Abstract
Four cases of young patients with acute myocardial infarction are discussed in which urgent angiography showed large intracoronary thrombus and TIMI (thrombolysis in myocardial infarction) flow ≥ 2 in the infarct related artery. The rest of the coronary tree appeared to be free of detectable atherosclerosis. Percutaneous transluminal coronary angioplasty was not performed and an aggressive antiplatelet/anticoagulant treatment was administered (acetylsalicylic acid, clopidogrel, abciximab, and heparin). In all cases early angiographic control (1–12 days after AMI) showed disappearance of thrombus, no significant residual stenosis, and normal flow. No deterioration of left ventricular function was observed and the clinical course both in hospital and at five months’ follow up was uneventful.
Keywords: myocardial infarction, coronary thrombosis, primary PTCA, thrombolysis
Acute myocardial infarction (AMI) is a clinical syndrome characterised by acute occlusion of a coronary artery caused mainly by the development of a thrombus on the substrate of various types of atherosclerotic plaque (often moderately impairing the arterial lumen). Occlusion of the culprit coronary artery is a dynamic process in which phases of spontaneous recanalisation can occur as a result of transient, partial thrombus dissolution.1,2 Early reperfusion of the infarct related artery has proven to lead to a dramatically improved prognosis. Aspirin with thrombolytic drugs (perhaps in conjunction with glycoprotein IIb/IIIa inhibitors3) is highly effective in restoring flow in infarct related arteries. On the other hand, the improvement in percutaneous intervention techniques has made percutaneous transluminal coronary angioplasty (PTCA) the most effective tool to achieve a correct flow in patients with AMI and it is recommended for such patients when a skilled team is available.4 Within the spectrum of clinical and angiographic presentations of patients with AMI, it is possible that different subgroups of patients have more to gain with one of these (medical versus PTCA) reperfusion strategies.
To date, no data are available concerning the optimal strategy to be adopted when the thrombus is large, the atherosclerotic burden is small, and the flow through the culprit lesion is good. In such conditions, because of the risk of no reflow associated with PTCA, antithrombotic medical treatment may be more beneficial.
Here we present and discuss four cases of young patients with evolving myocardial infarction referred for primary or rescue PTCA who were successfully managed medically after angiographic documentation of an infarct related artery with a large thrombus, grade ≥ 2 TIMI (thrombolysis in myocardial infarction) flow, and absence of detectable atherosclerosis in the rest of the coronary tree.
CASE REPORTS
Characteristics of patients and medical treatment
From August 1999 to May 2000 four young (35–47 years) patients with AMI referred to the catheterisation laboratory within eight hours after symptom onset for urgent coronary angiography were not treated with PTCA and were managed with an aggressive medical treatment.
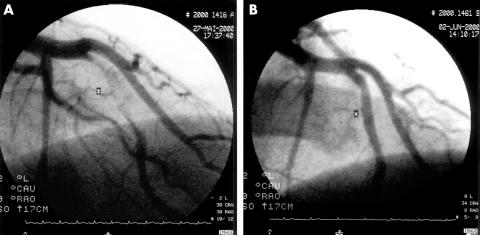
Table 1 lists the clinical characteristics of each of the four patients. None of them had a history of coronary artery disease. All the patients had ongoing chest pain (with a trend towards reduction) and persistent ST elevation in two or more contiguous leads. In all cases a single lesion was present in a coronary tree free of detectable angiographic narrowing. The culprit lesion consisted of a large intraluminal thrombus (thrombus score ≥ 2; fig 1A). TIMI flow grade in the infarct related arteries was ≥ 2. Table 1 shows the location of the culprit lesion, TIMI flow,5 and thrombus score6 at the emergency angiography for each patient.
Table 1.
Patients’ characteristics and medical treatment
| Case 1 | Case 2 | Case 3 | Case 4 | |
| Age (years) | 47 | 36 | 44 | 35 |
| Sex | Female | Male | Female | Female |
| Risk factors | ||||
| Familial history | No | No | No | No |
| Hypertension | No | Yes | No | No |
| Hypercholesterolaemia | No | No | No | No |
| Diabetes | Type I | No | No | No |
| Smoking | No | No | No | Yes |
| History of other disease(s) | No | No | Heterozygous for prothrombin G20210A gene polymorphism | Varicose veins in the left leg |
| Leads with ST elevation at ECG on admission | V1–V5 | V2–V6 | V4–V6, DI, aVL | DII, DIII, aVF |
| Site of culprit lesion | Mid-LAD | Proximal LAD | Proximal LAD | Mid-RCA |
| Angiographic features of infarct related artery | ||||
| TIMI flow | 2 | 2 | 3 | 3 |
| Thrombus score | 3 | 2 | 2 | 3 |
| Antithrombotic treatment | ||||
| Acetylsalicylic acid (500 mg bolus intravenously followed by 250 mg/day orally) | Yes | Yes | Yes | Yes |
| rt-PA (before angiography) | Yes | Yes | No | No |
| Abciximab (bolus 0.25 mg/kg intravenously plus 12 hours infusion 0.125 mg/kg/min intravenously) | Yes | Yes | Yes | Yes |
| Unfractionated heparin (infusion for 48 hours followed by low molecular weight heparin subcutaneously for 15 days) | Yes | Yes | Yes | Yes |
| Clopidogrel (loading dose of 300 mg orally followed by 75 mg/day orally) | Yes | Yes | Yes | Yes |
LAD, left anterior descending artery; RCA, right coronary artery; rt-PA, recombinant tissue type plasminogen activator; TIMI, thrombolysis in myocardial infarction.
Figure 1.
Mid-left anterior descending artery (right anterior oblique caudal view) in case 1 during the acute myocardial infarction (A) and in the control angiography after six days (B). *Site of the thrombus containing lesion.
PTCA was not performed and aggressive anticoagulant (unfractionated heparin followed by low molecular weight heparin) and antiplatelet (acetylsalicylic acid, clopidogrel, and abciximab) treatment was administered to obtain thrombus resolution (table 1). The angiographic assessment was repeated after 1–12 days and showed in all cases disappearance of the thrombus (fig 1B), normal anterograde flow, and no significant residual stenosis.
In-hospital course and follow up
The in-hospital course was uneventful for all of the patients. Mean peak creatine kinase concentration was 1698 IU/l and the mean time to peak creatine kinase concentration was 14 hours. Left ventricular ejection fraction, evaluated angiographically (in two cases) or echocardiographically (in the remaining two), was > 50% in all patients. The patients were discharged after a mean of 10 days (range 7–13 days).
A clinical follow up was performed at five months by telephone interview. No event occurred after discharge and the non-invasive tests showed absence of inducible myocardial ischaemia.
DISCUSSION
Medical treatment with thrombolytic drugs (and possibly with glycoprotein IIb/IIIa inhibitors) and coronary angioplasty are the best available treatments to restore patency of infarct related arteries during the acute phase of myocardial infarction. The target of both these strategies is to improve prognosis by achieving a normal flow in the infarct related artery. PTCA also reduces coronary reocclusion rates.7
In the present report we describe a relatively rare finding in the setting of urgent coronary angiography for evolving myocardial infarction: the presence of an angiographic pattern indicative of large intraluminal thrombus (thrombus score 2 or 3) without critical impairment of the anterograde flow (TIMI 2 or 3) in a coronary tree free of detectable atherosclerosis. In this setting the optimal medical or interventional strategy is unknown. Indeed, because of the characteristics of thrombus rich target lesions,8 the use of angioplasty could have led to flow deterioration and impairment of adjacent side branches, as well as to an appreciable restenosis rate. Moreover, when urgent angiography shows good flow in the infarct related artery, a watchful conservative treatment can be adopted.9 On the other hand, because of the dynamic process of thrombus formation and dissolution during acute coronary syndromes,1,2 the choice of a conservative strategy can increase the risk of deterioration of coronary flow through the lesion in the following hours to days. This may occur especially in patients with a high degree of coronary stenosis even in the presence of TIMI 3 flow.10
In the four cases reported, we were prompted by the lack of detectable coronary atherosclerosis in the rest of the coronary bed, the trend towards improvement of symptoms, and the acceptable anterograde flow in the infarct related artery to refrain from performing PTCA and to manage the patients by administering a very aggressive antiplatelet/antithrombotic medical treatment (acetylsalicylic acid, clopidogrel, abciximab, and unfractionated and low molecular weight heparin). The uneventful clinical course, together with the preservation of the ejection fraction, showed that the medical management we adopted was safe, even in the two patients with suboptimal (TIMI 2) flow. In all cases an early angiographic control showed complete resolution of thrombus without significant residual stenosis.
It is reasonable to speculate that the combination of drugs we used facilitated the disappearance of thrombus. In particular the use of glycoprotein IIb/IIIa inhibitors could have exerted a beneficial effect, in agreement with recent data showing that the administration of abciximab reduces the rate of angiographically detectable thrombi in AMI.11
Of the four patients, one was found to have a recognised cause of genetic thrombophilia (G to A 20210 prothrombin gene variant) and one had history of suspected previous venous thrombosis: such data fit with a recent observation suggesting that patients with acute coronary syndromes and limited extent of coronary atherosclerosis at early angiography have a peculiar genetic predisposition to thrombosis.12 Within the wide spectrum of patients presenting with AMI, those younger ones with a prevalent thrombotic component and negligible coronary atherosclerosis may constitute a suitable subset (perhaps with a specific genetic prothrombotic background) who may benefit from an aggressive antithrombotic regimen, without undergoing the risks of a coronary revascularisation procedure.
The present clinical observation calls for further studies to verify the relevance of some clinical and angiographic features in guiding the best clinical management of the different AMI patients.
Acknowledgments
We are indebted to Luigi Conti and the European Imaging Laboratory, Rome, Italy, for skilled help and support in preparing the images showed in the present report. Dr Burzotta is the recipient of a Research Fellowship in Coronary Thrombosis awarded by the European Society of Cardiology.
Abbreviations
AMI, acute myocardial infarction
PTCA, percutaneous transluminal coronary angioplasty
TIMI, thrombolysis in myocardial infarction
REFERENCES
- 1.Davies MJ, Thomas AC. Plaque fissuring: the cause of acute myocardial infarction, sudden ischemic death, and crescendo angina. Br Heart J 1985;53:363–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Falk E. Unstable angina with fatal outcome: dynamic coronary thrombosis leading to infarction and/or sudden death: autopsy evidence of recurrent mural thrombosis with peripheral embolization culminating in total vascular occlusion. Circulation 1985;71:699–708. [DOI] [PubMed] [Google Scholar]
- 3.Antman EM, Giugliano RP, Gibson CM, et al, for the TIMI-14 Investigators. Abciximab facilitates the rate and extent of thrombolysis: results of the thrombolysis in myocardial infarction (TIMI 14) trial. Circulation 1999;99:2720–32. [DOI] [PubMed] [Google Scholar]
- 4.American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Management of Acute Myocardial Infarction). 1999 update: ACC/AHA guidelines for the management of patients with acute myocardial infarction. Circulation 1999;100:1016–30. [DOI] [PubMed] [Google Scholar]
- 5.Sheehan FH, Braunwald E, Canner P, et al. The effect of intravenous thrombolytic therapy on left ventricular function: a report on tissue-type plasminogen activator and streptokinase from the thrombolysis in myocardial infarction (TIMI phase I) trial. Circulation 1987;75:817–29. [DOI] [PubMed] [Google Scholar]
- 6.The TIMI IIIA Investigators. Early effects of tissue-type plasminogen activator added to conventional therapy on the culprit coronary lesion in patients presenting with ischemic cardiac pain at rest. Results of the TIMI IIIA trial. Circulation 1993;87:38–52. [DOI] [PubMed] [Google Scholar]
- 7.Gersh BJ. Current issues in reperfusion therapy. Am J Cardiol 1998;82:3P–11P. [DOI] [PubMed] [Google Scholar]
- 8.Topol EJ, Yadav JS. Recognition of the importance of embolization in atherosclerotic vascular disease. Circulation 2000;101:e570. [DOI] [PubMed] [Google Scholar]
- 9.Steg PG, Himbert D, Benamer H, et al. Conservative management of patients with acute myocardial infarction and spontaneous acute patency of the infarct-related artery. Am Heart J 1997;134:248–52. [DOI] [PubMed] [Google Scholar]
- 10.Grech ED, Sutton AG, Campbell PG, et al. Reappraising the role of immediate intervention following thrombolytic recanalization in acute myocardial infarction. Am J Cardiol 2000;86:400–5. [DOI] [PubMed] [Google Scholar]
- 11.Gibson CM, de Lemos JA, Murphy SA, et al. Combination therapy with abciximab reduces angiographically evident thrombus in acute myocardial infarction. A TIMI 14 substudy. Circulation 2001;103:2550–4. [DOI] [PubMed] [Google Scholar]
- 12.Burzotta F, Paciaroni K, De Stefano V, et al. Increased prevalence of the G20210A prothrombin mutation in acute coronary syndromes with no cardiovascular risk factor or limited extent of disease. Eur Heart J 2002;23:26–30. [DOI] [PubMed] [Google Scholar]