Significant progress is being made in addressing the cataract blindness problem in parts of the developing world. For example, surgical coverage among those afflicted by bilateral blindness because of cataract has been shown to exceed 75% in parts of India, particularly among the literate and urban residents.1,2 Considering that all cataract blind persons are not candidates for surgery because of co-existing ocular pathology or other medical contraindications, surgical coverage at these levels may be approaching a natural upper limit. Expanded prevention of blindness efforts, such as those currently underway in India, appear to be having a favourable impact on the cataract blindness ‘backlog’.
Visual Acuity Outcomes
It is also becoming evident, however, that much more attention must be given to improving visual acuity outcomes among those who have had cataract surgery. Recent population-based surveys in several countries have shown that 40–75% of post-operative eyes have a presenting visual acuity worse than 6/18, with as many as 50% worse than 6/60.3–6 This high proportion of cataract-operated cases with poor vision is a matter of great concern. Many cataract patients are not experiencing the level of vision restoration possible with modern day surgery. A clinical trial of cataract surgery at the Aravind Eye Hospital in India suggests that four years after surgery no more than 25% should have presenting visual acuity worse than 6/18; and with best corrected vision, no more than 5% should be in this category. It might be expected that cases operated on in recent years are faring better than earlier cases. This is generally not the case, however, as was shown in the referenced surveys1–6 where a cross-sectional sample of patients, some operated on near the time of the survey and others operated on decades earlier, were evaluated.
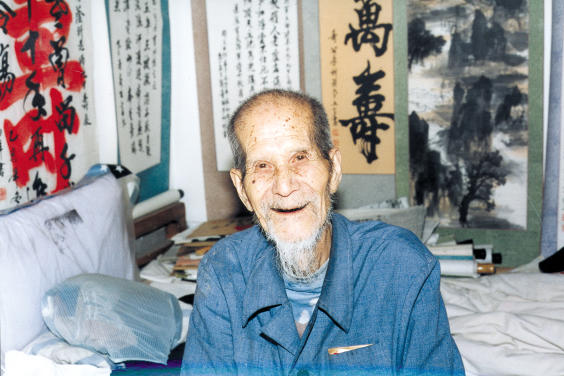
Vision 2020: The Right to Sight – for all ages. This lively 95-year-old Chinese calligrapher had early bilateral cataract
Photo: Murray McGavin
ICCE or ECCE without IOL versus IOL Surgery
These surveys also showed that aphakic patients who received intracapsular cataract extraction (ICCE), or extracapsular cataract extraction (ECCE) without an intraocular lens (IOL), were at a disadvantage compared to those who received IOL surgery. (Unfortunately, it was common for those with aphakia to present without the necessary spectacles). Uncorrected aphakia and other refractive error accounted for up to half of the vision impairment seen in aphakic eyes. Although the differential between IOL and non-IOL patients narrowed when best-corrected vision was considered, it is presenting vision that represents the actual circumstances under which people function in day-to-day activities. Accordingly, the measurement of visual acuity with the presenting correction, if any, not best-corrected measurement, is what counts when assessing the vision restoration benefits achieved through cataract surgery.
Factors Contributing to Post-operative Visual Impairment and Blindness
Even though surgical coverage may be on the rise, a proportionate decrease in the prevalence of cataract blindness will not be realised if a substantial number of those already operated on for cataract are still blind. To illustrate, the prevalence of cataract visual impairment and blindness (< 6/60) among those ≥ 50 years of age in a rural area of India was found to be 8.1%. This dropped to 5.7% if those who were already operated on, but were visually impaired, are excluded from the calculation.6
Multiple factors undoubtedly contribute to poor visual acuity among the cataract-operated: a less than favourable surgical setting, such as found in surgical camps; a less than competent surgical technique; inappropriate selection of surgical cases; or perhaps inadequate patient follow-up. It is apparent that patients operated on in well-equipped facilities by experienced surgeons do better. Patient hygiene and behaviour are also important. As already noted, not wearing aphakic spectacles will, by itself, result in a poor outcome among ICCE cases.
It appears that much of the visual impairment in operated eyes is uncorrectable because of surgical complications. Other ocular pathology, which may have been co-existing at the time of cataract surgery, or that which manifested itself later, is also responsible for some of the poor outcomes. From the perspective of the patient, however, the reason behind the poor outcome is less important than the fact that poor vision exists. The patient may not be able to distinguish between vision deterioration associated with the onset of new ocular pathologies versus that associated with surgical complications or undetected co-existing disease. Patients with poor vision may conclude that cataract surgery is only partially, or temporarily, effective in restoring sight, if at all. This message may be communicated to those still contemplating whether to seek such surgery and, thus, serve as a deterrent to care.
It is evident that poor visual acuity outcomes among those operated on for cataract are not limited to any one area or country. Studies in different parts of China, India, and Nepal all point to the need for greater recognition of less than desirable outcomes and the necessity for remedial action.
The Goal of Good Surgical Outcomes
The cataract blind, and particularly those in poverty, must overcome numerous socio-economic barriers involving significant sacrifices to obtain treatment. We must do more to ensure that, to the greatest extent possible, the result is complete sight restoration. The ability to produce consistently good surgical outcomes is becoming even more important as patients in developing countries are increasingly seeking cataract surgery earlier, before visual impairment has had a significant economic and social impact. Not only do patients with early cataract have nothing to gain by unsuccessful surgery, they have vision to lose.
In the articles that follow, Drs. Dandona, Limburg, Cook, Thomas and Kuriakose further discuss cataract surgery outcomes and what can be done to improve them.
References
- 1.Thulasiraj RD, Rahamathulla R, Saraswati A, Selvaraj S, Ellwein LB. The Sivaganga Eye Survey: I. Blindness and cataract surgery. (Submitted) [DOI] [PubMed]
- 2.Limburg H, Vasavada A, Muzumdar G, et al. Rapid assessment of cataract blindness in an urban district of Gujarat. Indian J Ophthalmol. 1999;47:135–41. [Google Scholar]
- 3.Pokharel GP, Selvaraj S, Ellwein LB. Visual-functioning, and quality of life outcomes between cataract operated and un-operated blind populations in Nepal. Br J Ophthalmol. 1998;82:606–10. doi: 10.1136/bjo.82.6.606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.He M, Xu J, Li S, Wu K, Munoz SR, Ellwein LB. Visual acuity and quality of life in patients with cataract in Doumen County, China. Ophthalmology. 1999;106:1609–15. doi: 10.1016/S0161-6420(99)90460-8. [DOI] [PubMed] [Google Scholar]
- 5.Dandona L, Dandona R, Naduvilath TJ, et al. Population-based assessment of the outcomes of cataract surgery in an urban population in southern India. Am J Ophthalmol. 1999;127:650–58. doi: 10.1016/s0002-9394(99)00044-6. [DOI] [PubMed] [Google Scholar]
- 6.Murthy GVS, Ellwein LB, Gupta S, Tanikachalam K, Ray M, Dada VK. A population-based eye survey of older adults in a rural district of Rajasthan: II. Outcomes in cataract surgery. (Submitted) [DOI] [PubMed]