Abstract
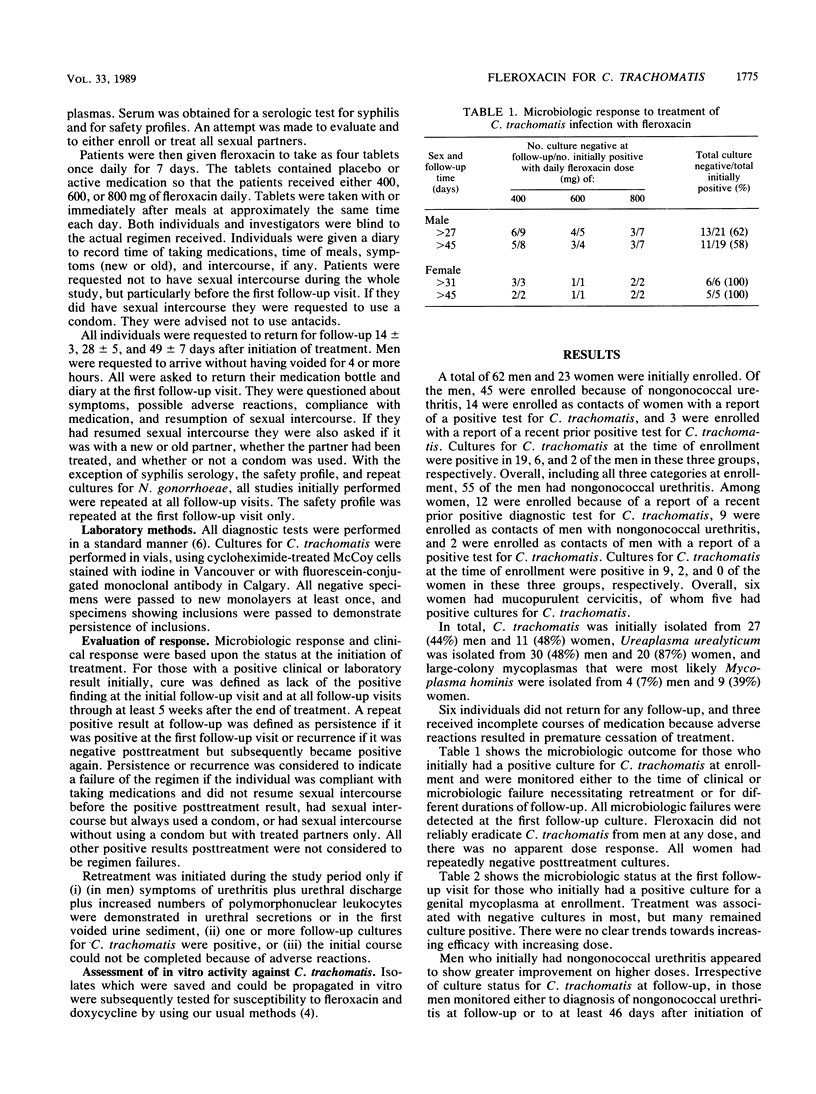
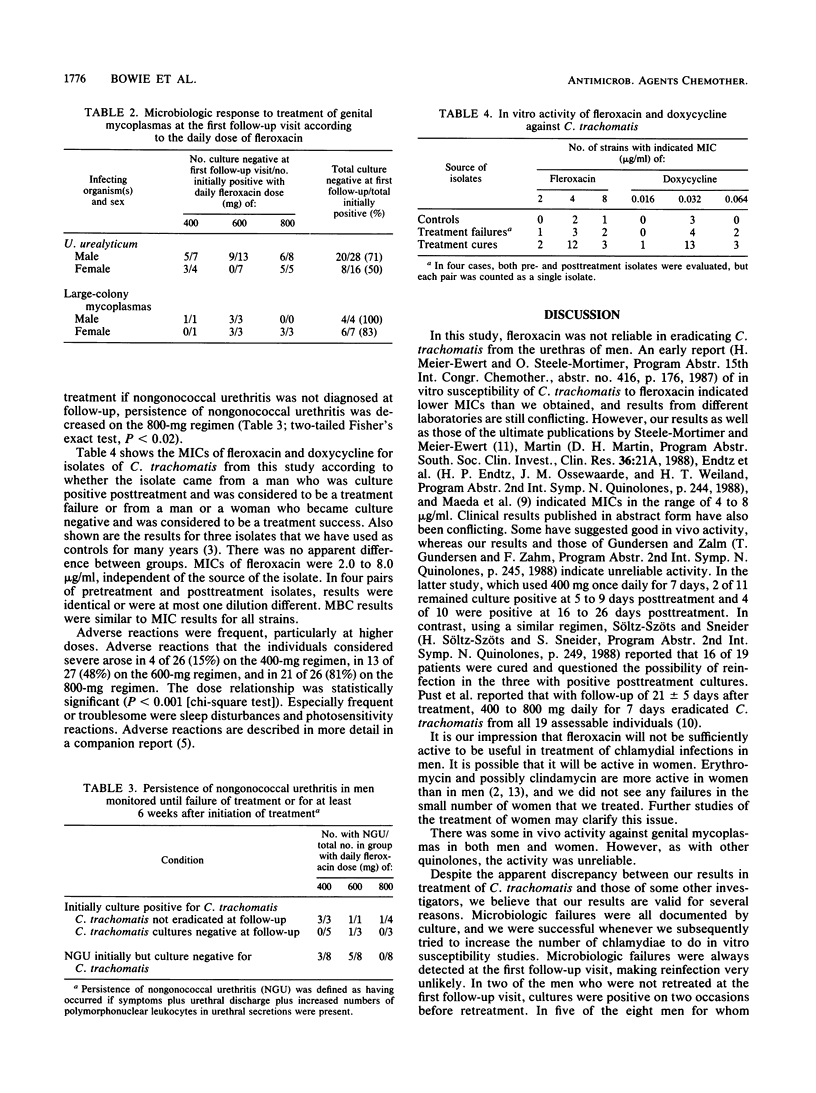
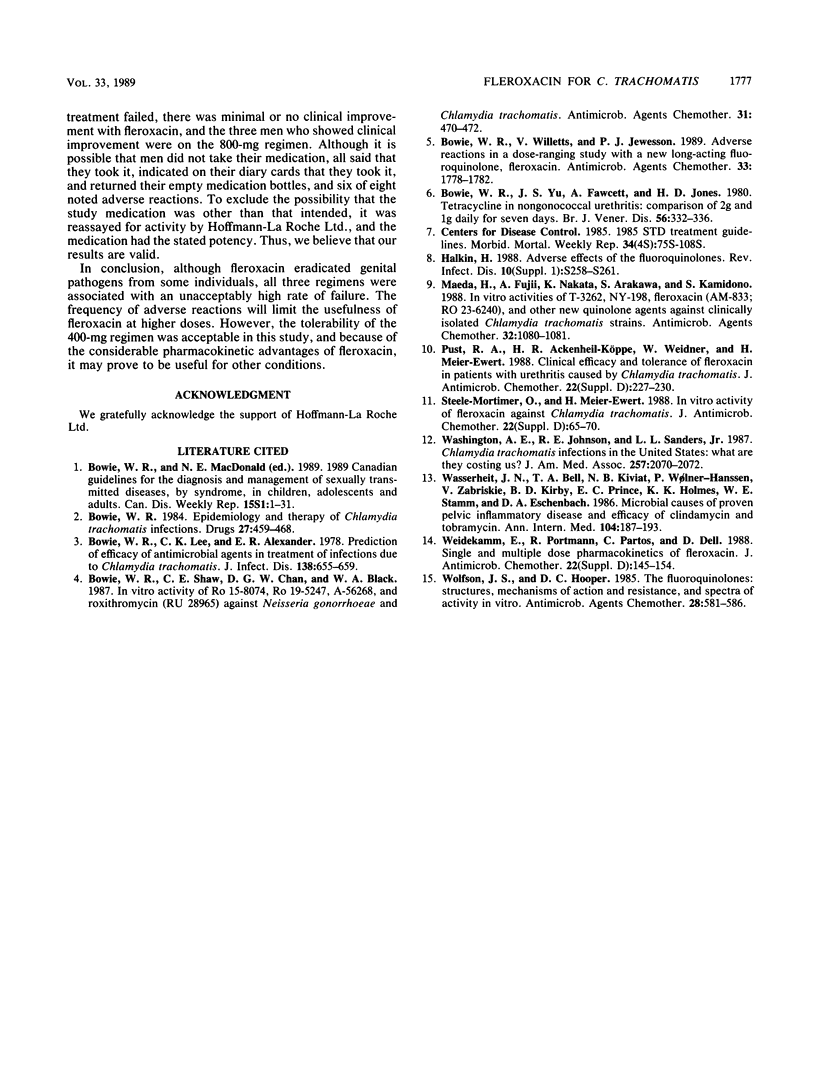
Men and women with suspected or proven genital infections caused by Chlamydia trachomatis were enrolled in a double-blind study to evaluate the efficacy and tolerability of fleroxacin. Patients received either 400, 600, or 800 mg once daily for 7 days and were monitored approximately 2, 4, and 7 weeks after initiation of therapy. In men monitored for at least 6 weeks or until failure of the therapy, fleroxacin failed to eradicate C. trachomatis in three of eight on the 400-mg regimen, in one of four on the 600-mg regimen, and in four of seven on the 800-mg regimen. All five women monitored for at least 6 weeks became culture negative. There was no association between in vitro susceptibility of C. trachomatis to fleroxacin and outcome, with MICs being 4 to 8 migrograms/ml for almost all isolates tested. Among those with positive cultures for Ureaplasma urealyticum initially, the first follow-up cultures remained positive in 8 (29%) of 28 men and 8 (50%) of 16 women. Independent of culture results, men with nongonococcal urethritis receiving 800 mg of fleroxacin were significantly more likely to show a clinical response than men receiving 400 or 600 mg (93 versus 54%). Adverse events were frequent, often severe, and dose related. Insomnia and photosensitivity reactions were the most important. The adverse reactions and unacceptably high rates of microbiologic failure resulted in premature termination of the study.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bowie W. R. Epidemiology and therapy of Chlamydia trachomatis infections. Drugs. 1984 May;27(5):459–468. doi: 10.2165/00003495-198427050-00005. [DOI] [PubMed] [Google Scholar]
- Bowie W. R., Lee C. K., Alexander E. R. Prediction of efficacy of antimicrobial agents in treatment of infections due to Chlamydia trachomatis. J Infect Dis. 1978 Nov;138(5):655–659. doi: 10.1093/infdis/138.5.655. [DOI] [PubMed] [Google Scholar]
- Bowie W. R., Shaw C. E., Chan D. G., Black W. A. In vitro activity of Ro 15-8074, Ro 19-5247, A-56268, and roxithromycin (RU 28965) against Neisseria gonorrhoeae and Chlamydia trachomatis. Antimicrob Agents Chemother. 1987 Mar;31(3):470–472. doi: 10.1128/aac.31.3.470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowie W. R., Willetts V., Jewesson P. J. Adverse reactions in a dose-ranging study with a new long-acting fluoroquinolone, fleroxacin. Antimicrob Agents Chemother. 1989 Oct;33(10):1778–1782. doi: 10.1128/aac.33.10.1778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowie W. R., Yu J. S., Fawcett A., Jones H. D. Tetracycline in nongonococcal urethritis. Comparison of 2 g and 1 g daily for seven days. Br J Vener Dis. 1980 Oct;56(5):332–336. doi: 10.1136/sti.56.5.332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halkin H. Adverse effects of the fluoroquinolones. Rev Infect Dis. 1988 Jan-Feb;10 (Suppl 1):S258–S261. doi: 10.1093/clinids/10.supplement_1.s258. [DOI] [PubMed] [Google Scholar]
- Maeda H., Fujii A., Nakata K., Arakawa S., Kamidono S. In vitro activities of T-3262, NY-198, fleroxacin (AM-833; RO 23-6240), and other new quinolone agents against clinically isolated Chlamydia trachomatis strains. Antimicrob Agents Chemother. 1988 Jul;32(7):1080–1081. doi: 10.1128/aac.32.7.1080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pust R. A., Ackenheil-Köppe H. R., Weidner W., Meier-Ewert H. Clinical efficacy and tolerance of fleroxacin in patients with urethritis caused by Chlamydia trachomatis. J Antimicrob Chemother. 1988 Oct;22 (Suppl 500):227–230. doi: 10.1093/jac/22.supplement_d.227. [DOI] [PubMed] [Google Scholar]
- Steele-Mortimer O., Meier-Ewert H. In-vitro activity of fleroxacin against Chlamydia trachomatis. J Antimicrob Chemother. 1988 Oct;22 (Suppl 500):65–70. doi: 10.1093/jac/22.supplement_d.65. [DOI] [PubMed] [Google Scholar]
- Washington A. E., Johnson R. E., Sanders L. L., Jr Chlamydia trachomatis infections in the United States. What are they costing us? JAMA. 1987 Apr 17;257(15):2070–2072. [PubMed] [Google Scholar]
- Wasserheit J. N., Bell T. A., Kiviat N. B., Wølner-Hanssen P., Zabriskie V., Kirby B. D., Prince E. C., Holmes K. K., Stamm W. E., Eschenbach D. A. Microbial causes of proven pelvic inflammatory disease and efficacy of clindamycin and tobramycin. Ann Intern Med. 1986 Feb;104(2):187–193. doi: 10.7326/0003-4819-104-2-187. [DOI] [PubMed] [Google Scholar]
- Weidekamm E., Portmann R., Partos C., Dell D. Single and multiple dose pharmacokinetics of fleroxacin. J Antimicrob Chemother. 1988 Oct;22 (Suppl 500):145–154. doi: 10.1093/jac/22.supplement_d.145. [DOI] [PubMed] [Google Scholar]
- Wolfson J. S., Hooper D. C. The fluoroquinolones: structures, mechanisms of action and resistance, and spectra of activity in vitro. Antimicrob Agents Chemother. 1985 Oct;28(4):581–586. doi: 10.1128/aac.28.4.581. [DOI] [PMC free article] [PubMed] [Google Scholar]


