Methods of Assessing Cataract Outcome
1. Population based studies
Several population-based blindness surveys and rapid assessments, conducted in the late 1990s, indicated that of all eyes operated on for cataract, 21–53% had a presenting visual acuity of less than 6/60.1,2,3,4 These figures include patients operated on recently as well as decades earlier. They include operations done under excellent as well as less favourable conditions, by experienced as well as less experienced surgeons, sometimes even by couchers.∗
Aphakic spectacles may have been lost or damaged. People with initial good outcome may have developed retinal disorders, reducing vision as they get older. Outcome data from surveys may not do justice to recent advancements in IOL surgery, but they do reflect what the public sees and determine their expectations and trust on regaining sight after surgery.
2. Monitoring case studies
Routine monitoring of pre-operative, operative and post-operative data of each operated patient calculates the visual outcome and assesses the quality of cataract surgery. It is assumed that encouraging eye surgeons to monitor their own results, over time, in itself will lead to better outcomes of cataract surgery. Better results will reduce fear and motivate more patients to come for surgery. Outcome data should not be used to compare surgeons or centres, since case selection, surgical skills, procedures and facilities, follow-up periods and other factors affecting outcome, differ by surgeon and by centre. Routine monitoring should be used to evaluate results of individual surgeons or centres over time. It can be useful to evaluate the surgical learning curve of residents during their training.
The Tools
We developed a manual ‘tally’ (record) sheet system and two computerised packages. The computer systems use more input data and provide a more detailed analysis. It is important to select the method that is most suitable and usable on a regular and long term basis in your own situation. When skilled data entry operators are not available it is advisable to use the manual tally sheet system.
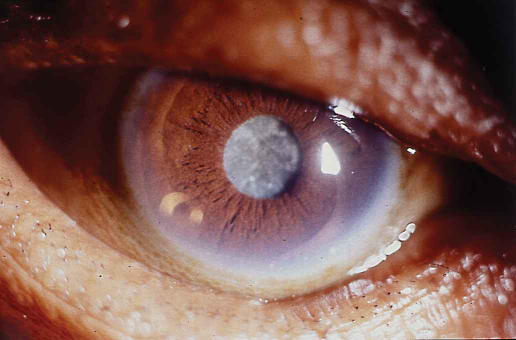
Age-related cataract – the most common cause of blindness in the world
Photo: John DC Anderson
1. Manual tally sheets
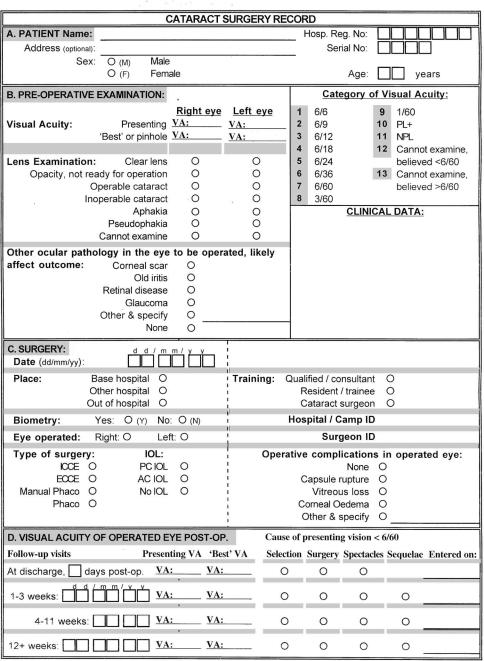
This system is developed for eye units without computers or units without data entry staff. Pre-operative, operative and post-operative data are collected from the case sheet normally used by the eye surgeon(s). Alternatively, the standard Cataract Surgery Record (CSR) from the computer systems can be completed and added to the case sheet. Using the CSR would also facilitate an easy change over to a computerised system at a later stage (see Figure 2).
Figure 2.
Cataract Surgery Record
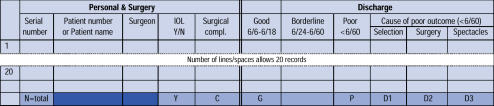
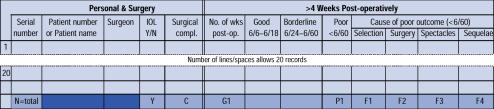
The data are entered on the tally sheets (Figures 1a and 1b), one row for each operated eye. Each sheet has 20 records. When 100 records are entered (5 full sheets), the totals in each column are equal to the percentages. When not all operated patients return for review, care should be taken with the interpretation of percentages in the ‘>4 weeks post-operative’ column as percentages are drawn from less than 100 cases.
Figure 1a.
The Manual Tally Sheet: Discharge
Figure 1b.
The Manual Tally Sheet: >4 Weeks Post-operatively
For all cases with ‘poor’ outcome a cause must be indicated. This helps the surgeon to decide whether current practices need modification to improve results. The causes of poor outcome can be divided into four categories:
Selection: patient-related risk factors, e.g., concurrent diseases affecting vision
Surgery: surgical or immediate post-operative complications
Spectacles: uncorrected refractive error, wrong power IOL
Sequelae: late post-operative complications.
Surgical procedures and provision of optical correction are relatively easy to modify. Selection procedures can also be modified, but patients should not be denied surgery if their vision has a fair chance of improvement by cataract surgery. Late post-operative sequelae are most difficult to control.
When more than one surgeon is operating, all data can be entered on one form, or each surgeon can have his/her own form. The second option will enable each surgeon to follow his/her own outcomes over time. However, the number of operations needs to be sufficient to allow meaningful interpretation.
2. Computer package (MS-DOS)
This package is programmed in Epi-Info 6.04 and runs under MS-DOS and Windows. It can run on all IBM compatible computers with 5 MB free disk space. Data collection for both computer systems is done with the standard Cataract Surgery Record (Figure 2). Data from this form are entered into the computer.
Age-related cataract
Photo: John D C Anderson
3. Computer package (Windows)
This package is programmed in Visual FoxPro 6.0 and runs under Windows only. It is recommended for computers with a processor faster than a Pentium 1, 90 MHz, with at least 8 MB free disk space. The reports produced by both computer packages are exactly the same, but the graphs from the Windows package are of better quality and show the data table. Experienced Epi-Info users can do custom analysis with the DOS package.
Ongoing Report
In the ongoing report the records are placed in chronological order by date of operation and shown in groups of 100. This allows the user to follow trends over time with meaningful percentages. The report provides the following tables:
Operative complications: total and type of complication.
Percentage of good, borderline or poor outcome at discharge.
Cause of poor outcome (VA<6/60) at discharge.
Percentage of good, borderline or poor outcome at 4 weeks or more post-operatively.
Cause of poor outcome (VA<6/60) at 4 weeks or more post-operatively.
The ongoing report can be used to evaluate cataract outcome at any time. Care should be taken with the interpretation of percentages when less than 100 records have been entered.
Annual Report
The annual report is best used to present outcome data for a whole year, or to link data to a particular month. The following tables are provided:
Age group and sex of operated patients.
Number of first eyes and second eyes operated on.
Proportion of known ocular pathology in operated eye.
Visual acuity in the operated eye pre-operatively, at discharge and follow-up.
Visual acuity in the better eye pre-operatively, at discharge and follow-up.
Good / borderline / poor outcome at discharge by month (presenting VA).
Proportion of good / borderline / poor outcome by follow-up (presenting VA).
Operative complications and type of complications by month.
Operative complications by place of surgery.
Operative complications by cadre of surgeons.
Operative complications by additional ocular pathology.
Operative complications by type of surgery.
Causes of poor outcome at discharge and follow-up.
Percentage of poor visual outcome at discharge and follow-up, by type and by place of surgery.
While the manual tally sheet system can register one follow-up visit at 4 or more weeks post-operatively, the computer system ideally registers three follow-up visits: at 1–3 weeks, 4–11 weeks and 12 or more weeks post-operatively. The pilot study showed that optimal visual outcome was reached at 6 months or more after surgery and that the World Health Organization visual outcome targets were realistic.5 In many countries not all patients return after surgery. The pilot study showed that results from patients who do come for follow-up are similar to those from patients who did not return, but were visited at home.
Bar graphs showing the proportion of good, borderline and poor outcomes per group of 100 operated eyes (Figure 3) should be displayed in the operating theatre.
Figure 3.
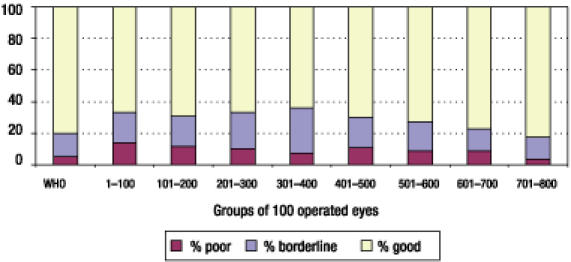
Proportion of Good/Borderline/Poor Outcomes at 12 or more Weeks Post-operatively, per 100 Operated Eyes
The following guidelines are useful to evaluate quality:
- Proportion of cases with IOL: a target percentage can be set according to local circumstances
- – If less, improve availability and affordability of IOLs and ensure that all surgeons are adequately trained in IOL surgery and have the necessary equipment.
- Percentage of complications should be less than 10%, with posterior capsule rupture and vitreous loss each not exceeding 5%
- – If more, improve surgical technique by asking for advice from a good and experienced cataract surgeon. Also, ensure that all surgeons are adequately trained in IOL surgery and have the necessary equipment.
At discharge, more than 50% of cases should have good presenting vision and less than 10% poor outcome
At 4 weeks or more post-operatively, more than 80% of cases should have good presenting vision and less than 5% poor outcome
- At 4 weeks or more post-operatively, more than 90% of cases should have good vision with best correction and less than 5% poor outcome
- – If not, analyse the causes of poor outcome. If surgical, take action as above. If refraction, provide at least best spherical correction spectacles at an affordable price.
- The trend over time is static outside the recommended limits, or worsening
- – Carefully analyse the reasons for lack of improvement and deal with identified problems.
The WHO has recommended that it should be a requirement for all eye surgeons to monitor their own results over time, and identify causes of poor outcome (selection, surgery, spectacles, sequelae). Addressing these causes is likely to improve future outcomes of cataract surgery. Monitoring outcomes is an essential part of the training of everyone who will do cataract surgery, so that it becomes routine and required practice to think about quality and how it can be improved.
Footnotes
Couching is the ‘surgical’ displacement of the cataractous lens, usually posteriorly and inferiorly into the vitreous cavity, often using a needle. It is a method used by some traditional healers.
References
- 1.Zhao J, Sui R, Jia L, Fletcher AE, Ellwein LB. Visual acuity and quality of life outcomes in patients with cataract in Shunyi County, China. Am J Ophthalmol. 1998;126:515–523. doi: 10.1016/s0002-9394(98)00274-8. [DOI] [PubMed] [Google Scholar]
- 2.He M, Xu J, Li S, Wu K, Munoz S, Ellwein LB, et al. Visual acuity and quality of life in patients with cataract in Doumen County, China. Ophthalmology. 1999;106:1609–1615. doi: 10.1016/S0161-6420(99)90460-8. [DOI] [PubMed] [Google Scholar]
- 3.Limburg H, Foster A, Vaidyanathan K, Murthy GVS. Monitoring visual outcome of cataract surgery in India. Bull WHO. 1999;77:455–460. [PMC free article] [PubMed] [Google Scholar]
- 4.Dandona L, Dandona R, Naduvilath TJ, McCarthy CA, Mandal P, Srinivas M, et al. Population-based assessment of the outcome of cataract surgery in an urban population in southern India. Am J Ophthalmol. 1999;127:650–658. doi: 10.1016/s0002-9394(99)00044-6. [DOI] [PubMed] [Google Scholar]
- 5.Limburg H, Foster A, Gilbert C, Johnson GJ, Kyndt M. Routine monitoring of cataract outcome – results from eight study centres. Submitted for publication. [DOI] [PMC free article] [PubMed]