Abstract
The occurrence of peptic ulcer increased rapidly in all Western countries from the 19th to the 20th century, attributed to a possible epidemic of Helicobacter pylori, a new pathogenic strain, or a change in host susceptibility. The early trends in hospital admissions for peptic ulcer and dyspepsia in London and New York during the 19th century are reviewed to test these hypotheses.
Keywords: peptic ulcer, gastric ulcer, duodenal ulcer, epidemiology
The occurrence of peptic ulcer showed a rapid increase in all Western countries from the turn of the 19th to the 20th century. Because almost all patients with gastric and duodenal ulcers not caused by non-steroidal anti-inflammatory drugs are infected with Helicobacter pylori, it has been widely assumed that these time trends in peptic ulcer rates were due to an epidemic of H pylori, a new pathogenic strain, or a change in host susceptibility. In the present short report, we review the early trends in hospital admissions for peptic ulcer and dyspepsia in London and New York during the 19th century to assess whether the statistical data support any of these contentions.
HOSPITAL RECORDS IN THE 19TH CENTURY
Historical trends in peptic ulcer and indigestion have been studied by necropsy, hospital admissions and deaths, attendance at clinics, and diagnostic modalities, such as barium meals and endoscopy. We have previously analysed data on period and cohort age contours of deaths from gastric and duodenal ulcers registered in the USA from 1921 to 19881 and in New York City from 1804 to 1998.2
Anne Borsay3 has recently traced English medical statistics back to William Petty in 1676, and James Jurin in the 1720s, with annual reports from some of the new voluntary hospitals from these dates onwards. We present data on admissions to the major teaching hospitals in London and New York from the 1840s. By that time hospital diagnostic record keeping had improved and annual reports became common practice. The published data were no longer merely records of the number of admissions, discharges, and deaths each year, enough to satisfy quantitatively the subscribers to these charitable institutions. It became the custom to also tabulate diagnoses, which became increasingly reliable with the pressure to try and obtain a post mortem examination on every death,4 to advance the science of medicine, and to satisfy public health movements by providing accurate figures of diseases and death for health reforms.
TRENDS IN PEPTIC ULCER IN LONDON AND NEW YORK
Gastric ulcer
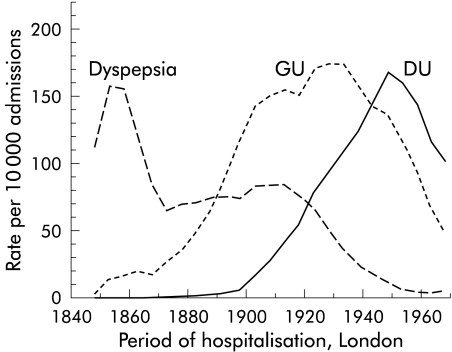
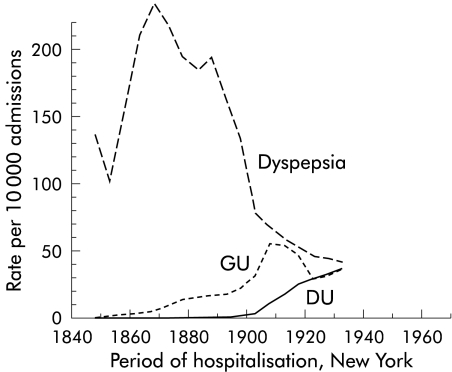
The earliest recorded admissions for gastric ulcer were in the 1840s in both cities, which increased rapidly to a maximum in about 1910 and then declined. However, the increase in admissions in London was far greater than that in New York, with a fourfold difference by 1920 (figs 1, 2 ▶ ▶).
Figure 1.
Admissions for gastric (GU) and duodenal (DU) ulcers, and dyspepsia in all 12 London hospitals associated with a medical school. Gastric ulcer, duodenal ulcer, and “dyspepsia” (including indigestion, gastralgia, and gastritis) are presented as mean rates per 10 000 admission in each five year period. To further smooth out missing time periods and various lengths of data availability from individual hospitals, the data were plotted as the moving average of three consecutive time periods.
Figure 2.
Admissions for gastric (GU) and duodenal (GU) ulcers, and dyspepsia from 10 hospitals in New York, analysed similarly as the London hospitals (see fig 1 ▶).
Duodenal ulcer
Duodenal ulcer was seen at necropsy in the Middlesex Hospital in the 1850s. Admissions for duodenal ulcer were recorded in both cities in the 1860s but became rapidly more common in London, rising to a peak by about 1950. However, in New York the rise in admissions was far less but we could find no data after 1930 (figs 1, 2 ▶ ▶). In both cities the increase in admissions for duodenal ulcer occurred about 20 years after that for gastric ulcers, and then increased in parallel and declined.
Dyspepsia
In contrast, admissions for dyspepsia were common in both cities in the 1840s but increased rapidly in New York to double the rate in London, decreasing equally rapidly until this diagnosis became rare after the 1940s (figs 1, 2 ▶ ▶).
St Bartholomew's Hospital
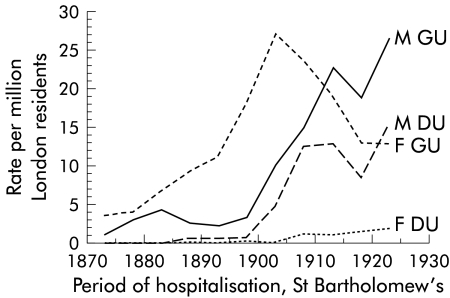
These detailed data (fig 3 ▶) show not only that the rise in gastric ulcer preceded that of duodenal ulcer, but also that the rise in women with gastric ulcer preceded the rise in men with gastric ulcer, and was followed by a rise in men with duodenal ulcer. Overall, women with gastric ulcer admitted to this hospital were predominantly young with a mean (range) percentage under 30 years of 58 (34–70)% rising from 50% in the 1870s to 72% in the 1890s, and falling to 38% in the 1910s. However, men with gastric ulcer were mostly over 30 years (81 (75–90)%) as were patients with duodenal ulcer (both males (79 (67–93)%) and females (83 (55–100)%)).
Figure 3.
Rates of admission per million London residents of males (M) and females (F) with gastric (GU) and duodenal (DU) ulcer to St Bartholomew's Hospital, London, 1872–1920, during which period the mean necropsy rate was 79%. Age and sex specific rates were calculated for each five year period and 10 year age group per million living London residents, using the method of direct standardisation to adjust the rates of different time periods to the age distribution of the census population of London from 1921.
Case fatality rates were expressed as ulcer deaths per all ulcer cases, and their 95% confidence intervals (CI) estimated from their binomial distribution. The rates were considered significantly different if their CI did not overlap. During the half century 1872–1925, the overall percentage case fatality rate in this hospital (mean (95% CI)) for admissions for peptic ulcer was 12.9% (11.9–14.0), and significantly higher for duodenal (14.8% (13.9–15.7)) than gastric (12.5% (12.1–12.8)) ulcers. Rates were significantly higher for men with peptic ulcers (17.0% (16.4–17.6)) than for women (8.7% (8.3–9.0)).
CAVEATS
The mean (range) necropsy rates in eight of the 12 London teaching hospitals for which we have found data was 83 (33–116)%, with little difference between hospitals. However, the mean necropsy rate in the seven New York hospitals for which we have data was only 32 (4–84)%.
“From the 1890s, elective and emergency operations for peptic ulcers were increasingly performed, allowing diagnoses as definitive in life as those at necropsy”
Today one can obtain valid incidences of gastric and duodenal ulcers by endoscopy of whole populations, or random samples. However, contrast radiology of peptic ulcer was not common until the 1920s, and endoscopy by fibreoptics not until the 1970s, so that diagnosis of these ulcers during most of the time periods of the current report was essentially clinical, based on suggestive clinical histories supported by correlation with necropsies. From the 1890s, elective and emergency operations for peptic ulcers were increasingly performed, allowing diagnoses as definitive in life as those at necropsy. However, while some of the differences over time and between and within cities could be due to differences in trends and fashions in diagnosis, they cannot explain the differences between men and women, and between gastric and duodenal ulcers.
TRENDS IN OTHER CITIES
Gastric ulcer
Rates of admissions for gastric ulcer varied considerably between different hospitals in each city, as had been reported for various hospitals within the cities of Baltimore, Boston, Montreal, and Philadelphia, possibly as a result of the differences in the populations served rather than the diagnostic criteria of the clinicians.5 The admission rate in the early years of the 20th century was about 50 per 10 000 admissions in New York, higher than Cleveland (38), Baltimore (37), Philadelphia (16), Chicago (15), and Denver (5).6 However, the New York rate (50) was markedly lower than in Montreal (92) and Boston (128).5,6
“Rates of admissions for gastric ulcer varied considerably between different hospitals in each city”
Although the rates increased in similar decades in the two cities, far higher rates were reached in London (150) and Berlin (133)5 and even higher further north in Edinburgh (202).7 In Philadelphia in 1827, “ulceration of the stomach is of rare occurrence”,8 in 1860 “its occurrence must be far rarer than in England or on the continent of Europe”,9 and in 1869 two physicians had never seen a fatal case of simple gastric ulcer in 25 years in either private or hospital practice; they explained this rarity to the “mode of living”.10 In contrast, in 1886 it was suggested that the low frequency of gastric ulcer in the USA was because “they are less carefully sought for”.11
Duodenal ulcer
As with gastric ulcer, the rates of duodenal ulcer varied between the different hospitals in each city, and again there were far higher rates of admission in London. It is interesting to compare the precise years when the admission rates for duodenal ulcer exceeded those for gastric ulcer. In London it was 1938 at the Royal Free and 1948 at St Bartholomew's; in New York it was 1925 at Bellevue. It is possible that duodenal ulcers were missed at necropsy because either the duodenums were not examined routinely or that ulcers in the duodenal bulb were misinterpreted as prepyloric gastric ulcers. However, those who performed post mortem examinations in the 19th century were not likely to have made such errors.
Data from St Bartholomew's Hospital show a clear pattern of successive increases in women with gastric ulcer (mostly young), followed 10–20 years later by men with gastric ulcer (mostly older), followed a decade later by men with duodenal ulcer.
TRENDS IN DYSPEPSIA
In the 1790s and early 19th century, patients with upper abdominal pain or discomfort were usually diagnosed as having indigestion, dyspepsia, and occasionally gastralgia or gastrodynia. From 1799 to 1801 there were 3336 admissions to medical beds in Westminster Hospital, London, of which 158 (470 per 10 000) were for dyspepsia.12 This rate was comparable with admission rates for dyspepsia in Sunderland, England13 in 1803 and in Glasgow, Scotland14 of 376 and 723 per 10 000. In contrast, in a New York Hospital in 1795–1799, only five of 2005 admissions (25 per 10 000) were for dyspepsia. As with gastric and duodenal ulcers, the rates of these non-specific diagnoses varied within cities between the different hospitals. However, by the 1850s admissions rates increased, and were higher in New York than in London, reaching a peak in about 1870, and then falling in both cities to negligible numbers by the middle of the 20th century.
There is no obvious explanation for the high rates of diagnosis of dyspepsia in New York in the middle of the 19th century. In 1878 “all forms of dyspepsia are incomparably more frequent in this country than in Europe”.15 In 1882 the British Medical Journal claimed that “the prevalent dyspepsia from which Americans suffer so much, and which is so apt to undermine the strength of the men and the bloom of the women of America, is in a large measure due, we believe, to the universal habit of drinking large quantities of ice-water”.16 In 1896 “in the distribution of diseases among nations, the English got gout, the French syphilis, and the Americans dyspepsia. But our friends the pathologists tell us there is no such disease as dyspepsia. As a pathological entity it does not exist; as a clinical condition one meets it almost every day of our lives”.17
“There is no obvious explanation for the high rates of diagnosis of dyspepsia in New York in the middle of the 19th century”
These high rates of non-specific dyspepsia in New York were unlikely to have been due to structural disease or to under diagnosis of gastric ulcer because of the absence, or markedly low rates, of necropsy in that city.
CONCLUSIONS
It is difficult to explain why in both cities, and in other hospitals in Europe and North America, there were rapid increases in the rates of admission for gastric and, 10–20 years later, for duodenal ulcers. Certainly these time periods correspond with our USA1 and New York2 mortality data that showed a peak mortality for gastric ulcer for those born in the 1870s, and for duodenal ulcer for those born in the 1880s. We cannot explain these differences in time trends nor that the initial increases in peptic ulcer in the 19th century began in Britain18 and Denmark19 in young women with gastric ulcer, and that duodenal ulcer was predominantly male.
These extraordinary increases in peptic ulcer in the 19th century have been attributed to a postulated increase in an (cross) infectious disease (H pylori) in childhood, spread perhaps by the overcrowding and poor sanitation of early urbanisation.1 Or there may have been a new and more pathogenic strain of H pylori, a change in host susceptibility, 20 or even a concurrent enteric infection modulating gastric inflammation and immune responses.21 However, these suggestions remain as yet untestable hypotheses, and do not explain the temporal changes in gastric versus duodenal ulcer and men versus women described and discussed above.
Supplementary Material
Acknowledgments
We are grateful for the help of many hospital archivists and librarians.
APPENDIX
REFERENCES
- 1.Sonnenberg A. The US temporal and geographic variation of diseases related to Helicobacter pylori. Am J Public Health 1993;83:1006–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Baron JH, Sonnenberg A. Period- and cohort-age contours of deaths from gastric and duodenal ulcer in New York 1804–1908. Am J Gastroenterol 2001;96:2887–91. [DOI] [PubMed] [Google Scholar]
- 3.Borsay A. An example of political arithmetic: the evaluation of spa therapy at the Georgian Bath Infirmary, 1742–1830. Med Hist 2000;45:149–72. [PMC free article] [PubMed] [Google Scholar]
- 4.Baron JH. Clinical diagnosis and the function of necropsy. J R Soc Med 2000;93:463–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Howard CP. The incidence of gastric ulcer in America. Med News 1904;85:673–5. [Google Scholar]
- 6.Greenough RB, Joplin EP. Gastric ulcer at the Massachusetts General Hospital, 1888–1898. Am J Med Sci 1899;118:167–83. [Google Scholar]
- 7.Bramwell B. A clinical lecture on the statistics of gastric ulcer, with special reference to gastric haemorrhage, its frequency and fatality. Lancet 1901;1:687–91. [Google Scholar]
- 8.Rogers DL. Ulcerated stomach. Philad J Med Phys Sci 1827;14:115. [Google Scholar]
- 9.Keating WV. Ulcer of the stomach. Proc Path Soc Philad 1860;1:141–2. [Google Scholar]
- 10.Oliver HK. Gastric ulcer. Boston Med Surg J 1869;80:207–13. [Google Scholar]
- 11.Wood HC. Case of perforating ulcer of the stomach. Therap Gaz Detroit 1886;2:153–5. [Google Scholar]
- 12.Bradley T. Admissions to Westminster Hospital London. Med Physical J 1799;1:110–11 to 1802;6:391. [Google Scholar]
- 13.Wilkinson G. Report of disease in the parish workhouse of Sunderland. Med Physical J 1803;10:455. [PMC free article] [PubMed] [Google Scholar]
- 14.Anonymous. Medical Report of Glasgow Infirmary for 1810. Edinburgh Med Surg J 1811;7:246–9. [Google Scholar]
- 15.Neftel WB. The treatment of some forms of dyspepsia (chronic catarrh of the stomach). Med Rec 1878;13:443–9. [Google Scholar]
- 16.Editorial. BMJ 1882;1:280. [Google Scholar]
- 17.Huston Wo. The American disease. Columbus Med J 1896;16:1–6. [Google Scholar]
- 18.Jennings FD. Perforated peptic ulcer. Changes in age-incidence and sex-distribution in the last 150 years. Lancet 1940;1:395–8, 444–7. [Google Scholar]
- 19.With C. The clinical picture, diagnosis and treatment of gastric ulcer. Copenhagen: Gyldendal, 1881. Cited by Wulff HR. Rational diagnosis and treatment: an introduction to clinical decision-making, 2nd Edn. Oxford: Blackwell Scientific, 1981:62–3.
- 20.Malaty HM, Engstrond L, Pederson NL, et al. Helicobacter pylori infection: genetic and environmental influences: a study of twins. Ann Intern Med 1994;120:982–6. [DOI] [PubMed] [Google Scholar]
- 21.Lee JG, Beck B, Dongler CA, et al. Concurrent enteric helminth infection modulates inflammation and gastric immune responses and reduces gastric Helicobacter-induced gastric atrophy. Nat Med 2000;6:536–42. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.