Abstract
Aims—To provide an illustrated, detailed semiquantitative analysis of the important degenerative changes along the length of the vertebral artery so that pathologists faced with investigating a fatal arterial injury can identify important pre-existing wall abnormalities.
Methods—Ten transverse annuli were taken along 34 vertebral arteries from 17 subjects and stained sections were prepared using haematoxylin and eosin and the picro-sirius red method. After routine microscopy, the elastic fibres, collagen, and smooth muscle nuclei in the tunica media were quantified using an eyepiece graticule. An estimate of the severity and extent of elastic tissue fragmentation, collagenous scarring, and intimal thickening/atheroma was then undertaken.
Results—Smooth muscle counts remained constant along the artery but collagen counts were higher and elastic counts substantially lower within the intracranial segment. Elastic fibre fragmentation was recognised in infancy and was moderately advanced by early adulthood but considerable collagenous scarring developed later in life. Some individuals demonstrated severe fragmentation and scarring before the age of 35 years. The degenerative changes were often focal and spared the intracranial segment almost completely. Atheroma increased with age but was rarely severe and appeared not to worsen appreciably beyond the age of 40 years. An unusual arrangement of the collagenous tissue was described within the upper cervical loops.
Conclusion—Damaged vertebral arteries need to be sampled extensively to allow a proper histological assessment. The picro-sirius red method was successful in delineating the fine connective tissue structure of the wall and early degenerative changes. An understanding of the age and site specific changes should allow the pathologist to recognise important pre-existing abnormalities more easily.
Key Words: vertebral artery • picro-sirius red • degenerative change • injury
Full Text
The Full Text of this article is available as a PDF (284.4 KB).
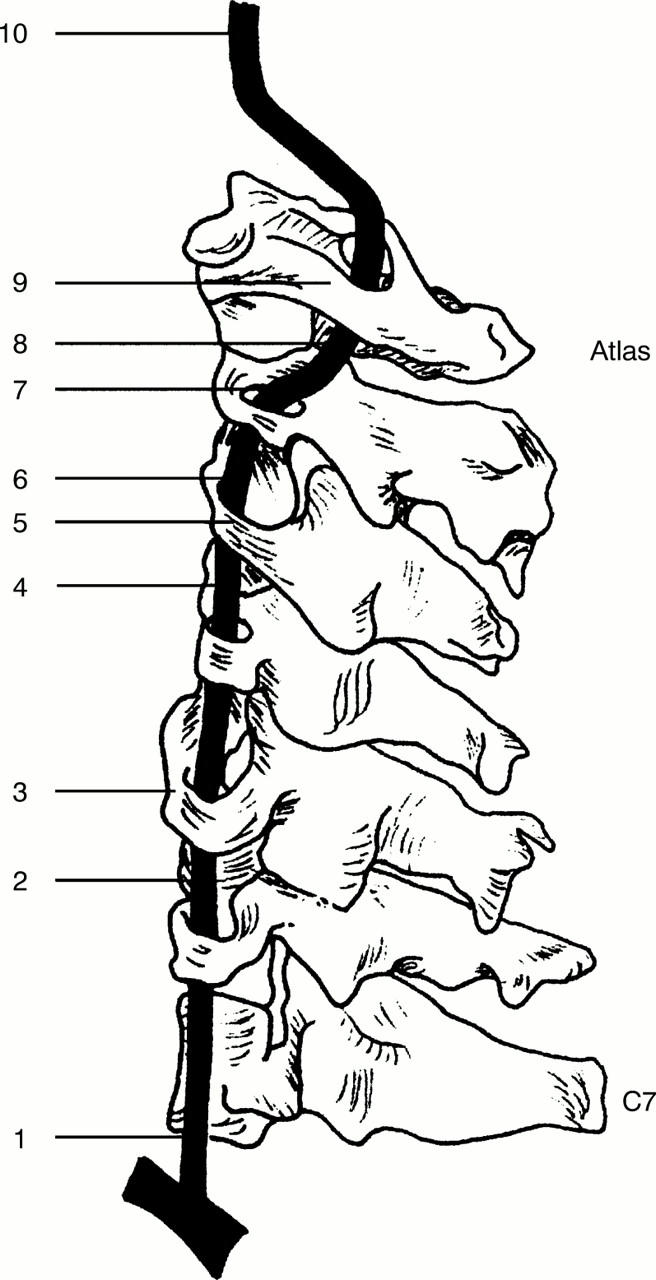
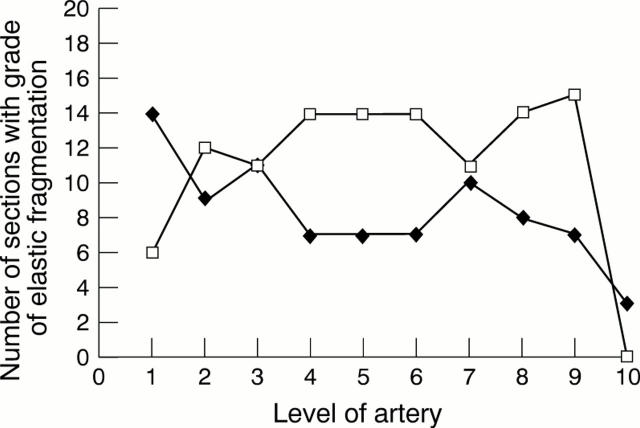
Figure 1 Sites from which the annuli were taken.
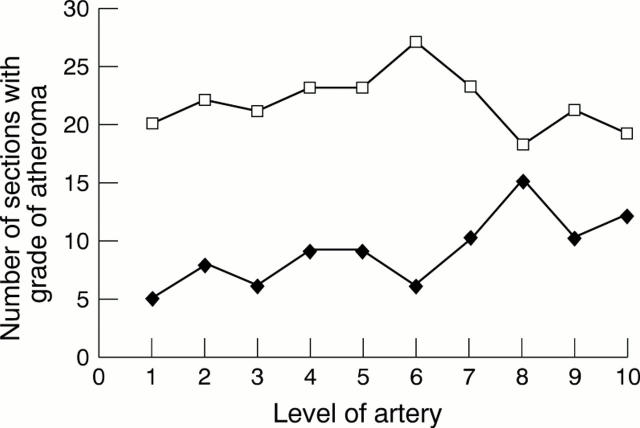
Figure 2 Graph showing lower grades of atheroma along the artery. Closed diamonds, A0, open squares, A1.
Figure 3 Graph showing higher grades of atheroma along the artery. Open squares, A2; closed circles, A3.
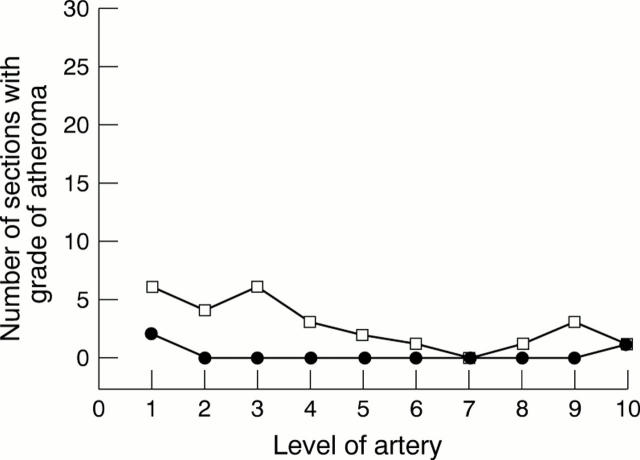
Figure 4 Graph showing the effect of age on the grade of atheroma. Closed squares, left artery; open diamonds, right artery.
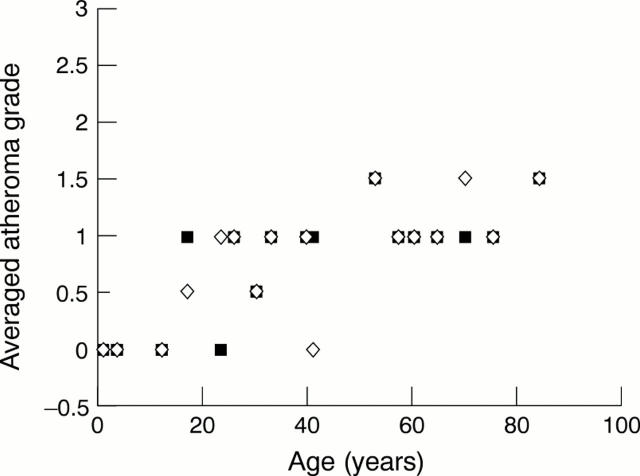
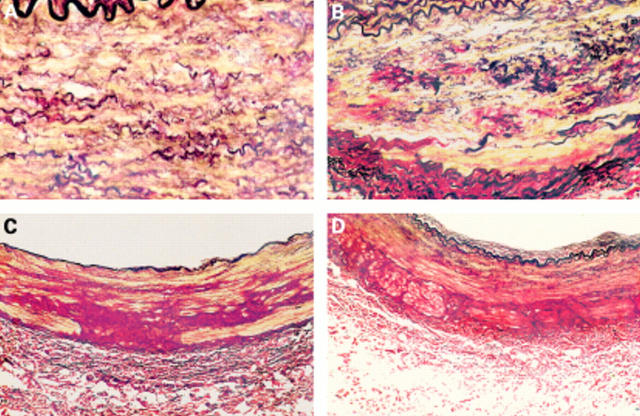
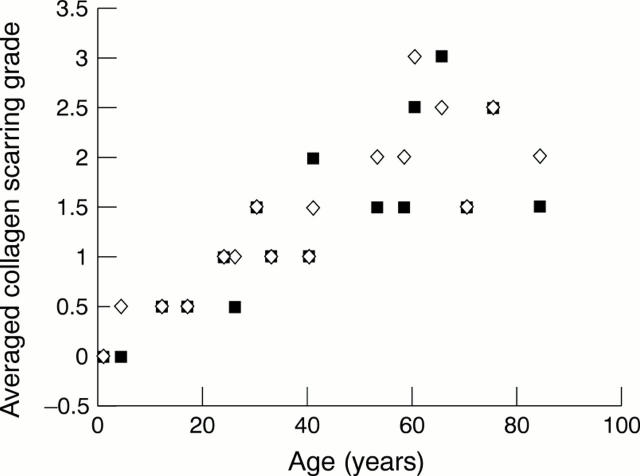
Figure 5 (A) Transverse extracranial vertebral artery section from a 9 month old child showing well formed internal and external elastic lamina, the circumferential arrangement of the elastic fibres, and an absence of fragmentation and scarring. (B) Extracranial vertebral artery section from a 4 year old child. Note the close relation between the elastic fibres and collagen. The fine architecture is evident as is the absence of fragmentation or scarring. (C) Section of extracranial vertebral artery from a 9 month old child showing early intimal thickening and obvious breaks in the internal elastic lamina. (D) Typical intracranial vertebral artery transverse section (age 12 years) showing very little elastic tissue in the tunica media and a poorly formed external elastic lamina (all stained with picro-sirius red).
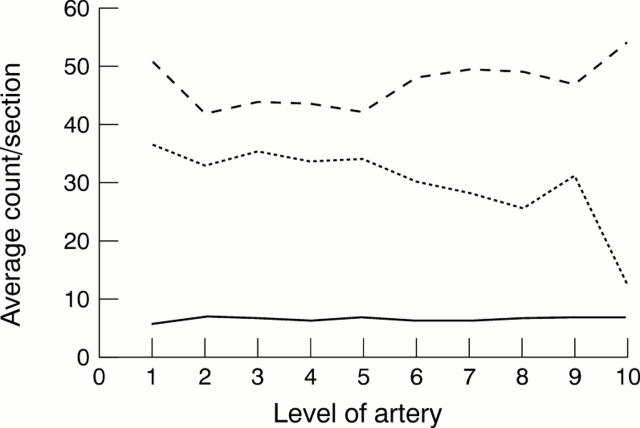
Figure 6 Graph showing the average count/section along the artery for elastic fibres (small dashes), collagen fibres (large dashes), and smooth muscle nuclei (continuous line). The changes along the vessel are clearly demonstrated and are most striking at the origin and as the vessel becomes intracranial.
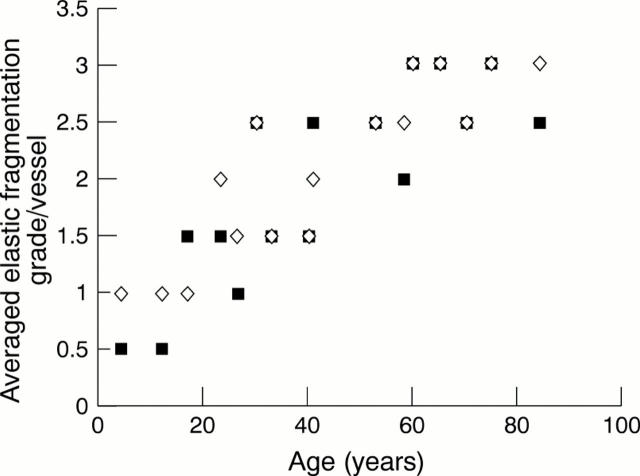
Figure 7 Graph showing the age related increase in elastic fibre fragmentation. Closed squares, left artery; open diamonds, right artery.
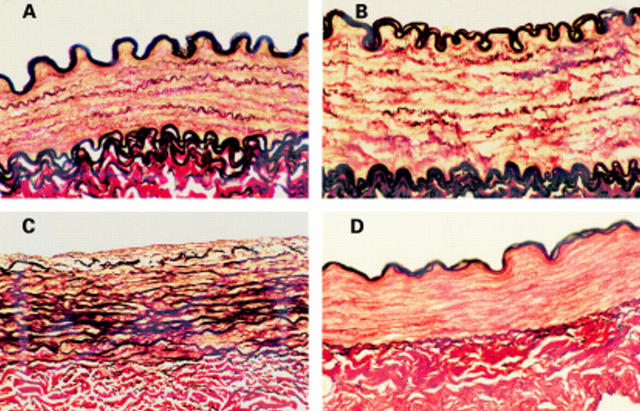
Figure 8 (A) Extracranial vertebral artery transverse section from a 17 year old subject, showing mild to moderate elastic fibre fragmentation (E1–E2). (B) Extracranial vertebral artery section from a 33 year old subject. Note the advanced elastic fibre fragmentation (E3) and severe collagen scarring (C3). (C) Transverse vertebral artery section from the upper cervical loop segment of a 30 year old subject. Note the very dense distribution of collagen extending from the adventitia into the media. (D) Transverse vertebral artery section from the upper cervical loop segment of a 33 year old subject. Again, note the unusual arrangement of peripheral collagen extending from the adventitia (all stained with picro-sirius red).
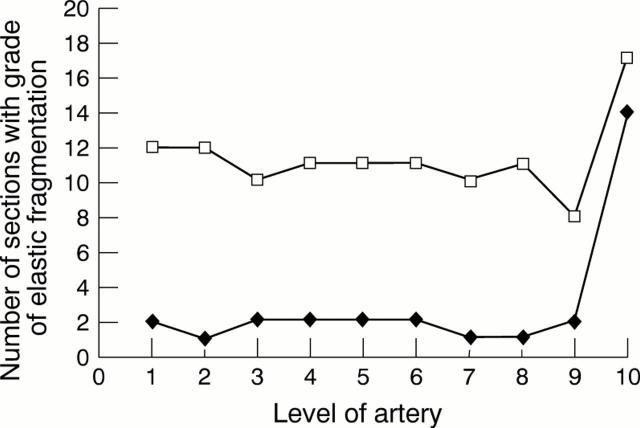
Figure 9 Graph showing the number of sections with lower grades of elastic fragmentation along the artery. Note the change as the vessel becomes intracranial (level 10). Closed diamonds, E0; open squares, E1.
Figure 10 Graph showing the number of sections with higher grades of elastic fragmentation along the artery. Note the change as the vessel becomes intracranial (level 10). Closed diamonds, E2; open squares, E3.
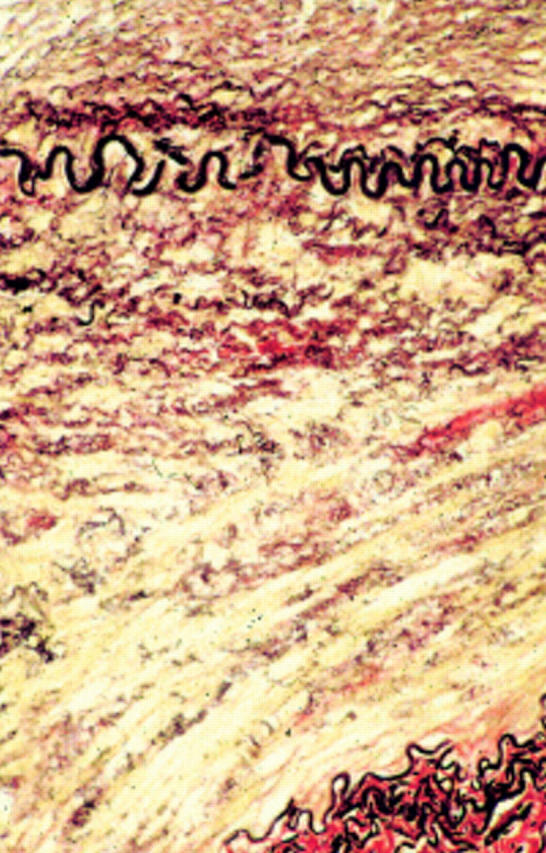
Figure 11 Transverse section of extracranial vertebral artery from a 60 year old subject showing moderate elastic fragmentation (E2) and two foci of early scarring (C1). (Stained with picro-sirius red.)
Figure 12 Graph showing age related increase in the severity of collagenous scarring. Closed squares, left artery; open diamonds, right artery.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Chopard R. P., de Miranda Neto M. H., Lucas G. A., Chopard M. R. The vertebral artery: its relationship with adjoining tissues in its course intra and inter transverse processes in man. Rev Paul Med. 1992 Nov-Dec;110(6):245–250. [PubMed] [Google Scholar]
- Coast G. C., Gee D. J. Traumatic subarachnoid haemorrhage: an alternative source. J Clin Pathol. 1984 Nov;37(11):1245–1248. doi: 10.1136/jcp.37.11.1245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Contostavlos D. L. Massive subarachnoid hemorrhage due to laceration of the vertebral artery associated with fracture of the transverse process of the atlas. J Forensic Sci. 1971 Jan;16(1):40–56. [PubMed] [Google Scholar]
- Dowling G., Curry B. Traumatic basal subarachnoid hemorrhage. Report of six cases and review of the literature. Am J Forensic Med Pathol. 1988 Mar;9(1):23–31. [PubMed] [Google Scholar]
- HUTCHINSON E. C., YATES P. O. The cervical portion of the vertebral artery; a clinico-pathological study. Brain. 1956 Jun;79(2):319–331. doi: 10.1093/brain/79.2.319. [DOI] [PubMed] [Google Scholar]
- Harland W. A., Pitts J. F., Watson A. A. Subarachnoid haemorrhage due to upper cervical trauma. J Clin Pathol. 1983 Dec;36(12):1335–1341. doi: 10.1136/jcp.36.12.1335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson C. P., Burns J. The medicolegal significance of proteoglycans in the tunica media of the vertebral artery. Am J Forensic Med Pathol. 1993 Jun;14(2):165–169. doi: 10.1097/00000433-199306000-00014. [DOI] [PubMed] [Google Scholar]
- Johnson C. P., Lawler W., Burns J. Use of histomorphometry in the assessment of fatal vertebral artery dissection. J Clin Pathol. 1993 Nov;46(11):1000–1003. doi: 10.1136/jcp.46.11.1000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson C. P., Scraggs M., How T., Burns J. A necropsy and histomorphometric study of abnormalities in the course of the vertebral artery associated with ossified stylohyoid ligaments. J Clin Pathol. 1995 Jul;48(7):637–640. doi: 10.1136/jcp.48.7.637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piffer C. R., Zorzetto N. L. Microscopy anatomy of the vertebral artery in the suboccipital and intracranial segments. Anat Anz. 1980;147(4):382–388. [PubMed] [Google Scholar]
- Pollanen M. S., Deck J. H., Boutilier L., Davidson G. Lesions of the tunica media in traumatic rupture of vertebral arteries: histologic and biochemical studies. Can J Neurol Sci. 1992 Feb;19(1):53–56. [PubMed] [Google Scholar]
- SIMONSEN J. Traumatic subarachnoid hemorrhage in alcohol intoxication. J Forensic Sci. 1963 Jan;8(1):97–116. [PubMed] [Google Scholar]
- Schlatmann T. J., Becker A. E. Histologic changes in the normal aging aorta: implications for dissecting aortic aneurysm. Am J Cardiol. 1977 Jan;39(1):13–20. doi: 10.1016/s0002-9149(77)80004-0. [DOI] [PubMed] [Google Scholar]
- Sherman M. R., Smialek J. E., Zane W. E. Pathogenesis of vertebral artery occlusion following cervical spine manipulation. Arch Pathol Lab Med. 1987 Sep;111(9):851–853. [PubMed] [Google Scholar]
- Simonsen J. Fatal subarachnoid haemorrhages in relation to minor injuries in Denmark from 1967 to 1981. Forensic Sci Int. 1984 Jan;24(1):57–63. doi: 10.1016/0379-0738(84)90152-x. [DOI] [PubMed] [Google Scholar]
- Vanezis P. Techniques used in the evaluation of vertebral artery trauma at post-mortem. Forensic Sci Int. 1979 Mar-Apr;13(2):159–165. doi: 10.1016/0379-0738(79)90280-9. [DOI] [PubMed] [Google Scholar]
- Vanezis P. Vertebral artery injuries in road traffic accidents: a post-mortem study. J Forensic Sci Soc. 1986 Jul-Aug;26(4):281–291. doi: 10.1016/s0015-7368(86)72496-1. [DOI] [PubMed] [Google Scholar]
- Wilkinson I. M. The vertebral artery. Extracranial and intracranial structure. Arch Neurol. 1972 Nov;27(5):392–396. doi: 10.1001/archneur.1972.00490170024004. [DOI] [PubMed] [Google Scholar]