-Parker visual analog scale (VAS) used for assessment of pain. The millimeter demarcations were not shown on the patients' VAS.
Topical anesthetic gel (20% benzocaine, Patterson Dental Supply, Inc, St Paul, Minn) was passively placed at the IAN injection site for 60 seconds using a cotton tip applicator. A standard IAN block42 was administered with a 27-gauge 1¼-inch needle (Monoject, Sherwood Services, Mansfield, Mass) using the appropriate 5-mL syringe equipped with an aspirating handle (Becton Dickinson & Co, Rutherford, NJ). Following initial needle penetration, the needle was advanced toward the target site over a period of 10 seconds while 0.2 mL of anesthetic solution was expressed. After gentle contact with bone, the needle was withdrawn 1 mm, aspiration was performed, and the remaining anesthetic solution was deposited over a 2-minute time period regardless of anesthetic volume. All injections were given by the senior author (A.G.).
At 1 minute after the IAN block, the first and second molars were pulp-tested. At 2 minutes, the first and second premolars were tested. At 3 minutes, the central and lateral incisors were tested. At 4 minutes, the control canine was tested. This cycle of testing was repeated every 4 minutes. At every fourth cycle the control tooth, the contralateral canine, was tested by a pulp tester without batteries to test the reliability of the subject. Each subject was asked if his or her lip/tongue was numb every minute for 5 minutes and at every fourth minute during pulp testing. If profound lip numbness was not recorded within 15 minutes, the block was considered unsuccessful; the subject was then reappointed. All testing was stopped at 60 minutes postinjection.
All subjects completed postinjection surveys after each IAN block administered. The subjects rated pain in the injection area, using the previous VAS, immediately after the numbness wore off and again each morning upon arising for 3 days. Forty-six of the 52 subjects returned completed postinjection pain rating surveys. Subjects were also instructed to describe and record any problems, other than pain, that they experienced.
No response from the subject at the maximum output (80 reading) of the pulp tester was used as the criterion for pulpal anesthesia. Anesthesia was considered successful when 2 consecutive 80 readings were obtained within 15 minutes and the 80 reading was continuously sustained for 60 minutes. That is, for most restorative procedures, we would want the patient to be numb within 15 minutes and to remain numb for 60 minutes. With a nondirectional alpha risk of .05 and a power of 80%, a sample size of 52 subjects was required to demonstrate a difference of ±25% in anesthetic success.
Comparisons between the lidocaine and lidocaine/meperidine solutions for anesthetic success was analyzed nonparametrically using exact McNemar tests. Incidences of pulpal anesthesia (percentage of 80 readings across time) between the 2 solutions were analyzed using exact McNemar tests, which were adjusted using the step-down Bonferroni method of Holm. Between–anesthetic solution differences in pain ratings for solution deposition, postinjection survey ratings, and sequelae were analyzed using Wilcoxon matched-pairs, signed-rank tests. Comparisons were considered significant at P < .05.
RESULTS
Fifty-two adult subjects, 24 women and 28 men, aged 19 to 46 years with an average age of 24 years, participated.
A total of 10 patients, 4 using the lidocaine solution and 6 using the lidocaine/meperidine solution, did not have profound lip numbness at 15 minutes (unsuccessful blocks) and were reappointed. One hundred percent of the subjects used for data analysis had profound lip anesthesia with both the lidocaine and the lidocaine/meperidine solutions.
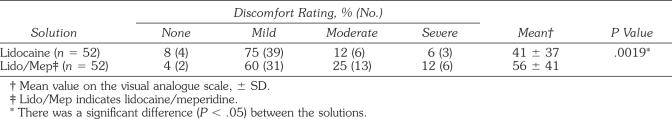
The discomfort ratings of solution deposition for the IAN blocks are presented in Table 1. There was a significant difference (P < .05) between the solutions.
Table 1.
Percentages and Discomfort Ratings of Solution Deposition
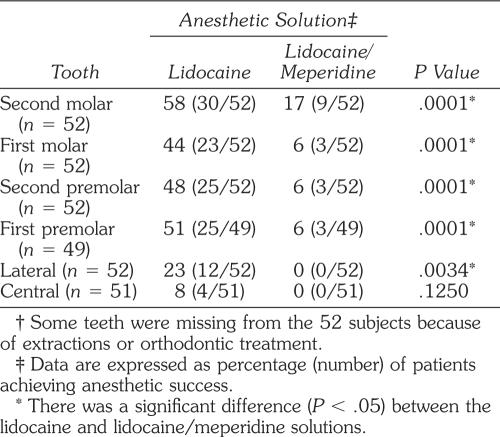
The rates of anesthetic success are presented in Table 2. For the lidocaine solution, successful pulpal anesthesia ranged from 8 to 58% from the central incisor to the second molar. Using the lidocaine/meperidine solution, successful pulpal anesthesia ranged from 0 to 17%. Except for the central incisor, the lidocaine solution had statistically higher success rates when compared to the lidocaine/meperidine solution. Figures 2 through 7 present the incidences of pulpal anesthesia (80 readings) for the 2 anesthetic solutions. There were significant differences (P < .05) between the 2 anesthetic solutions.
Table 2.
Percentages and Number of Subjects Who Experienced Anesthetic Success †
Figure 2.
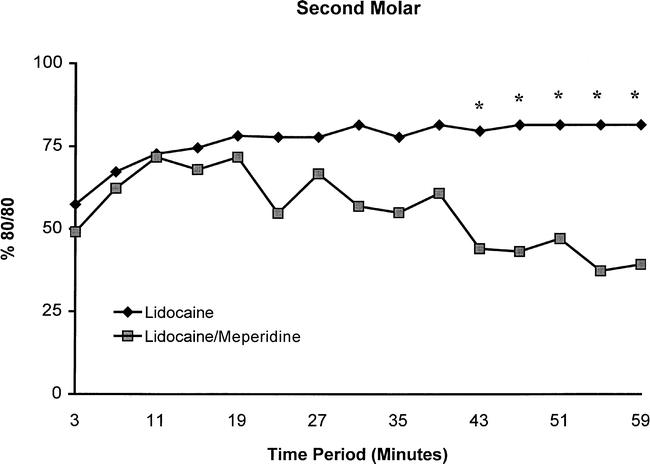
Incidence of second molar anesthesia as determined by lack of response to electrical pulp testing at the maximum setting (percentage of 80/80s) at each postinjection time interval for the lidocaine and lidocaine/meperidine solutions. Significant differences (P < .05) between the 2 anesthetic solutions are marked with an asterisk (*).
Figure 7.
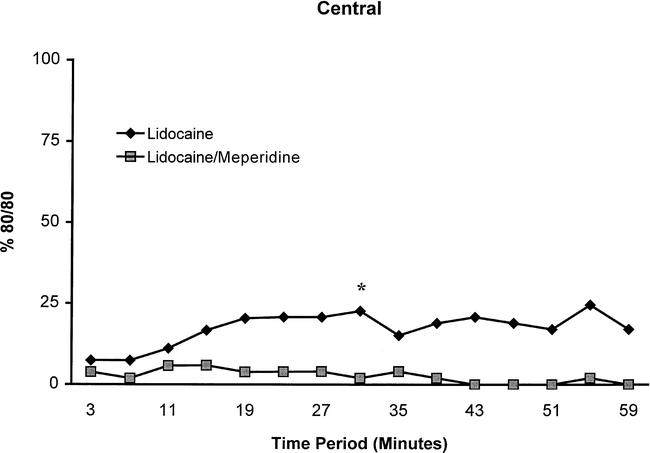
Incidence of central incisor anesthesia as determined by lack of response to electrical pulp testing at the maximum setting (percentage of 80/80s) at each postinjection time interval for the lidocaine and lidocaine/meperidine solutions. Significant differences (P < .05) between the 2 anesthetic solutions are marked with an asterisk (*).
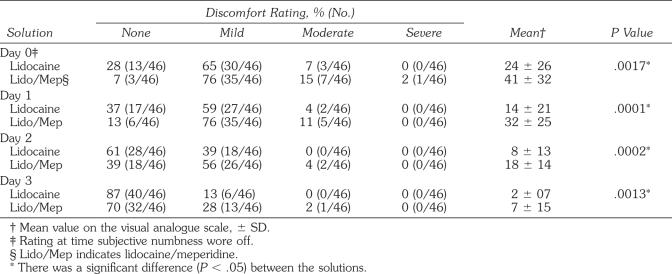
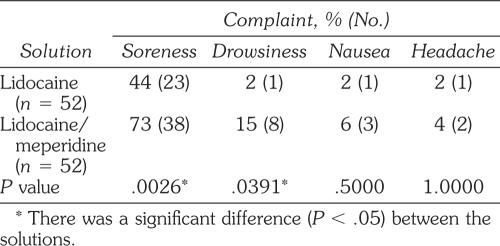
The postinjection pain ratings and subjects reporting postinjection sequelae are summarized in Tables 3 and 4. There were significant differences (P < .05) between the 2 anesthetic solutions for the day of the injection and the 3 postinjection days. The lidocaine/meperidine solution had higher mean pain ratings when compared to the lidocaine solution. Regarding postinjection sequelae, there were significant differences (P < .05) for soreness and drowsiness between the 2 anesthetic solutions.
Table 3.
Percentages and Discomfort Ratings for Postinjection Survey
Table 4.
Percentage and Number of Subjects Reporting Postinjection Sequelae
DISCUSSION
We based our use of the pulp test reading of 80—signaling maximum output—as a criterion for pulpal anesthesia on the studies of Dreven and colleagues43 and Certosimo and Archer.44 These studies43,44 showed that no patient response to an 80 reading ensured pulpal anesthesia in vital asymptomatic teeth. Additionally, Certosimo and Archer44 demonstrated that electric pulp test readings less than 80 resulted in pain during operative procedures in asymptomatic teeth. Therefore, using the electric pulp tester prior to beginning dental procedures on asymptomatic vital teeth will provide the clinician a reliable indicator of pulpal anesthesia. Because all subjects felt profound lip numbness, but pulp testing revealed that subjects did not always have pulpal anesthesia (80 readings), asking the patient if the lip is numb indicates only soft-tissue anesthesia and does not guarantee successful pulpal anesthesia.
For most teeth, anesthetic success and incidence of pulpal anesthesia (Figures 2 through 7) were significantly different between the lidocaine and lidocaine/meperidine solutions. Generally, the lidocaine solution had similar rates of anesthetic success and incidences of pulpal anesthesia to those found in other studies of the IAN block.1–13 The lidocaine solution did not provide complete pulpal anesthesia for the mandibular teeth (Figures 2 through 7) and could present meaningful clinical problems because the teeth may not be numb for procedures requiring complete pulpal anesthesia. Practitioners should consider supplemental techniques, such as intraosseous14,15,18,20 or periodontal ligament injections17 when an IAN block fails to provide pulpal anesthesia for a particular tooth. Because we studied a young adult population, the results of this study may not apply to children or the elderly.
The lidocaine/meperidine solution did not statistically improve pulpal anesthesia of the IAN block when compared to the lidocaine solution. In evaluating anesthetic success and the incidence of pulpal anesthesia (Figures 2 through 7), it can be seen that generally the duration of pulpal anesthesia begins to decrease after about 15 minutes, which accounts for a great deal of the problem with anesthetic success. Hassan and colleagues29 found that the duration of a block was significantly shortened when lidocaine was introduced into a solution of meperidine. They felt the decreased duration was caused by interaction or antagonism at drug receptors in the nerve membrane or at nonspecific binding sites. Meperidine also causes histamine release,45 which may act as a vasodilator, causing the lidocaine solution to be removed from the injection site. A portion of the decreased anesthetic efficacy with the combination lidocaine/meperidine may be because the lidocaine solution was diluted by the addition of the meperidine. In conclusion, for the concentrations used in the current study, the duration of pulpal anesthesia was shortened when meperidine was added to a lidocaine solution for the IAN block.
A third arm of the current study was to randomly and blindly give 36 mg of meperidine with 18 μg epinephrine in the IAN block. However, the initial results with meperidine alone showed that it was ineffective for pulpal anesthesia (77 to 100% failure from the second molar to central incisor), with only 3 subjects obtaining lip anesthesia, and it was discontinued after the first 15 patients. Wagner et al46 found that meperidine was less potent in phasic inhibition when compared to lidocaine. Flanagan et al47 found that meperidine had no anesthetic ability in inhibiting conduction in human peripheral nerves. They noted that the disparity between meperidine's ability to produce spinal anesthesia and its inability to produce peripheral anesthesia may be attributable to mechanisms other than inhibition of sodium channels.
Solution deposition of the lidocaine solution had an incidence of around 12% moderate pain and 6% severe pain (Table 1). Previous studies3,5,8,12 have reported a 20 to 40% incidence of moderate to severe pain with solution deposition of 36 mg of lidocaine with 18 μg of epinephrine. The ratings indicate that an IAN block has the potential to be painful even though the solution was deposited slowly over 2 minutes.
Solution deposition of the lidocaine/meperidine solution resulted in statistically higher pain ratings when compared to the lidocaine solution. Twenty-five percent of the subjects reported moderate pain and 12% reported severe pain. Even though the pH of the lidocaine/meperidine solution was similar to that of the lidocaine solution (6.5 vs 6.6), the lidocaine/meperidine resulted in higher pain ratings. Perhaps histamine release associated with meperidine may have accounted for the higher pain ratings.45
Postinjection pain ratings, at the time anesthesia wore off, were statistically lower for the lidocaine solution when compared to the lidocaine/meperidine solution (Table 3). The incidence of moderate pain was 7% with the lidocaine solution, with no reports of severe pain (Table 3). The incidence of moderate pain decreased over the next 3 days. In the current study, the incidence of moderate postinjection pain for the lidocaine solution was lower than in the study by Nist et al,8 who showed a 17% initial incidence and decreasing moderate ratings over 3 days using a lidocaine solution for the IAN block. Ridenour et al12 and Mikesell et al3 reported a 14 and 21% incidence of moderate/severe pain respectively, and decreasing pain ratings over 3 days, when also using a lidocaine solution for the IAN block. In general, we can state that the IAN block injection of lidocaine with epinephrine could result in some initial moderate postinjection pain.
The statistically higher postinjection pain ratings for the lidocaine/meperidine solution would indicate that this solution has the potential to be more irritating than a lidocaine solution. However, the decreasing moderate pain ratings over 3 days demonstrate that any initial effect does not seem long-lasting. Again, histamine release associated with meperidine may have accounted for the higher pain ratings.45
Subjects reported some postinjection sequelae (Table 4). The most common complaint was soreness, with a statistically higher incidence (73%) with the lidocaine/meperidine solution when compared to the lidocaine solution (44% incidence). Perhaps the irritating potential with the lidocaine/meperidine solution was associated with histamine release.45 There was a statistically higher incidence of drowsiness associated with the lidocaine/meperidine solution. Reuben et al40 reported side effects, including sedation and dizziness, with a similar dose of meperidine to that used in this study. Therefore, drowsiness can be a side effect of meperidine administration.
In conclusion, a solution of lidocaine/meperidine was statistically inferior to the lidocaine solution for IAN blocks. Therefore, its usefulness as an anesthetic agent would be severely limited for standard dental procedures requiring profound pulpal anesthesia.
Figure 3.
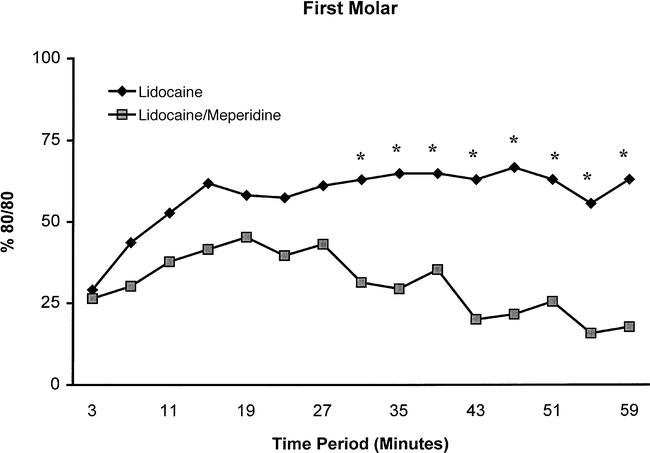
Incidence of first molar anesthesia as determined by lack of response to electrical pulp testing at the maximum setting (percentage of 80/80s) at each postinjection time interval for the lidocaine and lidocaine/meperidine solutions. Significant differences (P < .05) between the 2 anesthetic solutions are marked with an asterisk (*).
Figure 4.
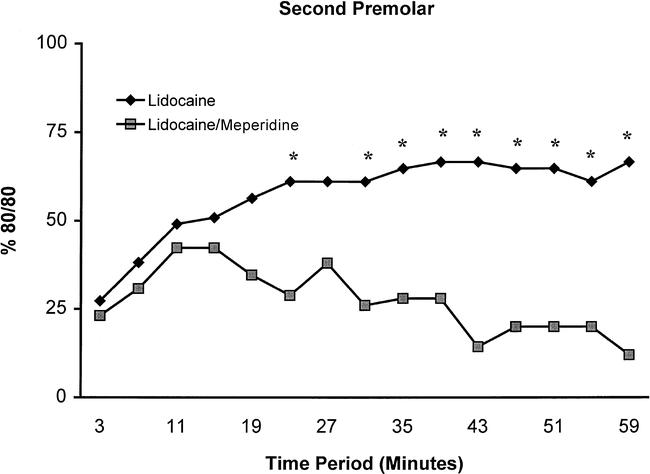
Incidence of second premolar anesthesia as determined by lack of response to electrical pulp testing at the maximum setting (percentage of 80/80s) at each postinjection time interval for the lidocaine and lidocaine/meperidine solutions. Significant differences (P < .05) between the 2 anesthetic solutions are marked with an asterisk (*).
Figure 5.
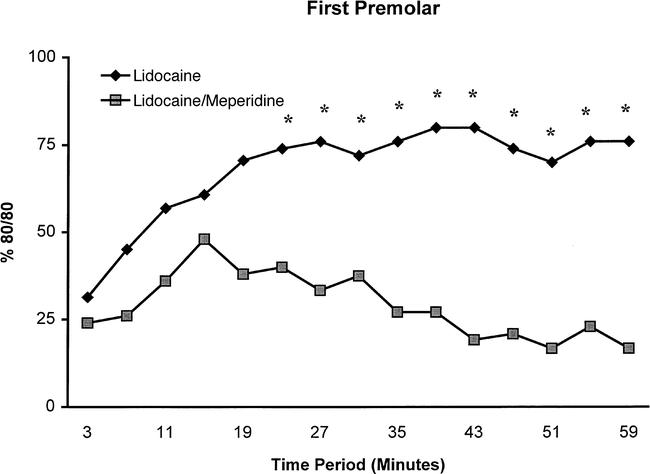
Incidence of first premolar anesthesia as determined by lack of response to electrical pulp testing at the maximum setting (percentage of 80/80s) at each postinjection time interval for the lidocaine and lidocaine/meperidine solutions. Significant differences (P < .05) between the 2 anesthetic solutions are marked with an asterisk (*).
Figure 6.
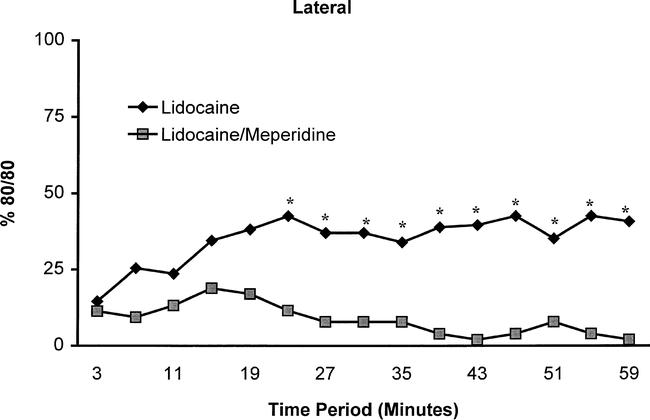
Incidence of lateral incisor anesthesia as determined by lack of response to electrical pulp testing at the maximum setting (percentage of 80/80s) at each postinjection time interval for the lidocaine and lidocaine/meperidine solutions. Significant differences (P < .05) between the 2 anesthetic solutions are marked with an asterisk (*).
Acknowledgments
This study was supported by Graduate Endodontic Research Funds.
REFERENCES
- Ågren E, Danielsson K. Conduction block analgesia in the mandible. Swed Dent J. 1981;5:81–89. [PubMed] [Google Scholar]
- Nusstein J, Reader A, Beck M. Anesthetic efficacy of different volumes of lidocaine with epinephrine for inferior alveolar nerve blocks. Gen Dent. 2002;50:372–375. [PubMed] [Google Scholar]
- Mikesell P, Nusstein J, Reader A, Beck M, Weaver J. A comparison of articaine and lidocaine for inferior alveolar nerve blocks. J Endod. 2005;31:265–270. doi: 10.1097/01.don.0000140576.36513.cb. [DOI] [PubMed] [Google Scholar]
- McLean C, Reader A, Beck M, Meyers WJ. An evaluation of 4% prilocaine and 3% mepivacaine compared to 2% lidocaine (1 : 100,000 epinephrine) for inferior alveolar nerve block. J Endod. 1993;19:146–150. doi: 10.1016/s0099-2399(06)80510-8. [DOI] [PubMed] [Google Scholar]
- Vreeland D, Reader A, Beck M, Meyers W, Weaver J. An evaluation of volumes and concentrations of lidocaine in human inferior alveolar nerve block. J Endod. 1989;15:6–12. doi: 10.1016/S0099-2399(89)80091-3. [DOI] [PubMed] [Google Scholar]
- Hinkley S, Reader A, Beck M, Meyers W. An evaluation of 4% prilocaine with 1 : 200,000 epinephrine and 2% mepivacaine with levonordefrin compared to 2% lidocaine with 1 : 100,000 epinephrine for inferior alveolar nerve block. Anesth Prog. 1991;38:84–89. [PMC free article] [PubMed] [Google Scholar]
- Chaney MA, Kerby R, Reader A, Beck FM, Meyers WJ, Weaver J. An evaluation of lidocaine hydrocarbonate compared with lidocaine hydrochloride for inferior alveolar nerve block. Anesth Prog. 1991;38:212–216. [PMC free article] [PubMed] [Google Scholar]
- Nist R, Reader A, Beck M, Meyers W. An evaluation of the incisive nerve block and combination inferior alveolar and incisive nerve blocks in mandibular anesthesia. J Endod. 1992;18:455–459. doi: 10.1016/S0099-2399(06)80849-6. [DOI] [PubMed] [Google Scholar]
- Dagher BF, Yared GM, Machtou P. The anesthetic efficacy of volumes of lidocaine in inferior alveolar nerve blocks. J Endod. 1997;23:178–180. doi: 10.1016/S0099-2399(97)80271-3. [DOI] [PubMed] [Google Scholar]
- Clark S, Reader A, Beck M, Meyers WJ. Anesthetic efficacy of the mylohyoid nerve block and combination inferior alveolar nerve block/mylohyoid nerve block. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999;87:557–563. doi: 10.1016/s1079-2104(99)70133-2. [DOI] [PubMed] [Google Scholar]
- Hannan L, Reader A, Nist R, Beck M, Meyers WJ. The use of ultrasound for guiding needle placement for inferior alveolar nerve blocks. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999;87:658–665. doi: 10.1016/s1079-2104(99)70156-3. [DOI] [PubMed] [Google Scholar]
- Ridenour S, Reader A, Beck M, Weaver J. Anesthetic efficacy of a combination of hyaluronidase and lidocaine with epinephrine in inferior alveolar nerve blocks. Anesth Prog. 2001;48:9–15. [PMC free article] [PubMed] [Google Scholar]
- Yonchak T, Reader A, Beck M, Meyers WJ. Anesthetic efficacy of unilateral and bilateral inferior alveolar nerve blocks to determine cross innervation in anterior teeth. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001;92:132–135. doi: 10.1067/moe.2001.115720. [DOI] [PubMed] [Google Scholar]
- Nusstein J, Reader A, Nist R, Beck M, Meyers WJ. Anesthetic efficacy of the supplemental intraosseous injection of 2% lidocaine with 1 : 100,000 epinephrine in irreversible pulpitis. J Endod. 1998;24:487–491. doi: 10.1016/S0099-2399(98)80053-8. [DOI] [PubMed] [Google Scholar]
- Nusstein J, Kennedy S, Reader A, Beck M, Weaver J. Anesthetic efficacy of the supplemental X-tip intraosseous injection in patients with irreversible pulpitis. J Endod. 2003;29:724–728. doi: 10.1097/00004770-200311000-00010. [DOI] [PubMed] [Google Scholar]
- Claffey E, Reader A, Nusstein J, Beck M, Weaver J. Anesthetic efficacy of articaine for inferior alveolar nerve blocks in patients with irreversible pulpitis. J Endod. 2004;30:568–571. doi: 10.1097/01.don.0000125317.21892.8f. [DOI] [PubMed] [Google Scholar]
- Cohen HP, Cha BY, Spangberg LSW. Endodontic anesthesia in mandibular molars: a clinical study. J Endod. 1993;19:370–373. doi: 10.1016/S0099-2399(06)81366-X. [DOI] [PubMed] [Google Scholar]
- Reisman D, Reader A, Nist R, Beck M, Weaver J. Anesthetic efficacy of the supplemental intraosseous injection of 3% mepivacaine in irreversible pulpitis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997;84:676–682. doi: 10.1016/s1079-2104(97)90372-3. [DOI] [PubMed] [Google Scholar]
- Kennedy S, Reader A, Nusstein J, Beck M, Weaver J. The significance of needle deflection in success of the inferior alveolar nerve block in patients with irreversible pulpitis. J Endod. 2003;29:630–633. doi: 10.1097/00004770-200310000-00004. [DOI] [PubMed] [Google Scholar]
- Parente SA, Anderson RW, Herman WW, Kimbrough WF, Weller RN. Anesthetic efficacy of the supplemental intra-osseous injection for teeth with irreversible pulpitis. J Endod. 1998;24:826–828. doi: 10.1016/S0099-2399(98)80011-3. [DOI] [PubMed] [Google Scholar]
- Yagiela JA, Dowd FJ, Neidle EA. Pharmacology and Therapeutics for Dentistry. 5th ed. New York, NY: Elsevier Mosby Co; 2004. p. 324. [Google Scholar]
- Cousins M, Mather L. Intrathecal and epidural administration of opioids. Anesthesiology. 1984;61:276–310. [PubMed] [Google Scholar]
- Brau ME, Koch ED, Vogel W, Hempelmann G. Tonic blocking of meperidine on Na+ and K+ channels in amphibian peripheral nerves. Anesthesiology. 2000;92:147–155. doi: 10.1097/00000542-200001000-00026. [DOI] [PubMed] [Google Scholar]
- Famewo C, Naguib M. Spinal anaesthesia with meperidine as the sole agent. Can Anaesth Soc J. 1985;32:533–537. doi: 10.1007/BF03010804. [DOI] [PubMed] [Google Scholar]
- Acalovschi I, Ene V, Lorinczi E, Nicolaus F. Saddle block with pethidine for perineal operations. Br J Anaesth. 1986;58:1012–1016. doi: 10.1093/bja/58.9.1012. [DOI] [PubMed] [Google Scholar]
- Nguyen T, Orliaguet G, Ngu T, Bonnet F. Spinal anesthesia with meperidine as the sole agent for cesarean delivery. Reg Anesth. 1994;19:386–389. [PubMed] [Google Scholar]
- Norris M, Honet J, Leighton B, Arkoosh V. A comparison of meperidine and lidocaine for spinal anesthesia for postpartum tubal ligation. Reg Anesth. 1996;21:84–88. [PubMed] [Google Scholar]
- Sia A, Chow M, Koay C, Chong J. Intrathecal pethidine: an alternative anaesthetic for transurethral resection of prostate? Anaesth Intensive Care. 1997;25:650–654. doi: 10.1177/0310057X9702500610. [DOI] [PubMed] [Google Scholar]
- Hassan H, Youssef H, Renck H. Duration of experimental nerve block by combinations of local anesthetic agents. Acta Anaesthesiol Scand. 1993;37:70–74. doi: 10.1111/j.1399-6576.1993.tb03601.x. [DOI] [PubMed] [Google Scholar]
- Kafle S. Intrathecal meperidine for elective caesarean section: a comparison with lidocaine. Can J Anaesth. 1993;40:718–721. doi: 10.1007/BF03009767. [DOI] [PubMed] [Google Scholar]
- Lewis RP, Spiers SPW, McLaren IM, Hunt PC, Smith HS. Pethidine as spinal anaesthetic agent: a comparison with plain bupivacaine in patients undergoing transurethral resection of the prostate. Eur J Anaesth. 1992;9:105–109. [PubMed] [Google Scholar]
- Chaudhari L, Kane D, Shivkumar B, Kamath S. Comparative study of intrathecal pethidine versus lignocaine as an anaesthetic and a postoperative analgesic for perianal surgery. J Postgrad Med. 1996;42:43–45. [PubMed] [Google Scholar]
- Patel D, Janardhan Y, Merai B, Robalino J, Shevde K. Comparison of intrathecal meperidine and lidocaine in endoscopic urological procedures. Can J Anesth. 1990;37:567–570. doi: 10.1007/BF03006327. [DOI] [PubMed] [Google Scholar]
- Maurette P, Bonada G, Djiane V, Erny P. A comparison between lidocaine alone and lidocaine with meperidine for continuous spinal anesthesia. Reg Anesth. 1993;18:290–295. [PubMed] [Google Scholar]
- Armstrong PJ, Morton CPJ, Nimmo AF. Pethidine has a local anaesthetic action on peripheral nerves in vivo: addition to prilocaine 0.25% for intravenous regional anaesthetic in volunteers. Anaesthesia. 1993;48:382–386. doi: 10.1111/j.1365-2044.1993.tb07008.x. [DOI] [PubMed] [Google Scholar]
- Elhakim M, Abdul Salam AY, Eid A, Kaschef N, Mostafa BE. Inclusion of pethidine in lidocaine for infiltration improves analgesia following tonsillectomy in children. Acta Anaesthesiol Scand. 1997;41:214–217. doi: 10.1111/j.1399-6576.1997.tb04668.x. [DOI] [PubMed] [Google Scholar]
- Pang WW, Mok MS, Huang S, Hwang MH. The analgesic effect of fentanyl, morphine, meperidine, and lidocaine in the peripheral veins: a comparative study. Anesth Analg. 1998;86:382–386. doi: 10.1097/00000539-199802000-00031. [DOI] [PubMed] [Google Scholar]
- Jaffe RA, Rowe MA. A comparison of the local anesthetic effects of meperidine, fentanyl, and sufentanil on doral root axons. Anesth Analg. 1996;83:776–781. doi: 10.1097/00000539-199610000-00021. [DOI] [PubMed] [Google Scholar]
- Hunter E, Frank G. An opiate receptor on frog sciatic nerve axons. Can J Physiol Pharmacol. 1979;57:1171–1174. doi: 10.1139/y79-173. [DOI] [PubMed] [Google Scholar]
- Reuben SS, Steinberg RB, Lurie SD, Gibson CS. A dose-response study of regional anesthesia with meperidine. Anesth Analg. 1999;88:831–835. doi: 10.1097/00000539-199904000-00028. [DOI] [PubMed] [Google Scholar]
- Heft MW, Parker SR. An experimental basis for revising the graphic rating scale for pain. Pain. 1984;19:153–161. doi: 10.1016/0304-3959(84)90835-2. [DOI] [PubMed] [Google Scholar]
- Jorgensen NB, Hayden J., Jr. Local and General Anesthesia in Dentistry. 2nd ed. Philadelphia, PA: Lea & Febiger; 1967. [Google Scholar]
- Dreven L, Reader A, Beck M, Meyers W, Weaver J. An evaluation of the electric pulp tester as a measure of analgesia in human vital teeth. J Endod. 1987;13:233–238. doi: 10.1016/s0099-2399(87)80097-3. [DOI] [PubMed] [Google Scholar]
- Certosimo A, Archer R. A clinical evaluation of the electric pulp tester as an indicator of local anesthesia. Oper Dent. 1996;21:25–30. [PubMed] [Google Scholar]
- Hardman JG, Limbird LE, Gilman AG, editors. Goodman and Gilman's The Pharmacological Basis of Therapeutics. 10th ed. New York, NY: The McGraw-Hill Co; 2001. p. 592. [Google Scholar]
- Wagner LE, Eaton M, Sabnis SS, Gingrich KJ. Meperidine and lidocaine block of recombinant voltage dependant Na+ channels: evidence that meperidine is a local anesthetic. Anesthesiology. 1999;91:1481–1490. doi: 10.1097/00000542-199911000-00042. [DOI] [PubMed] [Google Scholar]
- Flanagan M, Walker F, Butterworth J. Failure of meperidine to anesthetize human median nerve. A blinded comparison with lidocaine and saline. Reg Anesth. 1997;22:73–79. doi: 10.1016/s1098-7339(06)80059-3. [DOI] [PubMed] [Google Scholar]