Abstract
BACKGROUND AND AIMS—To test the contribution of portal pressure gradient (PPG) and neurohumoral factors to sodium handling in cirrhotic patients without ascites, by comparing preascitic cirrhotic patients with patients with transjugular intrahepatic portosystemic stent shunt (TIPSS) and previous ascites. PATIENTS—Ten patients with TIPSS and 10 preascitic cirrhotic patients. METHODS—Changes in glomerular filtration, renal plasma flow, urinary sodium excretion (UNaV), and neurohumoral factors were measured before and for two hours after infusion of one litre of 0.9% saline over one hour. RESULTS—Glomerular filtration rate and renal plasma flow were significantly higher in patients with TIPSS compared with preascitic cirrhotic patients. Following saline infusion both parameters increased significantly; this increase was significantly greater in patients with TIPSS. UNaV increased significantly in both groups following saline infusion. The increase in UNaV was significantly greater in the TIPSS group. Plasma renin activity and angiotensin II decreased significantly in both groups. Basal UNaV was independently correlated with angiotensin II concentration and PPG and the change in UNaV correlated with the PPG. CONCLUSIONS—Results suggest that patients with advanced liver disease and low portal pressure handle sodium as well as patients with compensated liver disease and high portal pressure. These results are consistent with the notion that in addition to peripheral vasodilatation and severity of liver disease, the severity of portal hypertension contributes to the abnormalities of sodium retention in cirrhosis. Keywords: cirrhosis; transjugular intrahepatic portosystemic stent shunt; TIPSS; angiotensin; sodium handling; peripheral vasodilatation
Full Text
The Full Text of this article is available as a PDF (131.8 KB).
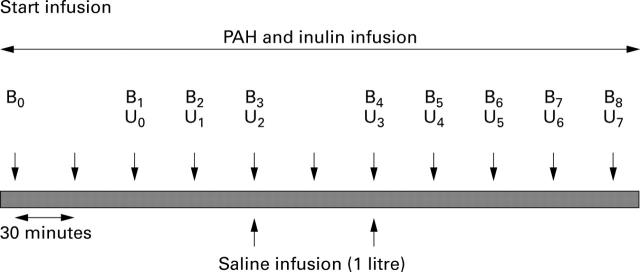
Figure 1 .
Study design. U1-U7, samples for urine volume, p-aminohippuric acid (PAH), inulin, sodium, and creatinine; B1-B7, blood samples for PAH, inulin, sodium, and creatinine; B3, B4 and B8, blood samples for plasma renin activity, angiotensin II, atrial natriuretic peptide, cyclic GMP, endothelin 1, and noradrenaline (norepinephrine). B0, B7, B3, B4, and B6, 250 ml water orally to ensure adequate urine flow.
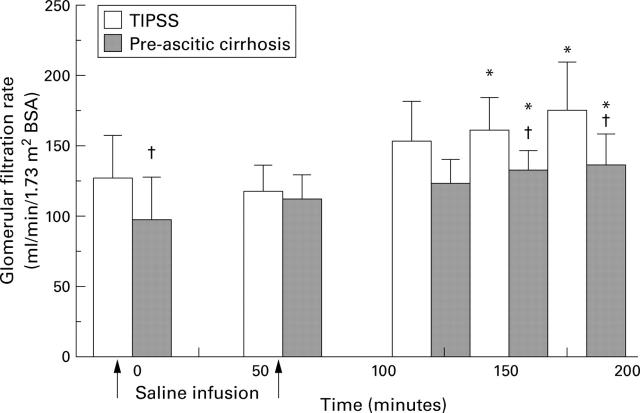
Figure 2 .
Changes in glomerular filtration rate following saline infusion. *p<0.05 versus baseline; †p<0.05 between groups.
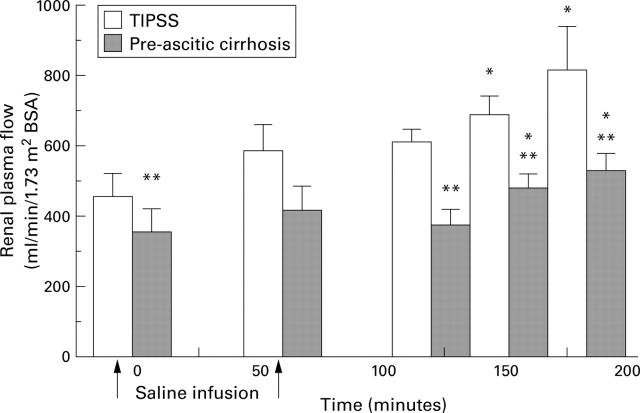
Figure 3 .
Changes in renal plasma flow following saline infusion. *p<0.05 versus baseline; **p<0.01 between groups.
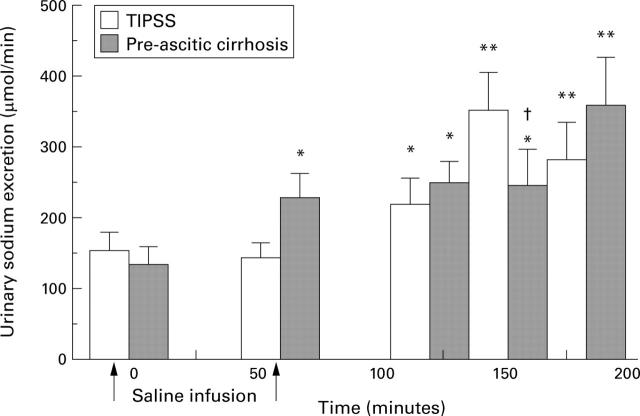
Figure 4 .
Changes in urinary sodium excretion following saline infusion. *p<0.05, **p<0.01 versus baseline; †p<0.03 between groups.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Arroyo V., Bosch J., Mauri M., Ribera F., Navarro-López F., Rodés J. Effect of angiotensin-II blockade on systemic and hepatic haemodynamics and on the renin-angiotensin-aldosterone system in cirrhosis with ascites. Eur J Clin Invest. 1981 Jun;11(3):221–229. doi: 10.1111/j.1365-2362.1981.tb01844.x. [DOI] [PubMed] [Google Scholar]
- Asbert M., Ginès A., Ginès P., Jiménez W., Clària J., Saló J., Arroyo V., Rivera F., Rodés J. Circulating levels of endothelin in cirrhosis. Gastroenterology. 1993 May;104(5):1485–1491. doi: 10.1016/0016-5085(93)90360-o. [DOI] [PubMed] [Google Scholar]
- Bendtsen F., Henriksen J. H., Sørensen T. I., Christensen N. J. Effect of oral propranolol on circulating catecholamines in cirrhosis: relationship to severity of liver disease and splanchnic haemodynamics. J Hepatol. 1990 Mar;10(2):198–204. doi: 10.1016/0168-8278(90)90052-s. [DOI] [PubMed] [Google Scholar]
- Bernardi M., Trevisani F., Santini C., Ligabue A., Capelli M., Gasbarrini G. Impairment of blood pressure control in patients with liver cirrhosis during tilting: study on adrenergic and renin-angiotensin systems. Digestion. 1982;25(2):124–130. doi: 10.1159/000198820. [DOI] [PubMed] [Google Scholar]
- Bichet D. G., Groves B. M., Schrier R. W. Mechanisms of improvement of water and sodium excretion by immersion in decompensated cirrhotic patients. Kidney Int. 1983 Dec;24(6):788–794. doi: 10.1038/ki.1983.229. [DOI] [PubMed] [Google Scholar]
- Bichet D. G., Van Putten V. J., Schrier R. W. Potential role of increased sympathetic activity in impaired sodium and water excretion in cirrhosis. N Engl J Med. 1982 Dec 16;307(25):1552–1557. doi: 10.1056/NEJM198212163072504. [DOI] [PubMed] [Google Scholar]
- Bichet D., Szatalowicz V., Chaimovitz C., Schrier R. W. Role of vasopressin in abnormal water excretion in cirrhotic patients. Ann Intern Med. 1982 Apr;96(4):413–417. doi: 10.7326/0003-4819-96-4-413. [DOI] [PubMed] [Google Scholar]
- Cody R. J., Haas G. J., Binkley P. F., Capers Q., Kelley R. Plasma endothelin correlates with the extent of pulmonary hypertension in patients with chronic congestive heart failure. Circulation. 1992 Feb;85(2):504–509. doi: 10.1161/01.cir.85.2.504. [DOI] [PubMed] [Google Scholar]
- Epstein M., Weitzman R. E., Preston S., DeNunzio A. G. Relationship between plasma arginine vasopressin and renal water handling in decompensated cirrhosis. Miner Electrolyte Metab. 1984;10(3):155–165. [PubMed] [Google Scholar]
- Floras J. S., Legault L., Morali G. A., Hara K., Blendis L. M. Increased sympathetic outflow in cirrhosis and ascites: direct evidence from intraneural recordings. Ann Intern Med. 1991 Mar 1;114(5):373–380. doi: 10.7326/0003-4819-114-5-373. [DOI] [PubMed] [Google Scholar]
- Gerbes A. L., Gülberg V., Waggershauser T., Holl J., Reiser M. Renal effects of transjugular intrahepatic portosystemic shunt in cirrhosis: comparison of patients with ascites, with refractory ascites, or without ascites. Hepatology. 1998 Sep;28(3):683–688. doi: 10.1002/hep.510280313. [DOI] [PubMed] [Google Scholar]
- Gerbes A. L., Møller S., Gülberg V., Henriksen J. H. Endothelin-1 and -3 plasma concentrations in patients with cirrhosis: role of splanchnic and renal passage and liver function. Hepatology. 1995 Mar;21(3):735–739. [PubMed] [Google Scholar]
- Henriksen J. H., Christensen N. J., Ring-Larsen H. Noradrenaline and adrenaline concentrations in various vascular beds in patients with cirrhosis. Relation to haemodynamics. Clin Physiol. 1981 Jun;1(3):293–304. doi: 10.1111/j.1475-097x.1981.tb00898.x. [DOI] [PubMed] [Google Scholar]
- Jalan R., Forrest E. H., Redhead D. N., Dillon J. F., Hayes P. C. Reduction in renal blood flow following acute increase in the portal pressure: evidence for the existence of a hepatorenal reflex in man? Gut. 1997 May;40(5):664–670. doi: 10.1136/gut.40.5.664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jalan R., Redhead D. N., Thomas H. W., Henderson N., O'Rourke K., Dillon J. F., Williams B. C., Hayes P. C. Mechanisms of changes in renal handling of sodium following transjugular intrahepatic portal systemic stent-shunt (TIPSS). Eur J Gastroenterol Hepatol. 1996 Nov;8(11):1111–1116. doi: 10.1097/00042737-199611000-00015. [DOI] [PubMed] [Google Scholar]
- KONTOS H. A., SHAPIRO W., MAUCK H. P., PATTERSON J. L., Jr GENERAL AND REGIONAL CIRCULATORY ALTERATIONS IN CIRRHOSIS OF THE LIVER. Am J Med. 1964 Oct;37:526–535. doi: 10.1016/0002-9343(64)90066-x. [DOI] [PubMed] [Google Scholar]
- KOWALSKI H. J., ABELMANN W. H. The cardiac output at rest in Laennec's cirrhosis. J Clin Invest. 1953 Oct;32(10):1025–1033. doi: 10.1172/JCI102813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lang F., Tschernko E., Schulze E., Ottl I., Ritter M., Völkl H., Hallbrucker C., Häussinger D. Hepatorenal reflex regulating kidney function. Hepatology. 1991 Oct;14(4 Pt 1):590–594. doi: 10.1016/0270-9139(91)90043-u. [DOI] [PubMed] [Google Scholar]
- Lieberman F. L., Ito S., Reynolds T. B. Effective plasma volume in cirrhosis with ascites. Evidence that a decreased value does not account for renal sodium retention, a sponteneous reduction in glomerular filtration rate (GFR), and a fall in GFR during drug-induced diuresis. J Clin Invest. 1969 Jun;48(6):975–981. doi: 10.1172/JCI106078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MURRAY J. F., DAWSON A. M., SHERLOCK S. Circulatory changes in chronic liver disease. Am J Med. 1958 Mar;24(3):358–367. doi: 10.1016/0002-9343(58)90322-x. [DOI] [PubMed] [Google Scholar]
- Martinet J. P., Legault L., Cernacek P., Roy L., Dufresne M. P., Spahr L., Fenyves D., Pomier-Layrargues G. Changes in plasma endothelin-1 and Big endothelin-1 induced by transjugular intrahepatic portosystemic shunts in patients with cirrhosis and refractory ascites. J Hepatol. 1996 Nov;25(5):700–706. doi: 10.1016/s0168-8278(96)80241-8. [DOI] [PubMed] [Google Scholar]
- Newby D. E., Jalan R., Masumori S., Hayes P. C., Boon N. A., Webb D. J. Peripheral vascular tone in patients with cirrhosis: role of the renin-angiotensin and sympathetic nervous systems. Cardiovasc Res. 1998 Apr;38(1):221–228. doi: 10.1016/s0008-6363(98)00008-x. [DOI] [PubMed] [Google Scholar]
- Niederberger M., Ginès P., Tsai P., Martin P. Y., Morris K., Weigert A., McMurtry I., Schrier R. W. Increased aortic cyclic guanosine monophosphate concentration in experimental cirrhosis in rats: evidence for a role of nitric oxide in the pathogenesis of arterial vasodilation in cirrhosis. Hepatology. 1995 Jun;21(6):1625–1631. [PubMed] [Google Scholar]
- Pariente E. A., Bataille C., Bercoff E., Lebrec D. Acute effects of captopril on systemic and renal hemodynamics and on renal function in cirrhotic patients with ascites. Gastroenterology. 1985 May;88(5 Pt 1):1255–1259. doi: 10.1016/s0016-5085(85)80088-3. [DOI] [PubMed] [Google Scholar]
- Quiroga J., Sangro B., Núez M., Bilbao I., Longo J., García-Villarreal L., Zozaya J. M., Betés M., Herrero J. I., Prieto J. Transjugular intrahepatic portal-systemic shunt in the treatment of refractory ascites: effect on clinical, renal, humoral, and hemodynamic parameters. Hepatology. 1995 Apr;21(4):986–994. [PubMed] [Google Scholar]
- Reznick R. K., Langer B., Taylor B. R., Seif S., Blendis L. M. Hyponatremia and arginine vasopressin secretion in patients with refractory hepatic ascites undergoing peritoneovenous shunting. Gastroenterology. 1983 Apr;84(4):713–718. [PubMed] [Google Scholar]
- Ryan J., Sudhir K., Jennings G., Esler M., Dudley F. Impaired reactivity of the peripheral vasculature to pressor agents in alcoholic cirrhosis. Gastroenterology. 1993 Oct;105(4):1167–1172. doi: 10.1016/0016-5085(93)90963-d. [DOI] [PubMed] [Google Scholar]
- SHERLOCK S., SHALDON S. The aetiology and management of ascites in patients with hepatic cirrhosis: a review. Gut. 1963 Jun;4:95–105. doi: 10.1136/gut.4.2.95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saló J., Francitorra A., Follo A., Navasa M., Ginès A., Jiménez W., Ginès P., Arroyo V., Rivera F., Rodés J. Increased plasma endothelin in cirrhosis. Relationship with systemic endotoxemia and response to changes in effective blood volume. J Hepatol. 1995 Apr;22(4):389–398. doi: 10.1016/0168-8278(95)80100-6. [DOI] [PubMed] [Google Scholar]
- Schrier R. W., Arroyo V., Bernardi M., Epstein M., Henriksen J. H., Rodés J. Peripheral arterial vasodilation hypothesis: a proposal for the initiation of renal sodium and water retention in cirrhosis. Hepatology. 1988 Sep-Oct;8(5):1151–1157. doi: 10.1002/hep.1840080532. [DOI] [PubMed] [Google Scholar]
- Schroeder E. T., Anderson G. H., Goldman S. H., Streeten D. H. Effect of blockade of angiotensin II on blood pressure, renin and aldosterone in cirrhosis. Kidney Int. 1976 Jun;9(6):511–519. doi: 10.1038/ki.1976.65. [DOI] [PubMed] [Google Scholar]
- Sellars L., Shore A. C., Wilkinson R., James O. F., Robson V. Sodium status and the renin-angiotensin-aldosterone system in compensated liver disease. Eur J Clin Invest. 1981 Aug;11(4):299–304. doi: 10.1111/j.1365-2362.1981.tb02120.x. [DOI] [PubMed] [Google Scholar]
- Stanley A. J., Forrest E. H., Dabos K., Bouchier I. A., Hayes P. C. Natriuretic effect of an adenosine-1 receptor antagonist in cirrhotic patients with ascites. Gastroenterology. 1998 Aug;115(2):406–411. doi: 10.1016/s0016-5085(98)70207-0. [DOI] [PubMed] [Google Scholar]
- Tajiri K., Miyakawa H., Izumi N., Marumo F., Sato C. Systemic hypotension and diuresis by L-arginine in cirrhotic patients with ascites: role of nitric oxide. Hepatology. 1995 Nov;22(5):1430–1435. [PubMed] [Google Scholar]
- Woitas R. P., Heller J., Stoffel-Wagner B., Spengler U., Sauerbruch T. Renal functional reserve and nitric oxide in patients with compensated liver cirrhosis. Hepatology. 1997 Oct;26(4):858–864. doi: 10.1002/hep.510260409. [DOI] [PubMed] [Google Scholar]
- Wong F., Logan A., Blendis L. The effect of varying sodium intake on blood volume, forearm blood flow and vascular responsiveness to sympathetic stimulation in pre-ascitic cirrhosis. Clin Invest Med. 1996 Jun;19(3):184–194. [PubMed] [Google Scholar]
- Wong F., Massie D., Colman J., Dudley F. Glomerular hyperfiltration in patients with well-compensated alcoholic cirrhosis. Gastroenterology. 1993 Mar;104(3):884–889. doi: 10.1016/0016-5085(93)91026-e. [DOI] [PubMed] [Google Scholar]
- Wong F., Massie D., Hsu P., Dudley F. Renal response to a saline load in well-compensated alcoholic cirrhosis. Hepatology. 1994 Oct;20(4 Pt 1):873–881. doi: 10.1002/hep.1840200415. [DOI] [PubMed] [Google Scholar]
- Wong F., Sniderman K., Blendis L. The renal sympathetic and renin-angiotensin response to lower body negative pressure in well-compensated cirrhosis. Gastroenterology. 1998 Aug;115(2):397–405. doi: 10.1016/s0016-5085(98)70206-9. [DOI] [PubMed] [Google Scholar]
- Wong F., Sniderman K., Liu P., Blendis L. The mechanism of the initial natriuresis after transjugular intrahepatic portosystemic shunt. Gastroenterology. 1997 Mar;112(3):899–907. doi: 10.1053/gast.1997.v112.pm9041252. [DOI] [PubMed] [Google Scholar]