Abstract
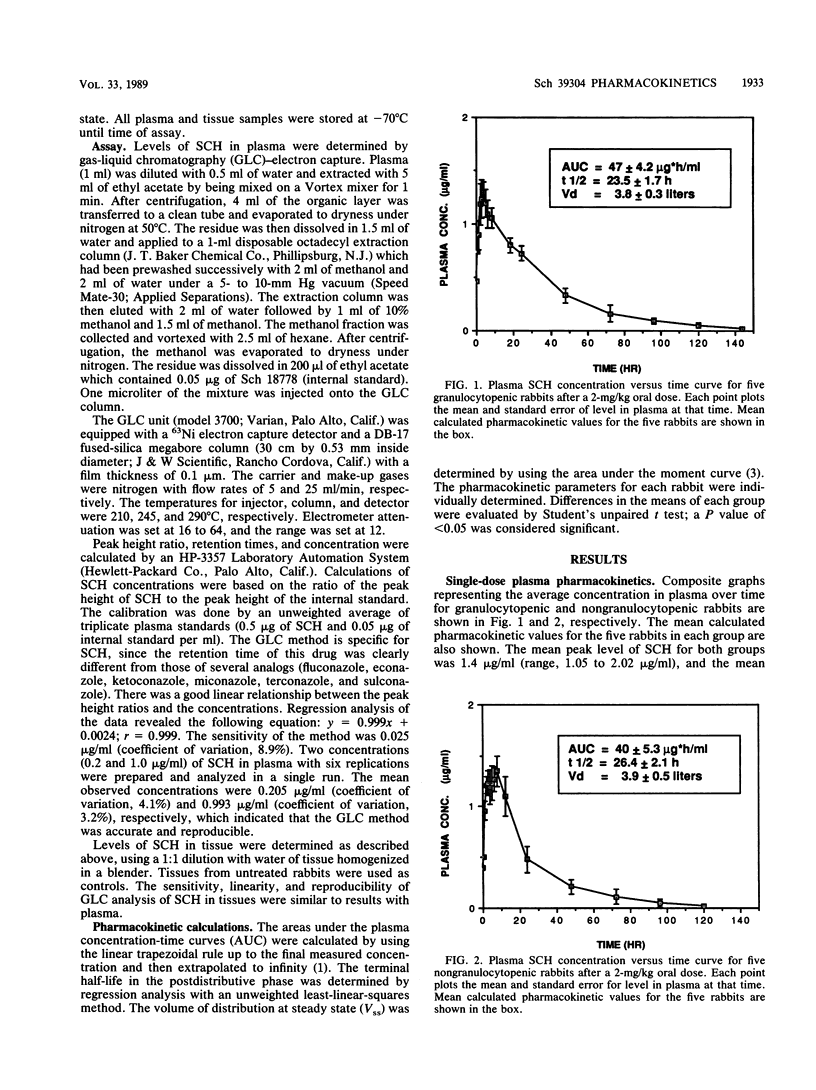
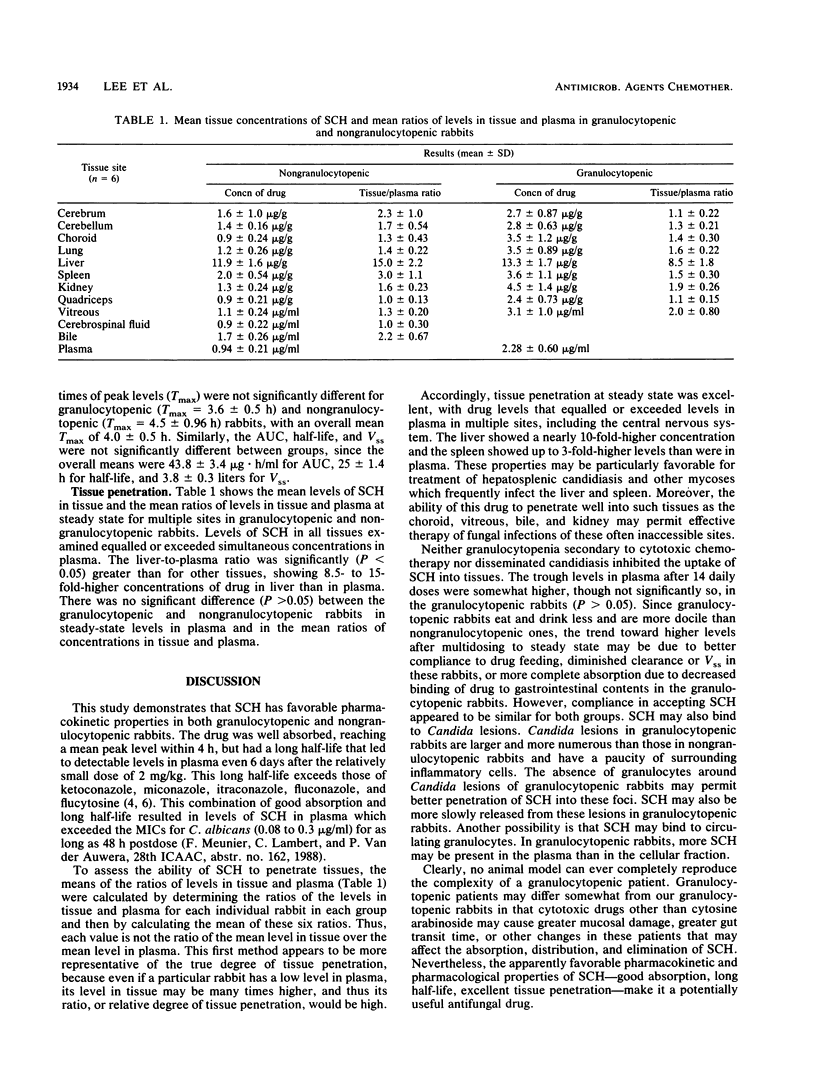
We studied the plasma pharmacokinetics and tissue penetration of Sch 39304 (SCH), a new antifungal triazole, in granulocytopenic [G(+)] and nongranulocytopenic [G(-)] rabbits. Five female New Zealand White G(-) rabbits were given a single oral dose of 2 mg of SCH per kg of body weight. Levels in plasma, determined by gas-liquid chromatography-electron capture, were obtained for 6 days. This procedure was repeated 2 weeks later with the same rabbits, which were induced and maintained G(+) with cytosine arabinoside. There were no significant differences between the pharmacokinetic parameters of G(+) and G(-) rabbits. Among all animals studied, the maximum concentration of the drug in plasma was 1.4 +/- 0.11 micrograms/ml at 4 +/- 0.5 h, the half-life was 25 +/- 1.4 h, the volume of distribution at steady state was 3.8 +/- 0.3 liters, and the area under the concentration-time curve was 44 +/- 3.4 micrograms.h/ml. SCH was detectable in plasma up to day 6. Levels of SCH in tissue were studied at steady state in six G(+) and six G(-) rabbits receiving 2 mg of the drug orally per kg per day for experimental disseminated candidiasis. Tissue SCH levels equalled or exceeded those in plasma (at steady state) at all sites examined, and these ratios were similar in both G(+) and G(-) rabbits. Thus, plasma pharmacokinetics of orally administered SCH were similar for G(+) and G(-) rabbits, and SCH achieved high levels of penetration into multiple tissues, including the liver and the central nervous system.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Hann I. M., Prentice H. G., Corringham R., Blacklock H. A., Keaney M., Shannon M., Noone P., Gascoigne E., Fox J., Boesen E. Ketoconazole versus nystatin plus amphotericin B for fungal prophylaxis in severely immunocompromised patients. Lancet. 1982 Apr 10;1(8276):826–829. doi: 10.1016/s0140-6736(82)91874-8. [DOI] [PubMed] [Google Scholar]
- Perrier D., Mayersohn M. Noncompartmental determination of the steady-state volume of distribution for any mode of administration. J Pharm Sci. 1982 Mar;71(3):372–373. doi: 10.1002/jps.2600710332. [DOI] [PubMed] [Google Scholar]
- Saag M. S., Dismukes W. E. Azole antifungal agents: emphasis on new triazoles. Antimicrob Agents Chemother. 1988 Jan;32(1):1–8. doi: 10.1128/aac.32.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walsh T. J., Bacher J., Pizzo P. A. Chronic silastic central venous catheterization for induction, maintenance and support of persistent granulocytopenia in rabbits. Lab Anim Sci. 1988 Aug;38(4):467–471. [PubMed] [Google Scholar]
- Walsh T. J., Pizzo A. Treatment of systemic fungal infections: recent progress and current problems. Eur J Clin Microbiol Infect Dis. 1988 Aug;7(4):460–475. doi: 10.1007/BF01962595. [DOI] [PubMed] [Google Scholar]


