Survivors of myocardial infarction (MI) who are depressed are at increased risk of cardiac death and morbidity than those who are not depressed.1 This adverse effect is independent of the severity of the underlying ischaemic heart disease.1 However, additional care is rarely taken of depressed patients, largely due to a failure in identification. Most studies have used time consuming interviews requiring specially trained staff that may be impractical for day to day use in the clinical setting. The Beck depression inventory (BDI) is a self report inventory which is simple, accurate at identifying depression, and has been used in the USA to indicate those with an adverse prognosis. However, prevalence of depression in the UK may be different to that in the USA when using similar methods post-MI.2,3 Cultural and socioeconomic differences between the USA and UK may exist to uncouple the prognostic association between an elevated BDI score and adverse prognosis. Therefore, the aims of this study were to determine the prevalence of an elevated BDI and to determine the relation between BDI score and prognosis in a UK population following MI.
METHODS
All patients aged less than 75 years consecutively hospitalised with MI to a district general hospital, between 1999 and 2000, were recruited if capable of giving written, informed consent. A specific named nurse provided a copy of the BDI (version II) for completion between the time of discharge from the coronary care unit (usually 48 hours from the time of thrombolysis) and the time of discharge from the hospital (usually 5–7 days from the time of thrombolysis). Information on cultural, social, educational background, together with medical history and details of the current admission, were collated.
Follow up reviews were performed between 2–3 months after discharge and also at six months after discharge. All patients were flagged in the UK National Health Service central register for notification to us of their death and 100% follow up data were obtained.
The cut off chosen as a lower threshold for detecting depression following MI in this study was a BDI score of 12 points based on the findings of the study by Frasure-Smith, which determined that an elevated BDI-I score ⩾ 10 was associated with an odds ratio of 7.82 for 18 month cardiac mortality.1 A score of 10 or more on the BDI-I is equivalent to a score of 12 or more on the BDI-II. To test for differences among patients with and without depression, Fischer’s exact, unpaired t, and Wilcoxon-Mann-Whitney tests were used as appropriate. Survival time distributions were compared using the Peto log rank test.
RESULTS
Of the 131 patients included in the study, 62 patients (47%, 95% confidence interval (CI) 39% to 56%) scored ⩾ 12 at the first in-hospital BDI assessment following MI. The mean (SD) score for those with a BDI of 12 and over at entry was 20 (7), compared to a mean score of 5 (3) for those with a BDI of below 12. There were no differences in size of MI (median creatine kinase concentration 1301 units/l (range 822–2322), location of MI (47 patients (36%) anterior), or rate of thrombolysis (99 patients (76%)) between groups. There was no difference in the rate of in-hospital complications (30 patients (23%)). Those who had an elevated BDI at baseline were more likely to receive calcium antagonists (23 (37%) v 12 (17%), p = 0.02) and less likely to receive a β adrenoceptor antagonist on discharge (20 (32%) v 38 (55%), p = 0.02), but there were no other differences in treatment following MI. No patients were discharged on antidepressant medication.
BDI scores fell in those classified as depressed, with scores at three months declining by 4.6 points (95% CI −6.7 to −2.4, p < 0.01) and at six months by 3.3 points (95% CI −6.0 to −0.5, p = 0.02). In those with a raised BDI at entry, 15 patients scored below the threshold at three months, and at six months nine patients continued to score below 12.
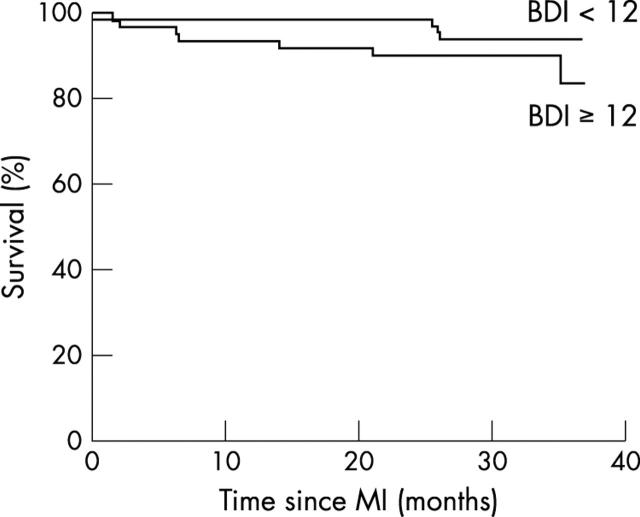
Over a median follow up period of 32 months (range 25–37 months), 7 (11%) depressed patients died compared with 4 (6%) non-depressed patients. The estimated odds ratio (OR) for death in the depressed group compared to the non-depressed group was 1.8, although this difference was not significant (OR 1.8, 95% CI 0.56 to 6.0; p = 0.37). Survival curves are displayed in fig 1. The estimated odds ratio for death in the depressed group on all three visits, compared to those who were not depressed at any time, was 2.3, but this difference was not significant (OR 2.3, 95% CI 0.42 to 15.1, p = 0.42).
Figure 1.
Survival curve for BDI scores above and below 12.
DISCUSSION
Depression post-MI is common in the UK and is detected in 47% of patients using the BDI-II, a rate similar to that found in the USA using structured interviews by trained staff.2,3 This depressive symptomatology is independent of the severity of underlying disease. Prevalence of depression does fall slightly over six months, although a significant number remain affected. A trend towards adverse outcome in depressed patients was found in our study, but this was not significant. In the USA, a BDI-I score greater than 10 measured seven days post-MI was associated with an odds ratio for increased mortality at 18 months of 7.82 (95% CI 2.42 to 25.26).1 Our study has over 90% power at 5% significance to detect such a difference in mortality. The only previous study in the UK using the BDI also failed to find a significant association with mortality at 12 months post-MI.4 This failure to find such a positive association could be due either to a reduction in the applicability of the BDI or to a reduction in the power of the link between depression and prognosis in post-MI patients in the UK. Although our study cannot exclude a smaller effect on prognosis than that previously found in the USA, the recovery of a high proportion of survivors of MI in the UK is blighted by significant psychological debility. The BDI may be used to identify these subjects who may then benefit from the safe, effective treatment for depression that is available.5
Abbreviations
BDI, Beck depression inventory
CI, confidence interval
MI, myocardial infarction
OR, odds ratio
REFERENCES
- 1.Frasure-Smith N, Lesperance F, Talajic M. Depression and 18-month prognosis after myocardial infarction. Circulation 1995;91:999–1005. [DOI] [PubMed] [Google Scholar]
- 2.Schleifer SJ, Macari-Hinson MM, Coyle DA, et al. The nature and course of depression following myocardial infarction. Arch Intern Med 1989;149:1785–9. [PubMed] [Google Scholar]
- 3.Lloyd GG, Cawley RH. Psychiatric morbidity in men one week after first acute myocardial infarction. BMJ 1978;2:1453–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lane D, Carroll D, Ring C, et al. Do depression and anxiety predict recurrent coronary events 12 months after myocardial infarction? QJM 2000;93:739–44. [DOI] [PubMed] [Google Scholar]
- 5.Glassman AH, O’Connor CM, Califf RM, et al. Sertraline treatment of major depression in patients with acute MI or unstable angina. JAMA 2002;288:701–9. [DOI] [PubMed] [Google Scholar]