Abstract
Objective To determine whether providing mothers of babies in neonatal intensive care units with audiotapes of their conversations with a neonatologist improves recall of information and psychological wellbeing.
Design Randomised, single blinded trial.
Setting Neonatal intensive care unit, North Queensland, Australia.
Participants 200 mothers of babies in a neonatal intensive care unit.
Interventions Mothers given (n=102) or not given (n=98) audiotapes of their conversations with a neonatologist.
Main outcome measures Recall of information, attitudes to and use of the tape, satisfaction with conversations, postnatal depression, anxiety, general health, and stress about parenting, at 10 days and four and 12 months.
Results 91% (n=93) of mothers in the tape group listened to the tape (once by day 10, twice by four months, and three times by 12 months; range 1-10). At 10 days and four months, mothers in the tape group recalled significantly more information about diagnosis, treatment, and outcome than mothers in the control group. At four months mothers in the tape group were 75% more likely to recall all of the information about treatment than mothers in the control group (59% v 34%; risk ratio 1.75, 95% confidence interval 1.27 to 2.4). Six mothers, all in the control group, could not recall their conversations. No statistically significant differences were found between the groups in satisfaction with conversations (10 days), postnatal depression and anxiety scores (10 days, four and 12 months), and stress about parenting (12 months).
Conclusion Providing the mothers of babies in neonatal intensive care units with audiotapes of conversations with a neonatologist enhanced their recall of information (up to four months). The taped conversations did not affect the mothers' wellbeing or satisfaction with the neonatologist.
Trial registration Australian Clinical Trials Registry 12606000478516.
Introduction
The parents of babies in neonatal intensive care units often do not recall information.1 2 3 4 Effective communication between doctors and parents underpins family centred care and is a key recommendation of the Bristol inquiry.1 5
Several studies have found that giving adults with cancer an audiotape of their initial conversations with oncologists improved their psychological distress, anxiety, satisfaction with conversations, and recall of information whereas other authors found no benefits.6 7 8 9 10 11 12 No reports exist on the effect of providing the mothers of babies in neonatal intensive care units with an audiotape of their conversations with the neonatologist.12 We carried out a randomised single blind trial to compare the effects of providing or not providing mothers of babies in neonatal intensive care units with an audiotape of their conversations with the neonatologist. We hypothesised that giving the mothers the tape would improve their recall of information and reduce psychological morbidity.
Methods
The neonatal intensive care unit at the Townsville Hospital, the regional neonatal unit for North Queensland, has three full time neonatologists and comprises 10 intensive care cots and 20 step-down cots. The unit looks after 150 ventilated babies a year.
Mothers were eligible for the study if their babies were admitted to the unit, they understood English or had an interpreter, and they consented to be recruited. We excluded mothers receiving psychiatric care or those whose baby needed to be transferred interstate during the first week of life.
The study was a randomised controlled trial of audiotape provision, with the neonatologist and neonatal team blinded to the participant's allocation. Before the first conversation the mothers completed a questionnaire eliciting personal details, anxiety scores, and preferences for information and involvement in decision making. The researcher then contacted a clinical trials centre randomisation service and the mother was allocated to receive or not to receive a copy of the taped conversations with a neonatologist. The randomisation schedule was generated using a computer sequence with variable blocks.
After randomisation the initial conversation and subsequent conversations of significance (as identified by the neonatologist—for example, babies with pneumothorax, patent ductus arteriosus needing treatment, necrotising enterocolitis, fits, cerebral injuries) were taped using a portable cassette recorder (PMD101; Marantz) and a copy retained for transcription and analysis. The mothers in the experimental arm received a tape of each of the conversations and a portable tape recorder (TCM-353; Sony).
Ten days and four months after the initial conversation the researcher carried out a structured interview with the mothers to document their recall of the diagnosis, tests, treatment, and outcome of their babies as conveyed by the neonatologist. Mothers also completed a questionnaire to ascertain views of the taping, use of the tapes, anxiety state, general health, depression, marital satisfaction, social support, and satisfaction with conversations held with the neonatologist.
At 12 months' follow-up mothers were sent the same questionnaire by post, with a stamped addressed envelope for return of the completed questionnaire. Non-respondents were telephoned a maximum of twice and contacted once by post.
Outcome measures
Recall of information was assessed by face to face or telephone interview. The interview opened with a broad question inviting mothers to report what the neonatologist had told them and their understanding of what that meant. If the answers were incomplete then five prompts followed on diagnosis, tests, treatment, and prognosis; responses were recorded on an interview form. Transcripts of each taped conversation were coded by a neonatologist (THHGK) to itemise the information in each category. The number of facts recalled by the mothers was expressed as a percentage of the total facts presented.9
We used the Spielberger state anxiety inventory to measure anxiety.13 Postnatal depression was measured with the 10 item Edinburgh postnatal depression scale, which assesses the intensity of depressive mood during the past seven days, with a cut-off score of 12.14 General psychological morbidity was assessed using the general health questionnaire-12 (0 scores for non-cases, 1 or greater for cases).15
The parental stress index, a self-report inventory with 101 items, measures the stress associated with a child's characteristics and with the parenting role.16 We summed the scores for each child and parent domain, with the total score being the sum of the two domains.
We used a 25 item five point Likert scale adapted from scales of proved sensitivity to tape provision to measure satisfaction with the conversation.17 This scale assesses satisfaction with the amount and quality of information presented, doctors' communication skills, and the extent of the patient's participation in the conversation.17
Satisfaction with the tape was measured using a scale based on usefulness of tapes to patients with cancer.18 We elicited information and preferences for involvement using a scale assessing the type and amount of information required and the level of involvement in decision making.19 Satisfaction with an intimate relationship was measured using the relational interaction satisfaction scale.20 For social support we used the six item Sarason social support questionnaire to assess the size of the support network (availability score) and satisfaction with support (satisfaction score).21
The clinical risk index for babies is a scoring system predicting mortality in hospital among high risk babies in neonatal intensive care units.22 Scores are given for birth weight, gestational age, maximum and minimum fraction of inspired oxygen and maximum base excess during the first 12 hours, and presence of congenital malformations. We documented severity of illness at birth and common neonatal complications.
Statistical analysis
We determined the study protocol a priori and collected and analysed the data on an intention to treat basis using SPSS version 10.0.5 for Windows (1999). Analyses were two tailed, with the significance set at 0.05.
For dichotomous variables we counted missing data as failures in the intervention group and successes in the control group whereas for continuous variables we set missing values to the mean of the other group.
We used linear and logistic multiple regression to analyse the effects of tape provision on mother's psychological outcomes, controlling for imbalances in baseline characteristics between the two groups. We prespecified subgroup analyses according to whether the babies had good or poor prognoses.
For recall of information (dichotomised as 100% recall or less than 100% recall) we calculated that a sample size of 100 mothers in each randomised group would be sufficient to detect differences as small as 20% between the groups at a 0.05 level of significance with 80% power.23 This calculation assumed that the percentage of mothers in the control group with 100% recall was 50%. We used 50% because there were no published studies to guide us, and 50% gave the largest sample size for a given absolute difference. A sample size of 100 in each group was also sufficient to detect mean differences of 0.3 of a standard deviation on the psychological adjustment and parent satisfaction measures, with a power of 80%.9
Results
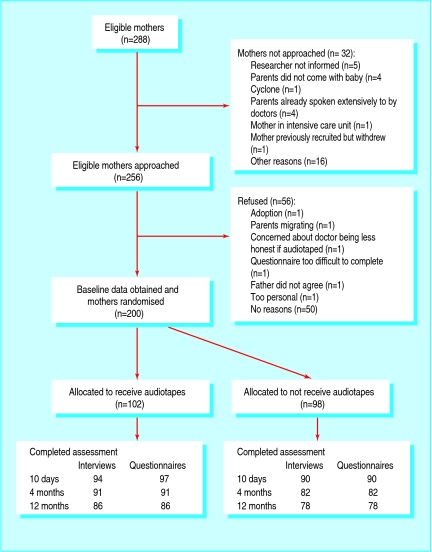
Between July 1999 and December 2001 288 mothers of babies admitted to the neonatal intensive care unit of Townsville Hospital, North Queensland, were eligible for the study. Thirty two mothers were not approached. Two hundred of the remaining 256 mothers (78%) agreed to participate. Overall 102 mothers were randomised to receive audiotapes of their conversations with a neonatologist and 98 mothers were randomised to no tape (figure).
Flow of participants through trial
No important differences were found between those mothers who refused to participate and those who accepted on variables for both the mothers and their babies except that for mothers who refused more were of Aboriginal descent (43% v 13%), parity was higher (3 v 2), fewer babies were born in the Townsville Hospital (29% v 65%), and the babies had fewer congenital abnormalities (7% v 15%).
Baseline characteristics of the mothers and babies were similar in both groups except that mothers randomised to receive the tape were more likely to have had less education than those in the control group (tables 1 and 2). Measures of mothers' baseline preferences for information and role in decision making, anxiety, and social support showed no significant differences between the groups. The modal number of conversations taped was one per mother (range 1-11), and no significant differences were found between the groups. Participation rates at follow up at 10 days and four and 12 months were up to 95%, 89%, and 84%.
Table 1.
Baseline characteristics of mothers with babies admitted to a neonatal intensive care unit provided with or without an audiotape of their conversations with a neonatologist. Values are numbers (percentages) of mothers unless stated otherwise
| Characteristics | Tape group (n=102) | Control group (n=98) | Significance |
|---|---|---|---|
| Mean (SD) age (years) | 28.1(5.3) | 27.2(5.8) | P=0.27, t=−1.1 |
| Ethnicity: | |||
| White | 86 (84) | 81 (83) | P=0.87, χ22=0.27 |
| Aboriginal and Torres Straits Islanders | 14 (14) | 14 (14) | |
| Asian | 2 (2) | 3 (3) | |
| Marital status: | |||
| Partner | 92 (90) | 86 (88) | P=0.58, χ21=0.3 |
| Single | 10 (10) | 12 (12) | |
| Education: | |||
| School certificate* | 21 (22) | 32 (38) | P=0.03, χ22=6.9 |
| Higher school certificate† | 41 (43) | 23 (27) | |
| Tertiary | 33 (35) | 30 (35) | |
| Parity: | |||
| 1 | 38 (38) | 45 (46) | P=0.29, χ22=2.4 |
| 2-4 | 57 (56) | 44 (45) | |
| ≥5 | 6 (6) | 8 (8) | |
| Mean (SD)state anxiety total score | 51.7 (15.1) | 51.3 (12.4) | P=0.81 |
| Gravida: | |||
| 1 | 29 (29) | 34 (35) | P=0.45, χ22=1.6 |
| 2-4 | 58 (57) | 47 (49) | |
| ≥5 | 14 (14) | 16 (17) | |
| Previous preterm deliveries: | |||
| No | 90 (88) | 75 (78) | P=0.06, χ21=3.6 |
| Yes | 12 (12) | 21 (22) | |
| In vitro fertilisation: | |||
| No | 100 (98) | 95 (97) | P=0.62, χ21=0.24 |
| Yes | 2 (2) | 3 (3) | |
| Caesarean section: | |||
| No | 40 (39) | 46 (47) | P=0.46, χ22=1.5 |
| Elective | 21 (21) | 15 (15) | |
| Emergency | 41 (40) | 37 (38) |
*School years 7-10.
†School years 11 and 12.
Table 2.
Baseline characteristics of babies admitted to a neonatal intensive care unit. Values are numbers (percentages) of babies unless stated otherwise
| Characteristics | Tape group (n=102) | Control group (n=98) | Significance |
|---|---|---|---|
| Male | 58 (57) | 65 (66) | P=0.17, χ21=1.89 |
| Female | 44 (43) | 33 (34) | |
| Mean (SD) gestational age (weeks) | 32.6 (0.48) | 33.6 (0.51) | t=1.5 |
| Mean (SD) birth weight (g) | 2114 (1122) | 2210 (1122) | t=0.6 |
| Plurality: | |||
| Singleton | 90 (88) | 92 (94) | P=0.38, χ22=1.9 |
| Twin | 10 (10) | 5 (5) | |
| Triplets | 1 (1) | 2 (2) | |
| Clinical risk index for babies score: | |||
| 0-5 | 79 (78) | 70 (71) | P=0.33, χ22=2.22 |
| 6-10 | 19 (19) | 26 (27) | |
| >10 | 4 (4) | 2 (2) | |
| Hyaline membrane disease: | |||
| None | 10 (10) | 15 (15) | P=0.17, χ22=3.5 |
| Mild | 20 (20) | 11 (11) | |
| Severe | 72 (71) | 72 (74) | |
| Sepsis: | |||
| No | 75 (74) | 66 (67) | P=0.34, χ21=0.9 |
| Yes | 27 (27) | 32 (33) | |
| No of days on ventilator: | |||
| 0-1 | 25 (25) | 28 (29) | P=0.33, χ23=3.4 |
| 2-3 | 37 (36) | 24 (25) | |
| 4-5 | 18 (18) | 19 (19) | |
| ≥6 | 22 (22) | 27 (28) | |
| No of days to reach full feeds: | |||
| 0-3 | 25 (25) | 23 (24) | P=0.50, χ23=2.3 |
| 4-7 | 30 (29) | 32 (33) | |
| 8-11 | 20 (20) | 12 (12) | |
| ≥12 | 27 (27) | 31 (32) | |
| Intraventricular haemorrhage: | |||
| None | 93 (91.2) | 91 (92.9) | P=0.91, χ22=19 |
| Grade I or II | 4 (4) | 3 (3) | |
| Grade III or IV | 5 (5) | 4 (4) | |
| Surgery: | |||
| None | 83 (81) | 80 (82) | P=0.88, χ22=0.25 |
| Simple | 9 (9) | 10 (10) | |
| Complex | 10 (10) | 8 (8) | |
| Outcome: | |||
| Died | 14 (14) | 9 (9) | P=0.56, χ22=0.03 |
| Alive, uncertain prognosis | 9 (9) | 8 (8) | |
| Alive, good prognosis | 79 (78) | 80 (82) | |
| Length of stay (days) in neonatal intensive care unit: | |||
| 0-9 | 21 (21) | 21 (21) | P=0.91, χ25=1.56 |
| 10-19 | 22 (22) | 25 (26) | |
| 20-29 | 17 (17) | 11 (11) | |
| 30-39 | 14 (14) | 14 (14) | |
| 40-49 | 9 (9) | 10 (10) | |
| ≥50 | 19 (19) | 17 (17) | |
| Apgar score at 5 minutes: | |||
| 0-3 | 3 (3) | 6 (6) | P=0.55, χ22=1.2 |
| 4-7 | 30 (29) | 27 (28) | |
| 8-10 | 69 (68) | 65 (66) |
Mothers' impressions of having conversations taped, and use of tapes
Most (84-98%) of the mothers in both groups responded that having their conversations with the neonatologist taped did not annoy or embarrass them or cause them to be anxious. Most (71-92%) of the mothers given the tapes stated that the taped conversations helped their understanding, reminded them of what had been said, and helped their family to understand and recall information.
After one week 86 of the 95 (91%) mothers who responded had listened to the tape. Eighty of 84 (95%) mothers at four months and 76 of 79 (96%) at 12 months had listened to the tape at any time since randomisation. Mothers listened to the tape a modal of once by10 days, twice by four months, and three times by 12 months (range 1-10 for each assessment time). Partners listened to the tape in 49% (n=44) of instances, grandparents in 7%, relatives or friends in 1%, and a mix of partner, grandparents, and relatives in 14%. By 12 months 7% of the tapes were not listened to by anyone else.
Recall of information and psychological morbidity
At 10 days and four months mothers in the tape group had significantly greater recall of information on the diagnosis or outcome of the baby and on tests or treatment, respectively (table 3). The difference between the two groups remained significant in multivariate analysis. Six mothers, all in the control group, could not recall any information.
Table 3.
Mothers having 100% recall about diagnosis, tests, treatment, and outcome of their babies in a neonatal intensive care unit, at 10 days and four months follow up, according to group. Values are numbers (percentages) unless stated otherwise
| Follow up | Tape group (n=102) | Control group (n=98) | Relative risk* (95% CI) | P value |
|---|---|---|---|---|
| 10 days: | ||||
| Diagnosis | 73 (72) | 52 (53) | 1.35 (1.08 to1.69) | 0.007 |
| Tests | 43 (42) | 39 (40) | 1.06 (0.63 to1.94) | 0.734 |
| Treatment | 64 (63) | 47 (48) | 1.83 (1.04 to 3.21) | 0.035 |
| Outcome | 84 (82) | 65 (66) | 1.24 (1.05 to 1.47) | 0.009 |
| 4 months: | ||||
| Diagnosis | 65 (64) | 49 (50) | 1.27 (0.99 to 1.63) | 0.05 |
| Tests | 45 (44) | 35 (36) | 1.35 (1.00 to 1.84) | 0.045 |
| Treatment | 60 (59) | 33 (34) | 1.75 (1.27 to 2.4) | 0.004 |
| Outcome | 82 (80) | 61 (62) | 1.29 (1.08 to 1.55) | 0.005 |
*Value greater than 1.0 indicates higher recall in tape group.
With and without adjustment for baseline differences, no differences were found between the two groups in the incidence of postnatal depression, anxiety scores, general psychological wellbeing, parenting stress, and satisfaction with conversation (tables 4 and 5).
Table 4.
Postnatal depression and psychological morbidity at follow-up in mothers of babies in a neonatal intensive care unit, according to group. Values are numbers (percentages) unless stated otherwise
| Measure | Tape group (n=102) | Control group (n=98) | Relative risk (95% CI) | P value |
|---|---|---|---|---|
| Edinburgh postnatal depression score >12*: | ||||
| 10 days | 48 (47) | 40 (41) | 1.15 (0.84 to 1.58) | 0.37 |
| 4 months | 13 (13) | 18 (18) | 0.9 (0.46 to 1.76) | 0.75 |
| 12 months | 12 (12) | 10 (10) | 1.15 (0.52 to 2.5) | 0.72 |
| General health questionnaire score >1†: | ||||
| 10 days | 66 (65) | 65 (66) | 0.99 (0.8 to 1.2) | 0.92 |
| 4 months | 41 (40) | 35 (36) | 1.13 (0.8 to 1.6) | 0.51 |
| 12 months | 23 (23) | 23 (24) | 0.96 (0.6 to 1.6) | 0.88 |
*Mothers with score >12 most likely to have a depressive illness and should be further assessed.
†0 score for non-cases, 1 or greater for cases of greater distress.
Table 5.
Psychometric outcomes, satisfaction with conversation, and parenting stress index
| Measure | Difference in means (95% CI) | P value | Adjusted difference in means (95% CI) | P value |
|---|---|---|---|---|
| State anxiety inventory score*: | ||||
| 10 days | 2.03 (−1.42 to 5.48) | 0.25 | 1.11 (−2.84 to 5.05) | 0.58 |
| 4 months | 2.04 (−0.86 to 4.96) | 0.167 | 2.94 (−0.39 to 6.27) | 0.08 |
| 12 months | 0.42 (−2.2 to 3.05) | 0.75 | −0.21 (−4.36 to 3.94) | 0.92 |
| Satisfaction with conversation† | 0.11 (−4.04 to 4.05) | 0.99 | 0.58 (−2.84 to 4.00) | 0.738 |
| Parental stress index‡: | ||||
| Child domain | 0.96 (0.52 to 1.77) | 0.90 | 0.62 (0.28 to 1.39) | 0.252 |
| Parental domain | 0.43 (0.12 to 1.62) | 0.230 | 0.92 (0.50 to 1.68) | 0.778 |
*Higher scores denote greater anxiety.
†Five point Likert scale; higher scores denote higher satisfaction.
‡Higher scores denote higher stress.
Impact of babies' outcome
For babies with a good outcome significantly more mothers in the tape group compared with the control group had 100% recall of information at 10 days of their babies' treatment or outcome and at four months of their babies' diagnosis, treatment, or outcome (table 6). For babies with a poor outcome no differences were found between the groups in recall of information at 10 days whereas at four months significantly more mothers in the tape group had 100% recall of information of their babies' treatment (table 6). No differences were found between the two groups in psychological wellbeing and parenting stress of mothers for babies with a poor outcome (table 7). Mothers of babies with a poor outcome in the tape group were, however, significantly more satisfied with the conversation (table 8).
Table 6.
Mothers with 100% recall of diagnosis, tests, treatment, and outcome of their babies in a neonatal intensive care unit, at 10 days and 4 months follow-up, according to babies' prognosis. Values are numbers (percentages) unless stated otherwise
| Measure | Tape group | Control group | Relative risk (95% CI) | P value |
|---|---|---|---|---|
| Babies with a good outcome (tape group n=79; control group n=81) | ||||
| 10 days: | ||||
| Diagnosis | 59 (75) | 41 (51) | 1.47 (1.15 to 1.89) | 0.002 |
| Tests | 32 (41) | 33 (41) | 0.32 (0.68 to 1.45) | 0.97 |
| Treatment | 52 (66) | 39 (48) | 1.37 (1.04 to 1.8) | 0.024 |
| Outcome | 68 (86) | 57 (70) | 1.22 (1.04 to 1.46) | 0.016 |
| 4 months: | ||||
| Diagnosis | 52 (66) | 42 (52) | 1.27 (0.98 to 1.65) | 0.07 |
| Tests | 36 (46) | 31 (38) | 1.19 (0.82 to 1.7) | 0.35 |
| Treatment | 48 (61) | 30 (37) | 1.6 (1.17 to 2.3) | 0.003 |
| Outcome | 67 (85) | 57 (70) | 1.20 (1.02 to 1.43) | 0.029 |
| Babies with a poor outcome (tape group n=23; control group n=17) | ||||
| 10 days: | ||||
| Diagnosis | 14 (61) | 11 (65) | 0.94 (0.58 to 1.52) | 0.804 |
| Tests | 11 (48) | 6 (35) | 1.35 (0.63 to 2.9) | 0.43 |
| Treatment | 12 (52) | 8 (47) | 1.1 (0.58 to 2.09) | 0.75 |
| Outcome | 16 (70) | 8 (48) | 1.48 (0.83 to 2.6) | 0.15 |
| 4 months: | ||||
| Diagnosis | 13 (57) | 7 (41) | 1.37 (0.70 to 2.69) | 0.34 |
| Tests | 9 (39) | 4 (24) | 1.66 (0.61 to 4.5) | 0.30 |
| Treatment | 12 (52) | 3 (18) | 2.96 (0.98 to 8.87) | 0.026 |
| Outcome | 8 (65) | 4 (24) | 2.8 (1.12 to 6.87) | 0.009 |
Table 7.
Psychological wellbeing and stress about parenting of mothers with babies in a neonatal intensive care unit with a poor outcome. Values are percentages (numbers) of mothers unless stated otherwise
| Measure | Tape group | Control group | Relative risk (95% CI) | P value |
|---|---|---|---|---|
| Edinburgh postnatal depression score >12*: | ||||
| 10 days | 60 (12/20) | 36 (5/14) | 1.68 (076 to 3.7) | 0.16 |
| 4 months | 33 (6/18) | 20 (2/12) | 0.64 (0.29 to 1.45) | 0.31 |
| 12 months | 19 (3/16) | 27 (3/11) | 0.69 (0.17 to 2.8) | 0.60 |
| General health questionnaire score >1†: | ||||
| 10 days | 79 (15/19) | 71 (10/14) | 1.1 (0.73 to 1.7) | 0.62 |
| 4 months | 56 (10/18) | 50 (6/12) | 1.1 (0.55 to 2.2) | 0.76 |
| 12 months | 40 (6/15) | 50 (6/12) | 0.8 (0.35 to 1.9) | 0.60 |
| Parenting stress index score >85%‡: | ||||
| Child domain | 40 (2/5) | 25 (2/8) | 1.6 (0.32 to 8.0) | 0.57 |
| Parents domain | 67 (1015) | 90 (9/10) | 0.74 (0.49 to 1.1) | 0.18 |
*Mothers with score >12 most likely to have a depressive illness and should be further assessed.
†0 score for non-cases, 1 or greater for cases of greater distress.
‡Score greater than 85% indicating greater stress.
Table 8.
Anxiety and satisfaction with conversation with a neonatologist of mothers with babies in a neonatal intensive care unit with a poor outcome
| Measure | Tape group (No of mothers) | Control group (No of mothers) | Significance |
|---|---|---|---|
| Mean (SD) state and anxiety inventory score: | |||
| 10 days | 48.0 (13.4) (n=20) | 43.9 (14.9) (n=14) | P=0.8, t=0.41 |
| 4 months | 39.3 (12.6) (n=20) | 35.3 (12.0) (n=14) | P=0.29, t=1.1 |
| 12 months | 34.73 (10.8) (n=19) | 33.4 (8.2) (n=13) | P=0.71, t=0.38 |
| Mean (95% CI) satisfaction with conversation | 115 (104 to 123.2) (n=19) | 100.5 (94.1 to 109.4) (n=14) | P=0.0051, χ21=7.8 |
Discussion
Providing the mothers of babies in a neonatal intensive care unit with an audiotape of their conversations with a neonatologist improved their recall of information at 10 days and at four months. The tapes did not influence parental wellbeing or stress about parenting. The mothers of babies with a poor outcome who received the tape were significantly more satisfied with the conversation.
Effective communication underpins family centred care in neonatal intensive care units.1 4 Interventions to improve mothers' understanding need to be cheap and simple and provide an opportunity for review of information.8
Two observational studies in neonatology reported the feasibility of taping conversations with parents and most of the neonatologists were happy for their conversations to be recorded.4 24
The mothers in our study attended a regional neonatal intensive care unit, were prospectively recruited, and were followed up to one year. The cohort included a racially and socioeconomically diverse sample of mothers whose babies had a wide spectrum of clinical conditions. The two groups had similar baseline characteristics. The incidence of postnatal depression at the three follow-up periods (10 days and four and 12 months) was similar to that reported among mothers with babies in neonatal intensive care units in another study, suggesting that our cohort is representative of such mothers.23
Most of the mothers in both groups were positive about having their conversations with the neonatologist taped. Overall, 96% of mothers listened to the tapes and found them helpful in recalling information. The tapes improved recall of information up to four months. That six of the mothers in the control group could not recall their conversations with the neonatologist has important medicolegal implications, especially when obtaining consent for treatment or participation in trials.3 25
The mothers of babies with poor outcome did not seem to be helped by the tapes at 10 days' follow-up; at four months, however, these mothers recalled significantly more information on the treatment and outcome of their babies compared with the control group. This may have been due to the mothers being in shock about their babies' condition at 10 days; the tapes allowed them to listen at home when they had had time to adjust to their situation. Mothers of babies with a poor outcome were significantly more satisfied with the conversation than mothers in the control group. The results need to be interpreted with caution, however, as the number of mothers with babies given a poor outcome was small.
No significant difference was found between the groups for postnatal depression, anxiety, psychological wellbeing, or parenting stress scores at 10 days and four and 12 months. Thus the benefits to recall do not seem to be associated with negative psychological effects.
The limitations of our study include a higher refusal rate for non-white mothers. No significant differences were, however, found between the groups in the proportion of mothers who were non-white. The trial involved three neonatologists so the results may be different with other neonatologists.
Assuming that mothers are well enough to discuss their situation, successful taping depends on three things: a good quality tape recorder; a quiet room in which to hold conversations between the mother and key health professionals; and use of updated, concise, and clear language, avoiding terms such as “certain” or “100% confident.” The doctor should make a copy of the tape for storage.
Suggestions for future research
Taping medical conversations has immense potential for research, education, and audit in neonatology (for example, discussing specific conditions such as extreme prematurity, Down's syndrome, antenatal counselling, postmortem results, seeking consent). Neonatologists need to follow oncologists and develop guidelines for the use of audiotaping.8 Future studies could focus on the fathers of babies, on the interaction between doctors and parents, and on whether doctors in neonatal intensive care units could benefit from listening to tapes of their conversations and receiving feedback on their communication skills.26
Conclusion
It is practical to tape conversations between the mothers of babies in neonatal intensive care units and neonatologists. In our study the tapes were listened to both by the mothers and by family members. At 10 days' and four months' follow-up the tapes improved the mothers' recall of information provided by the neonatologist and did not influence their wellbeing or stress about parenting. The mothers of babies with poor outcome who received the tapes were significantly more satisfied with the conversation than similar mothers in the control group.
What is already known on this topic
Parents of babies in a neonatal intensive care unit have problems recalling information
No randomised controlled trials have assessed the effects of providing parents with tapes of their conversations with neonatologists
What this study adds
Providing mothers of babies in neonatal intensive care units with tapes of conversations with neonatologists improves their recall of information
The tapes did not affect the mothers' wellbeing or satisfaction with the neonatologist
We thank the mothers and health professionals at the Institute of Women's and Children's Health, Townsville Hospital, for their support.
Contributors: THHGK initiated, organised, and supervised the study and cross checked the data; he is the guarantor. THHGK, MC, and PNB analysed the data. THHGK, PNB, and MHT contributed to the study design. THHGK, PB, DB, LC, and JW helped carry out the trial. THHGK, PNB, MC, and MHT contributed to the paper, interpretation of data, and subsequent revisions of the manuscript.
Funding: THHGK, PNB, DB, LC, JW, and MHT were supported by grants from the Royal Children's Hospital Foundation/Golden Casket, Brisbane and the Townsville health district.
Competing interests: None declared.
Ethical approval: This study was approved by Townsville health district ethics committee.
References
- 1.Harrison H. The principles for family-centered neonatal care. Pediatrics 1993;92:643-50. [PubMed] [Google Scholar]
- 2.Kmietowicz Z. Premature baby was not put on ventilator. BMJ 1996;313:963. [DOI] [PubMed] [Google Scholar]
- 3.Learning from Bristol: the Department of Health response to the report of the public enquiry into children's heart surgery at the Bristol Royal Infirmary 1984-1995. Norwich: Stationery Office, 2002:136.
- 4.Koh TH, Jarvis C. Promoting effective communication in neonatal intensive care units by audiotaping doctor-parent conversations. Int J Clin Pract 1998;52:27-9. [PubMed] [Google Scholar]
- 5.Coulter A. After Bristol: putting patients at the centre. BMJ 2002;324:648-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Butt HR. A method for better physician-patient communication. Ann Intern Med 1977;86:478-80. [DOI] [PubMed] [Google Scholar]
- 7.Scott JT, Harmsen M, Prictor MJ, Entwistle VA, Sowden AJ, Watt I. Recordings or summaries of conversations for people with cancer. Cochrane Database Syst Rev 2003;(2):CD001539. [DOI] [PubMed]
- 8.Tattersall MH, Butow PN. Conversation audio tapes: an underused cancer patient information aid and clinical research tool. Lancet Oncol 2002;3:431-7. [DOI] [PubMed] [Google Scholar]
- 9.Ong LM, Visser MR, Lammes FB, van Der Velden J, Kuenen BC, de Haes JC. Effect of providing cancer patients with the audiotaped initial conversation on satisfaction, recall, and quality of life: a randomized, double-blind study. J Clin Oncol 2000;18:3052-60. [DOI] [PubMed] [Google Scholar]
- 10.Hogbin B, Jenkins VA, Parkin AJ. Remembering ‘bad news' consultations: an evaluation of tape-recorded consultations. Psycho-Oncology 1992;1:147-54. [Google Scholar]
- 11.McHugh P, Lewis S, Ford S, Newlands E, Rustin G, Coombes C, et al. The efficacy of audiotapes in promoting psychological well-being in cancer patients: a randomised, controlled trial. Brit J Cancer 1995;71:388-92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Koh THHG, Budge D, Butow P, Renison B, Woodgate P. Audio recordings of conversations with doctors for parents of critically sick babies. Cochrane Database Syst Rev 2005;(1):CD004502. [DOI] [PubMed]
- 13.Spielberger CD, Gorsuch RL, Lushene RE. Manual for the state-trait anxiety inventory. Palo Alto, CA: Consulting Psychologists Press, 1970.
- 14.Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh postnatal depression scale. Br J Psychiatry 1987;150:782-6. [DOI] [PubMed] [Google Scholar]
- 15.Goldberg DP, Hillier VF. A scaled version of the general health questionnaire. Psychol Med 1979;9:139-45. [DOI] [PubMed] [Google Scholar]
- 16.Abidin RR. Parenting stress index-manual. Charlottesville, VA: Pediatric Psychology Press, 1990.
- 17.Brown R, Dunn S, Butow P. Meeting patient expectations in the cancer conversation. Ann Oncol 1997;8:877-82. [DOI] [PubMed] [Google Scholar]
- 18.Tattersall MH, Butow PN, Griffin AM, Dunn SM. The take-home message: patients prefer conversation audiotapes to summary letters. J Clin Oncol 1994;12:1305-11. [DOI] [PubMed] [Google Scholar]
- 19.Cassileth BR, Zupkis RV, Sutton-Smith K, March V. Information and participation preferences among cancer patients. Ann Intern Med [DOI] [PubMed] [Google Scholar]
- 20.Buunk BP. Relationship interaction satisfaction scale. In: Touliatos J, Perlmutter BF, Straus MA, eds. Handbook of family measurement techniques. Newbury Park, CA: Sage, 1990:106-7.
- 21.Sarason I, Sarason B, Shearin E, Pierce G. A brief measure of social support: practical and theoretical implications. J Soc Pers Relat 1987;4:497-510. [Google Scholar]
- 22.Anon. CRIB (clinical risk index for babies), mortality, and impairment after neonatal intensive care. Scottish Neonatal Consultants' Collaborative Study Group and the International Neonatal Network. Lancet 1995;345:1020-2. [PubMed] [Google Scholar]
- 23.Hagan R, Evans SF, Pope S. Preventing postnatal depression in mothers of very preterm infants: a randomised controlled trial. Brit J Obstetr Gynaecol 2004;111:641-7. [DOI] [PubMed] [Google Scholar]
- 24.Watkinson M. Does tape recording the disclosure of Down's syndrome help parents? J Reprod Infant Psychol 1994;12:1-4. [Google Scholar]
- 25.Snowdon C, Garcia J, Elbourne D. Making sense of randomization; responses of parents of critically ill babies to random allocation of treatment in a clinical trial. Soc Sci Med 1997;45:1337-55. [DOI] [PubMed] [Google Scholar]
- 26.Fallowfield L, Lipkin JM, Hall A. Teaching senior oncologists communication skills: results from phase I of a comprehensive longitudinal program in the UK. J Clin Oncol 1998;16:1961-8. [DOI] [PubMed] [Google Scholar]