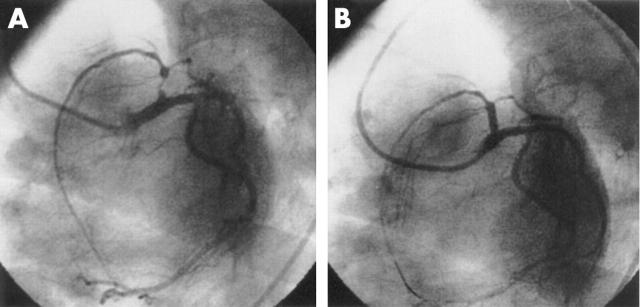
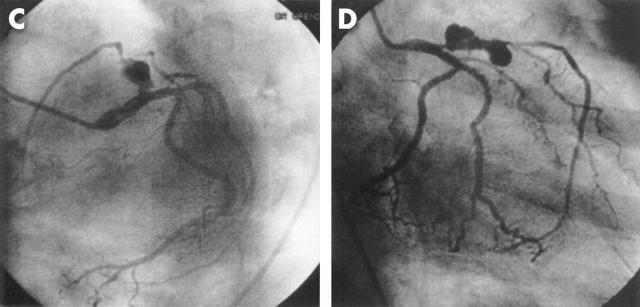
A 75 year old woman underwent an uneventful coronary angioplasty with stenting of the proximal left anterior descending (LAD) artery for acute coronary syndrome in August 2003. A 3.0 × 13 mm sirolimus eluting Cypher stent (Cordis Europa, NV) was used with good result (panels A and B). The patient started complaining of dyspnoea with angina (New York Heart Association functional class II) four months after the procedure. The symptoms became NYHA class III at the time of presentation six months after the initial procedure. A repeat angiography was performed which showed large aneurysms at both the proximal and distal ends of the stent, with evidence of significant stenosis at the inflow of proximal and outflow of distal aneurysm (panels C and D).
The patient underwent surgery. The operative findings showed pronounced inflammation and fibrosis around the area of proximal LAD with plastering of tissues, which were very hard in consistency. No dissection of this area was done and the distal LAD was grafted using a left internal mammary artery. The patient is doing well and symptom-free after three months of follow up.