The definition of sudden cardiac death (SCD) remains controversial. Many such deaths are not witnessed, and without cardiac monitoring at the time of death the assumption of an underlying arrhythmic cause is speculative. Nevertheless, it has been estimated that SCD accounts for 300 000 to 400 000 deaths annually in the USA.1 The degeneration of monomorphic ventricular tachycardia (VT) into ventricular fibrillation (VF) accounts for the majority of sudden arrhythmic deaths.w1
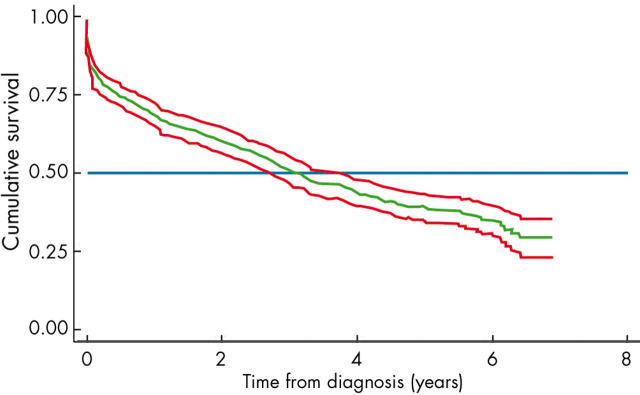
Despite considerable advances in the treatment of heart failure over the past 20 years, morbidity and mortality remain high with a four year survival of less than 50% in population based studies (fig 1). Ventricular arrhythmias (including non-sustained VT) have been documented in up to 85% of patients with severe congestive heart failure.2
Figure 1.
Cumulative survival of 552 incident (new) cases of heart failure identified in the London heart failure studies 1995 to 1998. Kaplan-Meier estimates with 95% point wise confidence bands (authors’ own data).
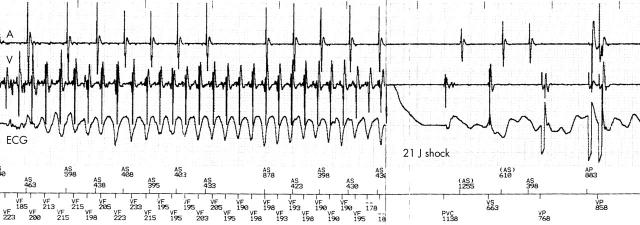
The implantable cardioverter-defibrillator (ICD) is highly effective at terminating life threatening ventricular tachyarrhythmia (fig 2). In selected high risk patients ICDs have proven to be a cost effective method of reducing mortality. At present, 1–2% of the population has heart failure and numbers continue to increase,3 but the ICD remains expensive. The challenge lies in identifying patients with heart failure who are at significant risk of arrhythmia and who would benefit from an ICD in addition to other antiarrhythmic strategies.
Figure 2.
Implantable cardioverter-defibrillator (ICD) data showing an episode of ventricular fibrillation terminated by a 21 J shock delivered by the device. Intracardiac electrograms are recorded from the right atrium (A) and right ventricle (V) along with a surface ECG. Sensed intracardiac intervals are shown at the bottom of the figure. Following cardioversion, ventricular fibrillation is terminated and bradycardia is seen requiring atrioventricular pacing.
RISK STRATIFICATION OF SCD
Heart failure aetiology
Patients with heart failure caused by ischaemic heart disease are generally considered to be at high risk of SCD, and have been the focus of many large randomised controlled trials of primary and secondary prevention of SCD. In the second multicenter automatic defibrillator implantation trial (MADIT II)4 of patients with low left ventricular ejection fraction (LVEF) and previous myocardial infarction, the all cause mortality was around 10% per year. In the eplerenone post-acute myocardial infarction heart failure efficacy and survival study (EPHESUS) of patients with symptomatic heart failure and LVEF < 40%, the one year mortality in the placebo arm was 13.6%, despite optimal medical therapy. The 12 month SCD rate was almost 5% increasing to nearly 8% at two years.5
The annual mortality in dilated cardiomyopathy (DCM) has been reported to range from 10–50% from referral centres, with up to 28% of deaths being classified as sudden.6w2 More recent studies of DCM patients on optimal medical treatment have reported considerably lower mortality rates of around 7% at two years.7 Although patients with DCM were excluded from many early ICD studies, a number of recent randomised trials have included such patients and will provide crucial outcome data to guide patient management.8,9
The recently reported sudden cardiac death in heart failure trial (SCD-HeFT) demonstrated similar relative risk reductions in mortality in ischaemic and non-ischaemic patients (21% and 27%, respectively) suggesting that the use of ICDs in patients with severely depressed left ventricular (LV) function was beneficial regardless of the aetiology of heart failure.9 The results were less conclusive in the cardiomyopathy trial (CAT) of patients with DCM: the study was terminated early with no reduction in all cause mortality at two and four years follow up, although the study was underpowered.7
New York Heart Association class
Mortality rates increase the higher the New York Heart Association (NYHA) class, but the proportion of patients dying suddenly (rather than from progressive pump failure) is highest among those with less severe heart failure (NYHA class II or III) (fig 3).10 Many of the randomised controlled trials have excluded patients in NYHA class IV, making decisions for use of therapeutic strategies for SCD more difficult in those patients with the worst prognosis.
Figure 3.
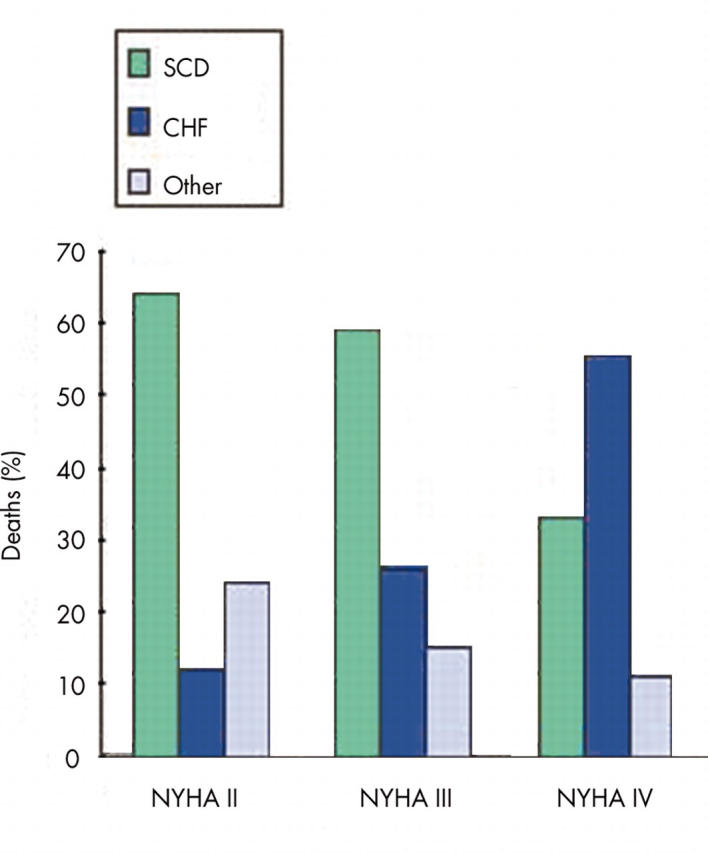
Severity of heart failure and the mode of death in the MERIT-HF study. CHF, congestive heart failure; MERIT-HF, metoprolol CR/XL randomized intervention trial in heart failure; NYHA, New York Heart Association; SCD, sudden cardiac death. Adapted from MERIT-HF Study Group. Lancet 1999;353:2001–7.
Syncope
Syncope is an important risk factor for SCD in patients with advanced heart failure, regardless of the underlying aetiology.w3 Observational data suggest that around 30% of patients with DCM, NYHA class III or IV symptoms, and recurrent syncope, will receive an appropriate shock for ventricular arrhythmia by one year after implantation of an ICD, rising to around 50% by two years.w4 w5
Left ventricular systolic dysfunction
Patients with severe LV systolic dysfunction are among those at greatest risk for SCD. However, it remains uncertain whether the degree of LV impairment per se can be used to estimate the risk of SCD. During four years of follow up after implantation of an ICD in patients with documented ventricular arrhythmia, both the proportion of patients who had received an ICD therapy and the sudden death rates were comparable between patients with moderate or severe LV dysfunction (LVEF > 30% and < 30%, respectively).w6
QRS duration
In patients with documented ventricular arrhythmias and moderately severe heart failure caused by poor LV systolic function, a long QRS duration was associated with a higher risk of death from a cardiac cause.w7 Intraventricular conduction delay is used in the heart failure survival score for estimating prognosis in patients with severe heart failure.w8 The QRS duration has not been used as an inclusion criterion in randomised controlled ICD trials, although there is some evidence from post hoc subgroup analysis that the benefit of ICD therapy may be greater in those with broader QRS complexes.
QT dispersion
The dispersion of the QT interval on the surface ECG is increased in patients with heart failure. This was initially considered to be associated with an increased risk of ventricular arrhythmias and SCD,w9 but this finding has proved inconsistent.w10
Holter monitoring
Before hospital discharge after acute myocardial infarction, around 9% of patients will have non-sustained VT on Holter monitoring. Only a minority of such patients also have a low LVEF. The presence of non-sustained VT has a very low positive predictive value for subsequent arrhythmic events or mortality in this clinical setting.w11
In patients with chronic heart failure, however, the presence of non-sustained VT has been shown to identify a population at high risk of SCD.w12 Patients with DCM (LVEF ⩽ 30%) and a history of non-sustained VT have an incidence of appropriate ICD interventions similar to that of DCM patients with a history of syncope or sustained VT/VF, at around 37% over three years.11
In the defibrillator in non-ischaemic cardiomyopathy treatment evaluation (DEFINITE) trial, in patients with DCM (LVEF < 36%) on optimal medical treatment with premature ventricular complexes or non-sustained VT, the ICD significantly reduced the risk of the primary end point of SCD by 80% (95% confidence interval (CI) 29% to 94%), with a non-significant reduction in the risk of death from any cause.12
Signal averaged ECG
The signal averaged ECG (SAECG) is a highly amplified, processed ECG that detects microvolt electrical potentials (late potentials) in the terminal QRS complexw13 originating from abnormal scarred myocardium with regions of slow conduction. The presence of late potentials on SAECG has been shown to identify patients at high arrhythmic risk after myocardial infarction.w14
In the multicenter unsustained tachycardia trial (MUSTT), an abnormal SAECG combined with an LVEF < 30% in patients with coronary artery disease was found to predict those patients at highest risk of arrhythmic and cardiac death.13
In contrast, no mortality difference was demonstrated between those with LV systolic dysfunction and an abnormal SAECG randomised to either ICD or to the control group at the time of coronary artery bypass surgery in the coronary artery bypass graft (CABG) Patch trial.14
There is no evidence that SAECG is of value in risk stratification of patients with DCM, as this has been found to have both a low sensitivity and specificity for serious arrhythmic events.w15
As a screening test the SAECG has a number of limitations. Late potentials from the anteroseptal walls may be masked within the main QRS because these areas are activated earliest. Similarly, late potentials may not outlast an abnormally wide QRS, and may not be detected even in patients with inducible VT.w16
Heart rate variability and baroreflex sensitivity
Abnormalities of the autonomic nervous system have been implicated in the genesis of SCD in patients with heart failure after myocardial infarction. Specific autonomic parameters (such as heart rate variability) reflect neurohormonal interaction with the sinus node and are decreased by the raised sympathetic activity observed in heart failure. In the multicentre postinfarction study a strong correlation was found between reduced heart rate variability and all cause mortality after acute myocardial infarction, with greatest prognostic value in those patients with an LVEF < 30%.15 However, the changes observed acutely were transient and almost completely vanished within 6–12 weeks. The value of this test is, of course, significantly limited in patients with atrial fibrillation or frequent premature atrial or ventricular complexes.
T wave alternans
Beat-to-beat variation in T wave amplitude known as microvolt T wave alternans (TWA) may be a useful tool for risk stratifying SCD in heart failure, regardless of the aetiology of heart failure, but has yet to be fully evaluated. Early reports suggest a very high negative predictive value, combined with an arrhythmic event rate (SCD, cardiac arrest, or sustained VT) of around 15–20% over 1–2 years follow up in those with positive or indeterminate TWA.16w17 w18
Electrophysiologic testing
Two randomised trials of primary prevention of SCD, the first multicenter automatic defibrillator implantation trial (MADIT) and MUSTT, required sustained ventricular tachyarrhythmia to be inducible at formal electrophysiological (EP) testing in patients with coronary artery disease, asymptomatic non-sustained VT, and impaired LV systolic function, before randomisation to prophylactic ICD or conventional antiarrhythmic drug treatment. Both demonstrated a > 50% relative risk reduction in all cause mortality.17,18
However, the lack of inducible sustained ventricular tachyarrhythmia at EP testing in the MUSTT study did not exclude the risk of cardiac arrest or arrhythmic death even within two years (negative predictive value was only 88%). In such patients, the absolute risk of SCD remains high (12% at two years, 24% at five years) with an overall mortality rate of 44% at five years with 45% of deaths reported to result from arrhythmia.19
EP testing may fail to provoke tachycardia altogether in DCMw15 and should not be relied upon to exclude the risk of SCD.
The induction of sustained monomorphic VT at EP testing therefore provides clear identification of patients at high risk of SCD for whom primary prevention with an ICD is advised. Failure to induce VT does not equate to no risk and thus poses important clinical management problems.
B-type natriuretic peptide
B-type natriuretic peptide (BNP) is secreted primarily from the left ventricle in response to changes in myocardial wall stretch. The plasma concentration of this peptide is strongly correlated with the degree of LV dysfunction and the risk of death.w19 In a study of 452 patients with ischaemic or non-ischaemic cardiomyopathy and LVEF < 35%, a plasma BNP cut off point of 130 pg/ml gave a 99% negative predictive value for SCD, with a positive predictive value of only 19% over an average 18 month follow up.20 This requires prospective validation.
PREVENTION OF SCD
Pharmacotherapy
Angiotensin converting enzyme inhibitors
Angiotensin converting enzyme (ACE) inhibitors reduce total mortality in patients with systolic heart failure recruited to randomised placebo controlled trials, and are considered first line agents. The mortality benefit is seen in all NYHA classes, but was seen with greatest absolute benefit among those with the most severely impaired LV function. ACE inhibitors have been shown to decrease death from progressive heart failure, but a recent meta-analysis did not report a consistent effect on arrhythmic mortality.21
Aldosterone receptor antagonists
A 30% reduction in mortality was achieved by the use of spironolactone in addition to an ACE inhibitor and diuretic in patients with moderate to severe heart failure caused by LV systolic dysfunction (NYHA class III or IV).22 This mortality benefit was attributed to a lower risk of death caused by both progressive heart failure and SCD. The postulated mechanisms for reducing SCD included increased serum potassium, increased myocardial uptake of noradrenaline (norepinephrine), and decreased myocardial fibrosis. In the recently reported EPHESUS trial of heart failure or LV systolic dysfunction after acute myocardial infarction, the aldosterone receptor antagonist eplerenone significantly reduced overall mortality by 15%, and SCD by 21%.5 In the subgroup of patients with an LVEF < 30%, eplerenone reduced SCD by 33%.w20
β Blockers
β Blockers have been shown to reduce morbidity and mortality in patients with chronic heart failure in randomised controlled trials, and consistently reduce the risk of SCD by between 40–55%.10,23 The use of carvedilol (in addition to ACE inhibitors) in the carvedilol post-infarct survival control in LV dysfunction (CAPRICORN) study of patients after myocardial infarction with LVEF < 40%, produced a significant reduction in total mortality, and a trend toward fewer SCD.w21
Antiarrhythmic agents
Clinical trials using class I antiarrhythmic drugs to suppress ventricular arrhythmia in patients after acute myocardial infarction were terminated prematurely because of an excess mortality attributed to drug induced pro-arrhythmia.w22
Two large randomised studies have specifically assessed amiodarone treatment as a primary prevention strategy for SCD in heart failure, with variable results. The GESICA (grupo de estudio de la sobrevida en la insuficiencia cardiaca en Argentina) trial reported a 28% risk reduction in mortality among NYHA III–IV patients randomised to treatment with amiodarone, compared with placebo. However, reductions in SCD were not significant.24 In contrast, the survival trial of antiarrhythmic therapy for congestive heart failure (CHF-STAT) (LVEF ⩽ 40% and > 10 ventricular ectopics per hour) found no reduction in SCD or mortality benefit from treatment with amiodarone, although there was a strong trend to mortality benefit in those with a non-ischaemic aetiology.25 Similarly, the recently completed SCD-HeFT study reported no survival benefit from the use of amiodarone in patients with either ischaemic or non-ischaemic cardiomyopathy in comparison with placebo.9
Sudden cardiac death in heart failure: key points.
Sudden cardiac death (SCD) is a major cause of death in the growing population of patients with heart failure
Ventricular arrhythmias have been documented in up to 85% of patients with severe congestive heart failure
Patients with severe left ventricular (LV) systolic dysfunction are among those at greatest risk for SCD
To date, no single test reliably predicts arrhythmic risk in patients with heart failure
Optimal medical treatment will improve prognosis and reduce the risk of SCD in heart failure patients
The implantable cardioverter-defibrillator (ICD) effectively treats malignant ventricular arrhythmias and is indicated for the secondary prevention of SCD
There is growing evidence for the use of the ICD for the primary prevention of SCD
Even among patients presenting with symptomatic ventricular arrhythmias, the efficacy of antiarrhythmic drug treatment is disappointing. At best, half of patients treated for VT are rendered non-inducible at EP study, and there is a high recurrence rate of clinical arrhythmia.w23 A careful risk–benefit evaluation is recommended before prescribing antiarrhythmic drugs for patients with significant LV systolic dysfunction.
Device therapy
Implantable cardioverter-defibrillator
A number of trials have established the efficacy of ICDs in reducing mortality by 20–60% (compared with antiarrhythmic drug treatment) over a 2–5 year follow up period in patients with poor LV function and documented (or inducible) ventricular arrhythmia.17,18 Trials have also been conducted in the primary prevention of SCD using the ICD in patients with LV systolic dysfunction without documented arrhythmia. All cause mortality was reduced by 31% over two years (p = 0.016) in the MADIT II study of patients with low LVEF and previous myocardial infarction, and 23% over five years (p = 0.007) in the SCD-HeFT study of patients with low LVEF, NYHA class II or III, and either ischaemic or non-ischaemic cardiomyopathy (table 1).4,9 The mortality in the optimal medical treatment arms of both of these trials was around 7–10% per year.
Table 1.
Randomised trials of ICDs for primary and secondary prevention of SCD in patients with heart failure
| Name of trial | Heart failure aetiology and severity | Number of patients | Additional risk stratification tool | Treatment groups | Primary and *secondary outcomes | Result |
| AVID29 | Mean LVEF 32% | 1016 | Resuscitated VF or VT | 1. Class III antiarrhythmic drugs | 1. Total mortality | 1.39% relative risk reduction |
| 2. ICD | *2. QOL | |||||
| *3. Cost | ||||||
| CIDS30 | Mean LVEF 34% | 659 | Resuscitated VF or VT or unmonitored syncope | 1. Amiodarone | 1. Total mortality | 1.20% relative risk reduction (NS) |
| 2. ICD | *2. Arrhythmic death | 2.33% relative risk reduction (NS) | ||||
| MADIT17 | Previous MI, NYHA I–III, LVEF <35% | 196 | Asymptomatic NSVT with inducible sustained VT at EPS | 1. Medical treatment | 1. Total mortality | 1.54% relative risk reduction |
| 2. ICD | ||||||
| MUSTT18 | IHD, LVEF <40% | 704 | Asymptomatic NSVT with inducible sustained VT at EPS | 1. Antiarrhythmics and ICD | 1. Cardiac arrest or death from arrhythmia | 1.27% relative risk reduction |
| 2. No antiarrhythmic treatment | *2. Total mortality | 2.20% relative risk reduction | ||||
| *3. Sustained VT | 3. NS | |||||
| CABG-Patch14 | CABG surgery, LVEF <36% | 900 | Abnormal SAECG | 1. ICD | 1. Total mortality | 1. NS |
| 2. Control | ||||||
| MADIT II4 | Prior MI, LVEF <30% | 1232 | None | 1. Medical treatment | 1. Total mortality | 1. 31% relative risk reduction |
| 2. ICD | ||||||
| SCD-HeFT9 | IHD or DCM, NYHA II–III, LVEF <35% | >2500 | None | 1. Amiodarone | 1. Total mortality | 1. Amiodarone v placebo: No reduction. ICD v placebo: 23% relative risk reduction |
| 2. Placebo | ||||||
| 3. ICD | ||||||
| AMIOVIRT31 | DCM, NYHA I–III, LVEF <35% | 103 | Asymptomatic NSVT | 1. Amiodarone | 1. Total mortality | 1. NS |
| 2. ICD | *2. Arrhythmia-free survival | 2. NS | ||||
| *3. QOL | 3. NS | |||||
| *4. Cost | 4. NS | |||||
| CAT7 | DCM <9 months, NYHA II–III, LVEF <30% | 104 | None | 1. Control | 1. Total mortality | 1. NS |
| 2. ICD | ||||||
| DEFINITE12 | DCM, LVEF <36% | 458 | PVCs or NSVT | 1. Medical treatment | 1. Total mortality | 1. 35% relative risk reduction (NS) |
| 2. Medical treatment + ICD | 2. Arrhythmic death | 2. 80% relative risk reduction | ||||
| COMPANION8 | IHD or DCM, NYHA III–IV, LVEF <35% | 1520 | None | 1. Control 2. CRT | 1. Death from or hospitalisation for any cause | CRT ICD v control 1. 19% relative risk reduction |
| 3. CRT with ICD | *2. Death or hospitalisation from heart failure | 2. 40% relative risk reduction | ||||
| *3. Total mortality | 3. 36% relative risk reduction |
CABG, coronary artery bypass graft; CRT, cardiac resynchronisation therapy; DCM, idiopathic dilated cardiomyopathy; EPS, electrophysiological study; ICD, implantable cardioverter-defibrillator; IHD, ischaemic heart disease; LVEF, left ventricular ejection fraction; MI, myocardial infarction; NS, non-significant; NSVT, non-sustained ventricular tachycardia; NYHA, New York Heart Association; PVC, premature ventricular complex; QOL, quality of life; SAECG, signal averaged ECG; VF, ventricular fibrillation; VT, ventricular tachycardia.
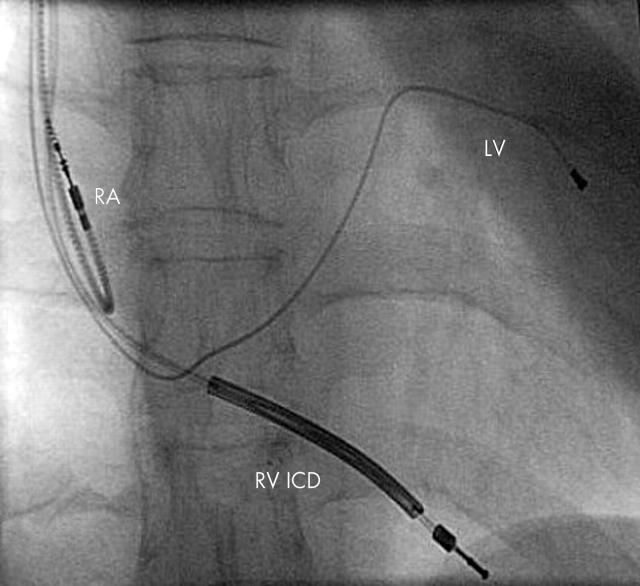
Biventricular pacing
In patients with advanced LV systolic dysfunction, concomitant conduction tissue disease may contribute to worsening heart failure because of loss of ventricular synchrony. Right ventricular pacing may induce ventricular dyssynchrony iatrogenically and worsen heart failure.4,26 Biventricular pacing attempts to resynchronise the failing heart providing functional and symptomatic improvements,27 and is increasingly used in combination with an ICD (fig 4). Preliminary data from the comparison of medical therapy, pacing and defibrillation in heart failure (COMPANION) study found biventricular pacing to reduce all cause mortality by 24% (p = 0.06) compared to optimal medical treatment at 12 months, the benefit increasing to 36% (p = 0.003) with a combined biventricular pacemaker-defibrillator.8 It seems likely that the use of combined devices will continue to expand with significant cost implications.
Figure 4.
Fluoroscopy showing lead positions of an atrio-biventricular ICD in an anteroposterior projection. LV, left ventricular coronary sinus lead; RA, right atrial lead; RV ICD, right ventricular implantable cardioverter-defibrillator lead.
Guidelines
Following the publication of MADIT II and CAT, the European Society of Cardiology guidelines on primary prevention of SCD were updated.28 Secondary prevention of SCD with an ICD remained the strongest possible recommended (class I) indication for patients with LV systolic dysfunction and heart failure—whether ischaemic or non-ischaemic.
In patients with heart failure after acute myocardial infarction, β blockers, ACE inhibitors, and aldosterone receptor blockers were recommended with class I indication. Amiodarone and the implantation of an ICD in patients with an LVEF < 30% were both given a class IIa indication (“some controversy but weight of evidence in favour”). Although the use of the ICD in primary prevention has been shown to reduce mortality,4 it was agreed that concordant results from other studies would be required before a class I recommendation could be given.28
For DCM, ACE inhibitors and β blockers were given class I indications for both primary and secondary prevention of SCD, and aldosterone receptor antagonists class IIa indication. Patients with symptomatic DCM (NYHA class II–III), LVEF < 30%, without documented symptomatic ventricular tachyarrhythmia (as in the CAT study) do not have a very poor short term prognosis with consequent downgrading of the indication for an ICD from class IIa to IIb (“efficacy less well established”).28
Since this update several trials of SCD prevention have been published. A joint American Heart Association/American College of Cardiology/European Society of Cardiology guideline is due to be published shortly.
CONCLUSION
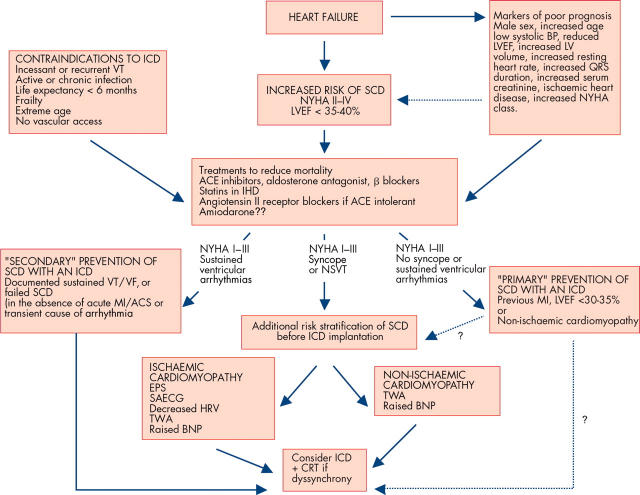
The number of patients with heart failure at risk of SCD is increasing. No single test reliably predicts arrhythmic risk in patients with heart failure—a combination of tests improves risk stratification and helps identify patients at greatest risk of SCD. A possible approach is outlined in fig 5. Further work is necessary to determine the simplest and best method of risk stratification.
Figure 5.
Algorithm for the assessment and management of patients with heart failure at risk of sudden cardiac death. ACE, angiotensin converting enzyme; ACS, acute coronary syndrome; BNP, B type natriuretic peptide; BP, blood pressure; CRT, cardiac resynchronisation therapy; EPS, electrophysiological study; HRV, heart rate variability; ICD, implantable cardioverter-defibrillator; LV, left ventricular; LVEF, left ventricular ejection fraction; MI, myocardial infarction; NSVT, non-sustained ventricular tachycardia; NYHA, New York Heart Association; SAECG, signal averaged ECG; SCD, sudden cardiac death; TWA, T wave alternans; VF, ventricular fibrillation; VT, ventricular tachycardia.
All heart failure patients should have their medical treatment optimised—the use of ACE inhibitors, β blockers, and aldosterone blockers are likely to improve prognosis, and reduce the risk of SCD. The ICD offers an effective therapy for treating malignant ventricular arrhythmia and is indicated for the secondary prevention of SCD. Primary prevention strategies are being refined, and the result of recent clinical trials along with discussions regarding the cost effectiveness of different strategies will consolidate the professional consensus in the coming years. More, rather than less, implants are likely to be needed.
Additional references appear on the Heart website—http://www.heartjnl.com/supplemental
Supplementary Material
Take the online multiple choice questions associated with this article (see page 695)
Competing interests: Dr R Lane received a research fellowship from Medtronic Inc. Professor M Cowie has a consultancy agreement with Medtronic Inc. Dr A Chow has no conflict of interest.
REFERENCES
- 1.Engelstein ED, Zipes DP. Sudden cardiac death. In: Alexander RW, Schlant RC, Fuster V, eds. The heart, arteries and veins. New York: McGraw-Hill, 1998:1081–112.
- 2.Singh SN, Carson PE, Fisher SG. Nonsustained ventricular tachycardia in severe heart failure. Circulation 1997;96:3794–5. [PubMed] [Google Scholar]
- 3.Cowie MR, Mosterd A, Wood DA, et al. The epidemiology of heart failure. Eur Heart J 1997;18:208–25. [DOI] [PubMed] [Google Scholar]
- 4.Moss AJ, Zareba W, Hall WJ, et al. Prophylactic implantation of a defibrillator in patients with myocardial infarction and reduced ejection fraction. N Engl J Med 2002;346:877–83. ▸ MADIT II was a randomised controlled trial of implantable defibrillator versus medical treatment. Prophylactic implantation of a defibrillator in patients with reduced left ventricular ejection fraction and prior myocardial infarction significantly reduced mortality. [DOI] [PubMed] [Google Scholar]
- 5.Pitt B, Remme W, Zannad F, et al. Eplerenone, a selective aldosterone blocker, in patients with left ventricular dysfunction after myocardial infarction. N Engl J Med 2003;348:1309–21. ▸ Aldosterone blockade with eplerenone reduces morbidity and mortality among patients with acute myocardial infarction and left ventricular dysfunction with a 21% reduction in sudden cardiac death. [DOI] [PubMed] [Google Scholar]
- 6.Zipes DP, Wellens HJ. Sudden cardiac death. Circulation 1998;98:2334–51. ▸ An excellent review of the pathogenesis, prevention, and treatment of sudden cardiac death. [DOI] [PubMed] [Google Scholar]
- 7.Bansch D, Antz M, Boczor S, et al. Primary prevention of sudden cardiac death in idiopathic dilated cardiomyopathy: the cardiomyopathy trial (CAT). Circulation 2002;105:1453–8. ▸ This randomised controlled trial failed to demonstrate a reduction in mortality with prophylactic ICD implantation in patients with DCM and impaired ejection fraction. [DOI] [PubMed] [Google Scholar]
- 8.Bristow MR, Saxon LA, Boehmer J, et al. Cardiac-resynchronization therapy with or without an implantable defibrillator in advanced chronic heart failure. N Engl J Med 2004;350:2140–50. ▸ Multicentre randomised controlled trial of > 1500 patients randomised to receive optimal pharmacologic treatment alone or in combination with cardiac resynchronisation therapy with either a pacemaker or pacemaker–defibrillator. CRT with an ICD significantly reduced mortality. [DOI] [PubMed] [Google Scholar]
- 9.Bardy GH, Lee KL, Mark DB, et al. Amiodarone or an implantable defibrillator for congestive heart failure. N Engl J Med 2005;352:225–37. [DOI] [PubMed] [Google Scholar]
- 10.MERIT-HF Investigators. Effect of metoprolol CR/XL in chronic heart failure: Metoprolol CR/XL randomised intervention trial in congestive heart failure (MERIT-HF). Lancet 1999;353:2001–7. [PubMed] [Google Scholar]
- 11.Grimm W, Hoffmann JJ, Muller HH, et al. Implantable defibrillator event rates in patients with idiopathic dilated cardiomyopathy, nonsustained ventricular tachycardia on Holter and a left ventricular ejection fraction below 30%. J Am Coll Cardiol 2002;39:780–7. [DOI] [PubMed] [Google Scholar]
- 12.Kadish A, Dyer A, Daubert JP, et al. Prophylactic defibrillator implantation in patients with nonischemic dilated cardiomyopathy. N Engl J Med 2004;350:2151–8. ▸ This randomised controlled trial found the implantation of a defibrillator significantly reduced the risk of sudden death from arrhythmia in patients with severe, non-ischemic dilated cardiomyopathy treated with ACE inhibitors and β blockers. [DOI] [PubMed] [Google Scholar]
- 13.Gomes JA, Cain ME, Buxton AE, et al. Prediction of long-term outcomes by signal-averaged electrocardiography in patients with unsustained ventricular tachycardia, coronary artery disease, and left ventricular dysfunction. Circulation 2001;104:436–41. ▸ In this study an abnormal SAECG predicted arrhythmic death or cardiac arrest in 36% of patients with coronary artery disease, unsustained VT, and LV dysfunction. [DOI] [PubMed] [Google Scholar]
- 14.Bigger JT Jr. Prophylactic use of implanted cardiac defibrillators in patients at high risk for ventricular arrhythmias after coronary-artery bypass graft surgery. Coronary artery bypass graft (CABG) Patch trial investigators. N Engl J Med 1997;337:1569–75. [DOI] [PubMed] [Google Scholar]
- 15.La Rovere MT, Pinna GD, Maestri R, et al. Short-term heart rate variability strongly predicts sudden cardiac death in chronic heart failure patients. Circulation 2003;107:565–70. [DOI] [PubMed] [Google Scholar]
- 16.Klingenheben T, Zabel M, D’Agostino RB, et al. Predictive value of T-wave alternans for arrhythmic events in patients with congestive heart failure. Lancet 2000;356:651–2. [DOI] [PubMed] [Google Scholar]
- 17.Moss AJ, Hall WJ, Cannom DS, et al. Improved survival with an implanted defibrillator in patients with coronary disease at high risk for ventricular arrhythmia. Multicenter automatic defibrillator implantation trial investigators. N Engl J Med 1996;335:1933–40. [DOI] [PubMed] [Google Scholar]
- 18.Buxton AE, Lee KL, Fisher JD, et al. A randomized study of the prevention of sudden death in patients with coronary artery disease. Multicenter unsustained tachycardia trial investigators. N Engl J Med 1999;341:1882–90. [DOI] [PubMed] [Google Scholar]
- 19.Buxton AE, Lee KL, DiCarlo L, et al. Electrophysiologic testing to identify patients with coronary artery disease who are at risk for sudden death. Multicenter unsustained tachycardia trial investigators. N Engl J Med 2000;342:1937–45. ▸ This large multicentre trial showed a negative electrophysiologic study in patients with coronary artery disease, left ventricular dysfunction and non-sustained ventricular tachycardia was associated with a significantly lower risk of sudden death. [DOI] [PubMed] [Google Scholar]
- 20.Berger R, Huelsman M, Strecker K, et al. B-type natriuretic peptide predicts sudden death in patients with chronic heart failure. Circulation 2002;105:2392–7. [DOI] [PubMed] [Google Scholar]
- 21.Naccarella F, Naccarelli GV, Maranga SS, et al. Do ACE inhibitors or angiotensin II antagonists reduce total mortality and arrhythmic mortality? A critical review of controlled clinical trials. Curr Opin Cardiol 2002;17:6–18. [DOI] [PubMed] [Google Scholar]
- 22.Pitt B, Zannad F, Remme WJ, et al. The effect of spironolactone on morbidity and mortality in patients with severe heart failure. Randomized aldactone evaluation study investigators. N Engl J Med 1999;341:709–17. [DOI] [PubMed] [Google Scholar]
- 23.CIBIS-II Investigators. The cardiac insufficiency bisoprolol study II (CIBIS-II): a randomised trial. Lancet 1999;353:9–13. ▸ In this multicentre trial of > 2600 patients with symptomatic heart failure in NYHA III or IV, the addition of bisoprolol to standard optimal medical treatment significantly reduced all cause mortality and sudden cardiac death. [PubMed] [Google Scholar]
- 24.Doval HC, Nul DR, Grancelli HO, et al. Randomised trial of low-dose amiodarone in severe congestive heart failure. Grupo de estudio de la sobrevida en la insuficiencia cardiaca en Argentina (GESICA). Lancet 1994;344:493–8. ▸ This randomised controlled trial demonstrated a reduction in all cause mortality in patients with heart failure treated with amiodarone. [DOI] [PubMed] [Google Scholar]
- 25.Singh SN, Fletcher RD, Fisher SG, et al. Amiodarone in patients with congestive heart failure and asymptomatic ventricular arrhythmia. Survival trial of antiarrhythmic therapy in congestive heart failure. N Engl J Med 1995;333:77–82. ▸ This study found amiodarone failed to reduce the incidence of sudden death or prolong survival among patients with heart failure and LV ejection fraction < 40%. [DOI] [PubMed] [Google Scholar]
- 26.Wilkoff BL, Cook JR, Epstein AE, et al. Dual-chamber pacing or ventricular backup pacing in patients with an implantable defibrillator: the dual chamber and VVI implantable defibrillator (DAVID) trial. JAMA 2002;288:3115–23. [DOI] [PubMed] [Google Scholar]
- 27.Abraham WT, Fisher WG, Smith AL, et al. Cardiac resynchronization in chronic heart failure. N Engl J Med 2002;346:1845–53. [DOI] [PubMed] [Google Scholar]
- 28.Priori SG, Aliot E, Blomstrom-Lundqvist C, et al. Update of the guidelines on sudden cardiac death of the European Society of Cardiology. Eur Heart J 2003;24:13–5. ▸ This paper outlines recent updates to ESC guidelines on sudden cardiac death incorporating data from MADIT II and CAT. Further recommendations will follow with the publication of additional important trials of the prevention sudden cardiac death. [DOI] [PubMed] [Google Scholar]
- 29.AVID Investigators. A comparison of antiarrhythmic-drug therapy with implantable defibrillators in patients resuscitated from near-fatal ventricular arrhythmias. The antiarrhythmics versus implantable defibrillators (AVID) investigators. N Engl J Med 1997;337:1576–83. [DOI] [PubMed] [Google Scholar]
- 30.Connolly SJ, Gent M, Roberts RS, et al. Canadian implantable defibrillator study (CIDS): a randomized trial of the implantable cardioverter defibrillator against amiodarone. Circulation 2000;101:1297–302. [DOI] [PubMed] [Google Scholar]
- 31.Strickberger SA, Hummel JD, Bartlett TG, et al. Amiodarone versus implantable cardioverter-defibrillator:randomized trial in patients with nonischemic dilated cardiomyopathy and asymptomatic nonsustained ventricular tachycardia—AMIOVIRT. J Am Coll Cardiol 2003;41:1707–12. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.