Abstract
Sudden cardiac arrest associated with major spasm of three coronary arteries was observed about 10 hours after Taxus stent insertion in a three vessel lesion and was successfully treated by intracoronary glyceryl trinitrate infusion. This case illustrates a potential risk associated with drug eluting stent and alerts clinicians to the life threatening risk of spasm when stenting multiple vessels with drug eluting stent (especially the Taxus stent).
Keywords: Taxus stent, spasm, stenting
A 62 year old woman was referred for acute chest pain. ECG and an echocardiogram showed acute inferior myocardial infarction. Coronary angiography showed a total occlusion of the proximal right coronary artery and significant focal stenosis in the mid left anterior descending artery and the proximal left circumflex artery (fig 1). Taxus stents (slow release, polymer based, paclitaxel eluting Express stent, Boston Scientific, Natick, Massachusetts, USA) measuring 3.5 × 28 mm, 3.0 × 24 mm, and 3.5 × 16 mm were successfully implanted in the right coronary artery, left anterior descending artery, and left circumflex artery lesions, respectively, after mandatory predilatation. The patient had been treated with calcium channel antagonist and oral nitrate. Ten hours after the procedure, sudden cardiac arrest developed and advanced cardiac life support was performed. Emergency repeated coronary angiography showed severe diffuse narrowing of three coronary arteries except for the previously implanted stent sites (fig 2). Severe diffuse spasms were documented and promptly relieved by intracoronary glyceryl trinitrate injection. The patient was successfully resuscitated and recovered.
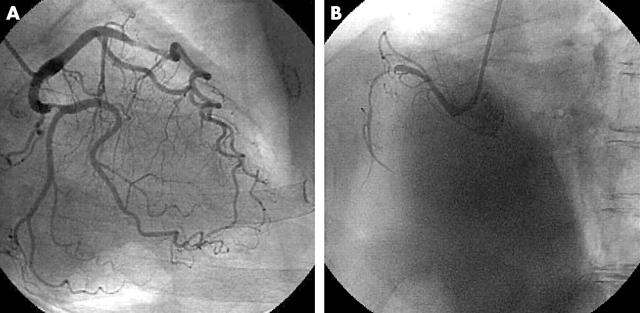
Figure 1.
Coronary angiography showed total occlusion of the proximal right coronary artery and significant focal stenosis in the mid left anterior descending artery and the proximal left circumflex artery.
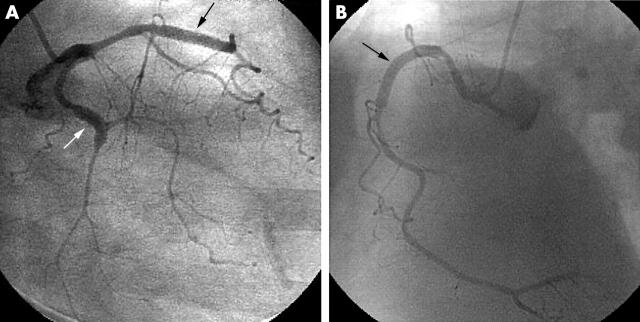
Figure 2.
About 10 hours after stenting, emergency coronary angiography showed severe diffuse narrowing of three coronary arteries except at the sites of the previously implanted stents (arrows).
DISCUSSION
To our knowledge, this is the first report of a multivessel spasm induced by Taxus stent insertion. Coronary artery spasm is reported to occur in 15% of percutaneous coronary interventions. However, the incidence of spasm associated coronary stenting is not clear. Rodgers and colleagues1 reported that in a swine model in which a stent was inserted into the coronary artery, spasm was likely to occur proximal to and distal to the stent, particularly at sites of arteriosclerosis. The exact mechanism of spasm induced by stenting is not known. However, Egashira and colleagues2 observed that ergonovine induced excessive coronary contraction in dogs four weeks after detachment of the intima but not immediately after the insult, and they speculated that excessive contraction occurs after the injured intima has been relined by endothelial cells. In the present case, spasm occurred about 10 hours after stenting. Endothelial injury caused by the end of the stent during its insertion may be a significant cause of spasm. However, in this case, the stent was very easily delivered to the target site without any resistance after adequate predilatation. It is not known whether drug eluting stents including Taxus cause spasm more easily than bare metal stents. However, this may be a potential risk associated with drug eluting stents. Considering the increasing incidence of multivessel stenting with drug eluting stents, the possibility of life threatening coronary spasm caused by stent deployment has to be taken into account during coronary interventions.
REFERENCES
- 1.Rodgers G, Raizner A, Cromeens D, et al. Coronary spasm induced by stent implantation. J Am Coll Cardiol 1989;13:194A. [Google Scholar]
- 2.Egashira K, Tomoike H, Hayashi Y, et al. Mechanism of ergonovine-induced hypercontraction of the large epicardial coronary artery in conscious dogs a month after arterial injury. Circ Res 1992;71:435–42. [DOI] [PubMed] [Google Scholar]