Abstract
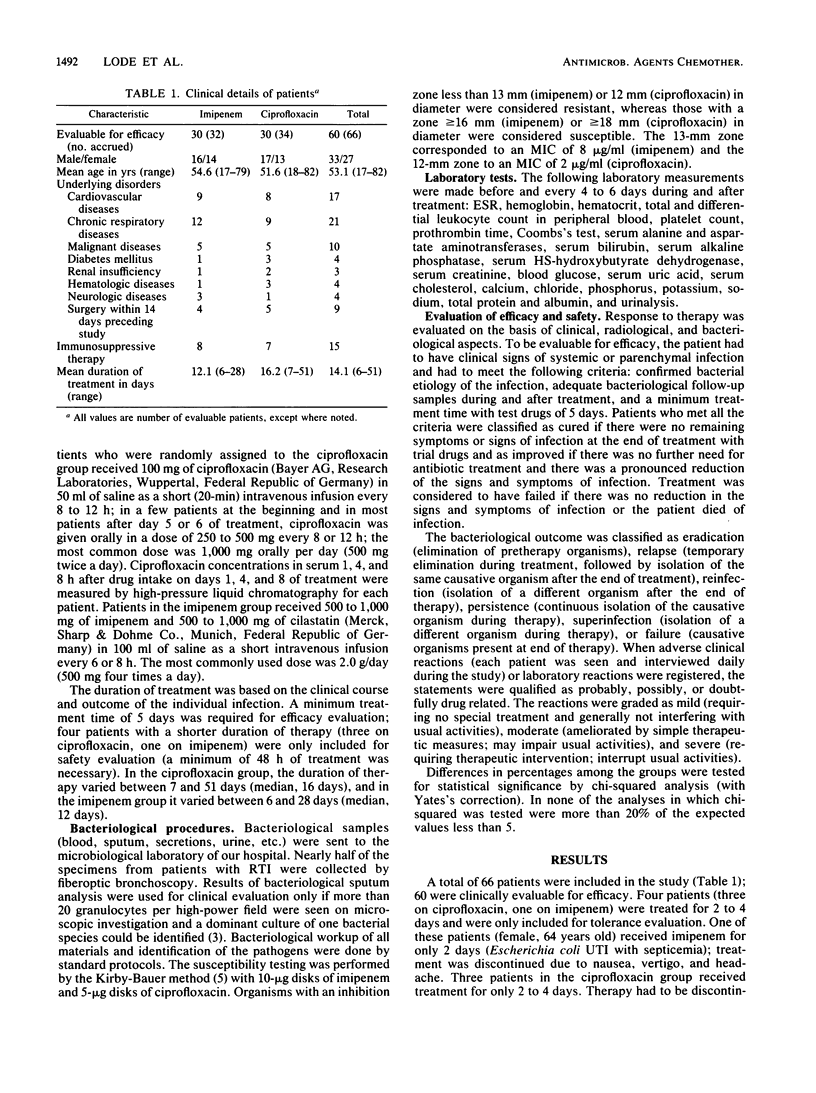
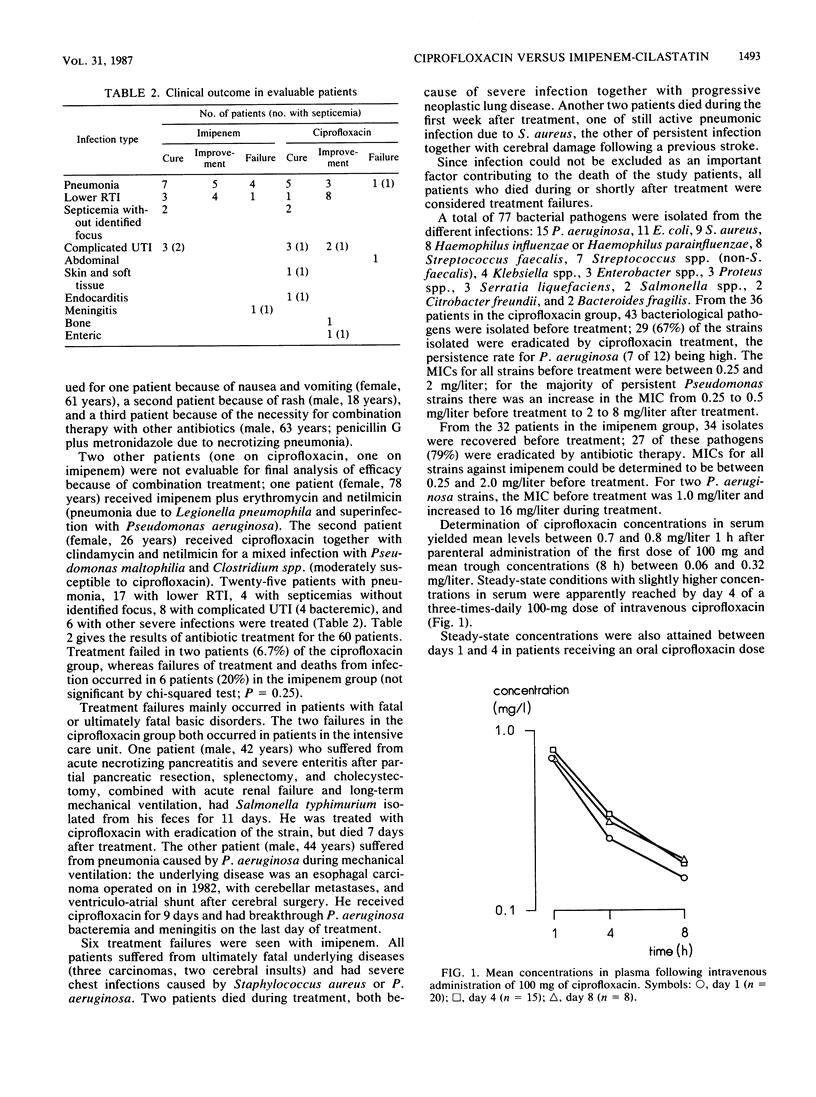
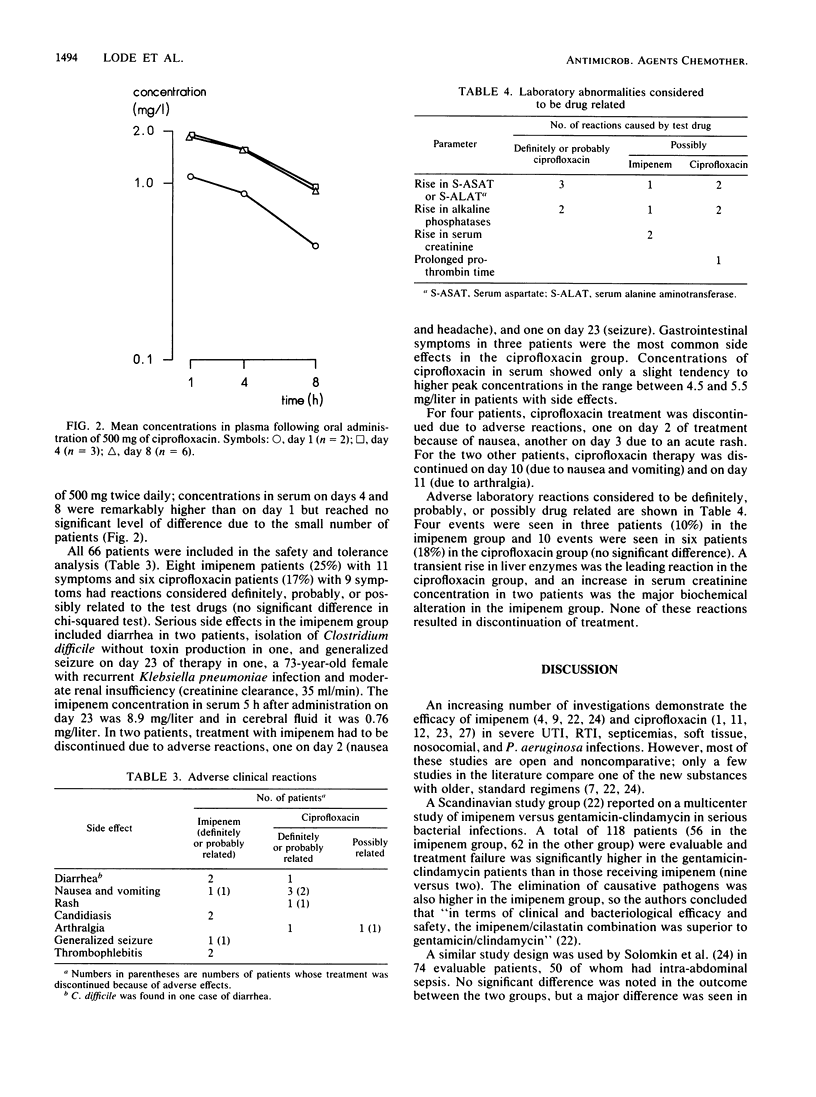
In a randomized prospective study, 66 patients with serious bacterial infections--mainly lower respiratory tract infections--were treated with either imipenem plus cilastatin (32 patients) or ciprofloxacin (34 patients); 30 patients in each group were evaluable for efficacy. Substantial underlying disease was present in most of the patients; pathogens isolated prior to treatment (77 isolates) consisted mainly of members of the family Enterobacteriaceae, Pseudomonas aeruginosa, Staphylococcus aureus, Haemophilus influenzae, and streptococci. Of the etiologic bacteria, 67% were eradicated by ciprofloxacin treatment and 79% by imipenem therapy; however, two patients (6.7%) failed in the ciprofloxacin group, and six patients (20%) did not respond to imipenem treatment (P = 0.25). All patients with therapeutic failures suffered from severe fatal underlying diseases, which had substantial impact on the outcome of treatment. Therapeutic drug monitoring in the ciprofloxacin patients revealed higher concentrations in serum at days 4 and 8 in comparison with day 1 of treatment, indicating that steady-state conditions were reached between days 1 and 4. The total number of side effects was relatively high--eight imipenem patients (25%) and six ciprofloxacin patients (18%) had reactions. Treatment had to be discontinued due to adverse reactions for three ciprofloxacin patients and two imipenem patients. Major side effects in both groups were gastrointestinal and central nervous system-related symptoms. In terms of clinical and bacteriological efficacy and safety, there was no statistical difference between the two groups, and both groups gave good to excellent results for bacterial infections that were difficult to treat.
Full text
PDF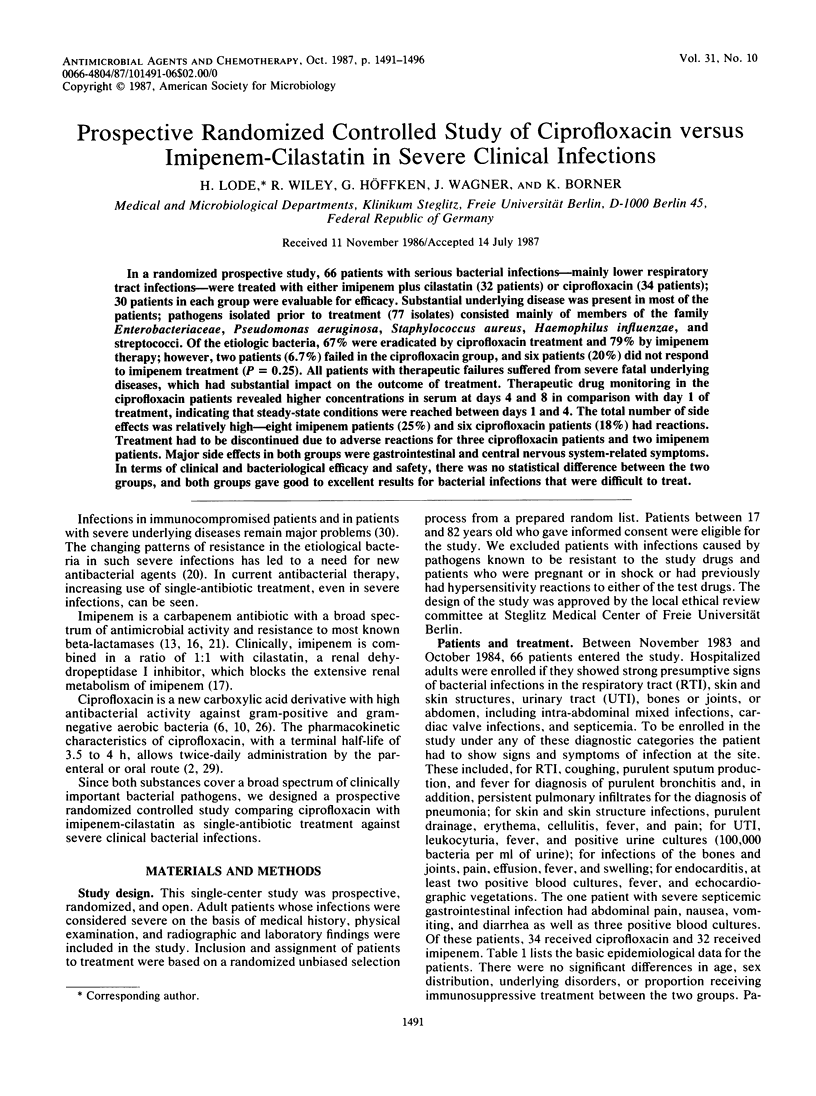
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Ball A. P., Fox C., Ball M. E., Brown I. R., Willis J. V. Pharmacokinetics of oral ciprofloxacin, 100 mg single dose, in volunteers and elderly patients. J Antimicrob Chemother. 1986 May;17(5):629–635. doi: 10.1093/jac/17.5.629. [DOI] [PubMed] [Google Scholar]
- Ball A. P. Overview of clinical experience with ciprofloxacin. Eur J Clin Microbiol. 1986 Apr;5(2):214–219. doi: 10.1007/BF02013993. [DOI] [PubMed] [Google Scholar]
- Barza M. Imipenem: first of a new class of beta-lactam antibiotics. Ann Intern Med. 1985 Oct;103(4):552–560. doi: 10.7326/0003-4819-103-4-552. [DOI] [PubMed] [Google Scholar]
- Bauer A. W., Kirby W. M., Sherris J. C., Turck M. Antibiotic susceptibility testing by a standardized single disk method. Am J Clin Pathol. 1966 Apr;45(4):493–496. [PubMed] [Google Scholar]
- Bauernfeind A., Petermüller C. In vitro activity of ciprofloxacin, norfloxacin and nalidixic acid. Eur J Clin Microbiol. 1983 Apr;2(2):111–115. doi: 10.1007/BF02001575. [DOI] [PubMed] [Google Scholar]
- Calandra G. B., Brown K. R., Grad L. C., Ahonkhai V. I., Wang C., Aziz M. A. Review of adverse experiences and tolerability in the first 2,516 patients treated with imipenem/cilastatin. Am J Med. 1985 Jun 7;78(6A):73–78. doi: 10.1016/0002-9343(85)90104-4. [DOI] [PubMed] [Google Scholar]
- Calandra G. B., Hesney M., Grad C. A multiclinic randomized study of the comparative efficacy, safety and tolerance of imipenem/cilastatin and moxalactam. Eur J Clin Microbiol. 1984 Oct;3(5):478–487. doi: 10.1007/BF02017380. [DOI] [PubMed] [Google Scholar]
- Eliopoulos G. M., Gardella A., Moellering R. C., Jr In vitro activity of ciprofloxacin, a new carboxyquinoline antimicrobial agent. Antimicrob Agents Chemother. 1984 Mar;25(3):331–335. doi: 10.1128/aac.25.3.331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ernst J. A., Sy E. R., Colon-Lucca H., Sandhu N., Rallos T., Lorian V. Ciprofloxacin in the treatment of pneumonia. Antimicrob Agents Chemother. 1986 Jun;29(6):1088–1089. doi: 10.1128/aac.29.6.1088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eron L. J., Harvey L., Hixon D. L., Poretz D. M. Ciprofloxacin therapy of infections caused by Pseudomonas aeruginosa and other resistant bacteria. Antimicrob Agents Chemother. 1985 Aug;28(2):308–310. doi: 10.1128/aac.28.2.308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanslo D., King A., Shannon K., Warren C., Phillips I. N-Formimidoyl thienamycin (MK0787): in-vitro antibacterial activity and susceptibility to beta-lactamases compared with that of cefotaxime, moxalactam and other beta-lactam antibiotics. J Antimicrob Chemother. 1981 Jun;7(6):607–617. doi: 10.1093/jac/7.6.607. [DOI] [PubMed] [Google Scholar]
- Johnson D. E., Calia F. M., Snyder M. J., Warren J. W., Schimpff S. C. Imipenem therapy of Pseudomonas aeruginosa bacteraemia in neutropenic rats. J Antimicrob Chemother. 1983 Dec;12 (Suppl 500):89–96. doi: 10.1093/jac/12.suppl_d.89. [DOI] [PubMed] [Google Scholar]
- Kesado T., Hashizume T., Asahi Y. Antibacterial activities of a new stabilized thienamycin, N-formimidoyl thienamycin, in comparison with other antibiotics. Antimicrob Agents Chemother. 1980 Jun;17(6):912–917. doi: 10.1128/aac.17.6.912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kropp H., Sundelof J. G., Hajdu R., Kahan F. M. Metabolism of thienamycin and related carbapenem antibiotics by the renal dipeptidase, dehydropeptidase. Antimicrob Agents Chemother. 1982 Jul;22(1):62–70. doi: 10.1128/aac.22.1.62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neu H. C. Antimicrobial activity, bacterial resistance, and antimicrobial pharmacology. Is it possible to use new agents cost-effectively? Am J Med. 1985 Jun 28;78(6B):17–22. doi: 10.1016/0002-9343(85)90358-4. [DOI] [PubMed] [Google Scholar]
- Neu H. C., Labthavikul P. Comparative in vitro activity of N-formimidoyl thienamycin against gram-positive and gram-negative aerobic and anaerobic species and its beta-lactamase stability. Antimicrob Agents Chemother. 1982 Jan;21(1):180–187. doi: 10.1128/aac.21.1.180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peters H. J. Comparison of intravenous ciprofloxacin and mezlocillin in treatment of complicated urinary tract infection. Eur J Clin Microbiol. 1986 Apr;5(2):253–255. doi: 10.1007/BF02014003. [DOI] [PubMed] [Google Scholar]
- Scully B. E., Neu H. C., Parry M. F., Mandell W. Oral ciprofloxacin therapy of infections due to Pseudomonas aeruginosa. Lancet. 1986 Apr 12;1(8485):819–822. doi: 10.1016/s0140-6736(86)90937-2. [DOI] [PubMed] [Google Scholar]
- Solomkin J. S., Fant W. K., Rivera J. O., Alexander J. W. Randomized trial of imipenem/cilastatin versus gentamicin and clindamycin in mixed flora infections. Am J Med. 1985 Jun 7;78(6A):85–91. doi: 10.1016/0002-9343(85)90106-8. [DOI] [PubMed] [Google Scholar]
- Strunk R. W., Gratz J. C., Maserati R., Scheld W. M. Comparison of ciprofloxacin with azlocillin plus tobramycin in the therapy of experimental Pseudomonas aeruginosa endocarditis. Antimicrob Agents Chemother. 1985 Sep;28(3):428–432. doi: 10.1128/aac.28.3.428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Caekenberghe D. L., Pattyn S. R. In vitro activity of ciprofloxacin compared with those of other new fluorinated piperazinyl-substituted quinoline derivatives. Antimicrob Agents Chemother. 1984 Apr;25(4):518–521. doi: 10.1128/aac.25.4.518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warns H., Lode H., Harnoss C. M., Kemmerich B., Koeppe P., Wagner J. Multiple dose pharmacokinetics and therapeutic results with ceftazidime. J Antimicrob Chemother. 1983 Jul;12 (Suppl A):235–240. doi: 10.1093/jac/12.suppl_a.235. [DOI] [PubMed] [Google Scholar]
- Wise R., Lockley R. M., Webberly M., Dent J. Pharmacokinetics of intravenously administered ciprofloxacin. Antimicrob Agents Chemother. 1984 Aug;26(2):208–210. doi: 10.1128/aac.26.2.208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zajac B. A., Fisher M. A., Gibson G. A., MacGregor R. R. Safety and efficacy of high-dose treatment with imipenem-cilastatin in seriously ill patients. Antimicrob Agents Chemother. 1985 May;27(5):745–748. doi: 10.1128/aac.27.5.745. [DOI] [PMC free article] [PubMed] [Google Scholar]


