Clinical presentation
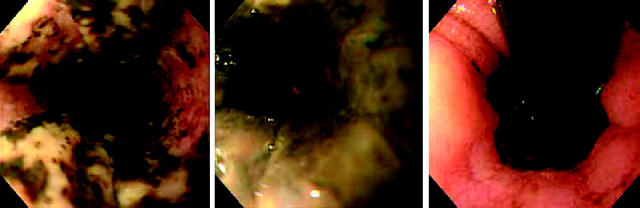
A 64 year old woman was admitted with coffee ground emesis. She had been bedridden for the previous two years due to osteoarthritis but had no past history of upper gastrointestinal ulcer, gastro-oesophageal reflux disease, or corrosive intake. Initial upper endoscopy revealed a patchy black appearance of the oesophageal mucosa extending from the proximal third of the oesophagus, with adherent yellow exudates, which became circumferential in the distal third of the oesophagus (fig 1 ▶). The black mucosa showed a sharp boundary at the gastro-oesophageal mucosal junction (fig 1 ▶), and the gastric and duodenal mucosa showed a normal appearance. The patient was treated with intravenous ranitidine for seven days and oral ranitidine thereafter. Endoscopy one week later revealed that the oesophageal mucosa was diffusely covered by thin whitish exudates with no stenosis, and biopsies revealed ulcerated mucosa with massive necrosis.
Figure 1.
Upper gastrointestinal endoscopy of the oesophagus revealing a diffusely black mucosa that ends sharply at the gastro-oesophageal mucosal junction.
Question
What is the diagnosis?
See page 227 for answer
This case is submitted by: