Abstract
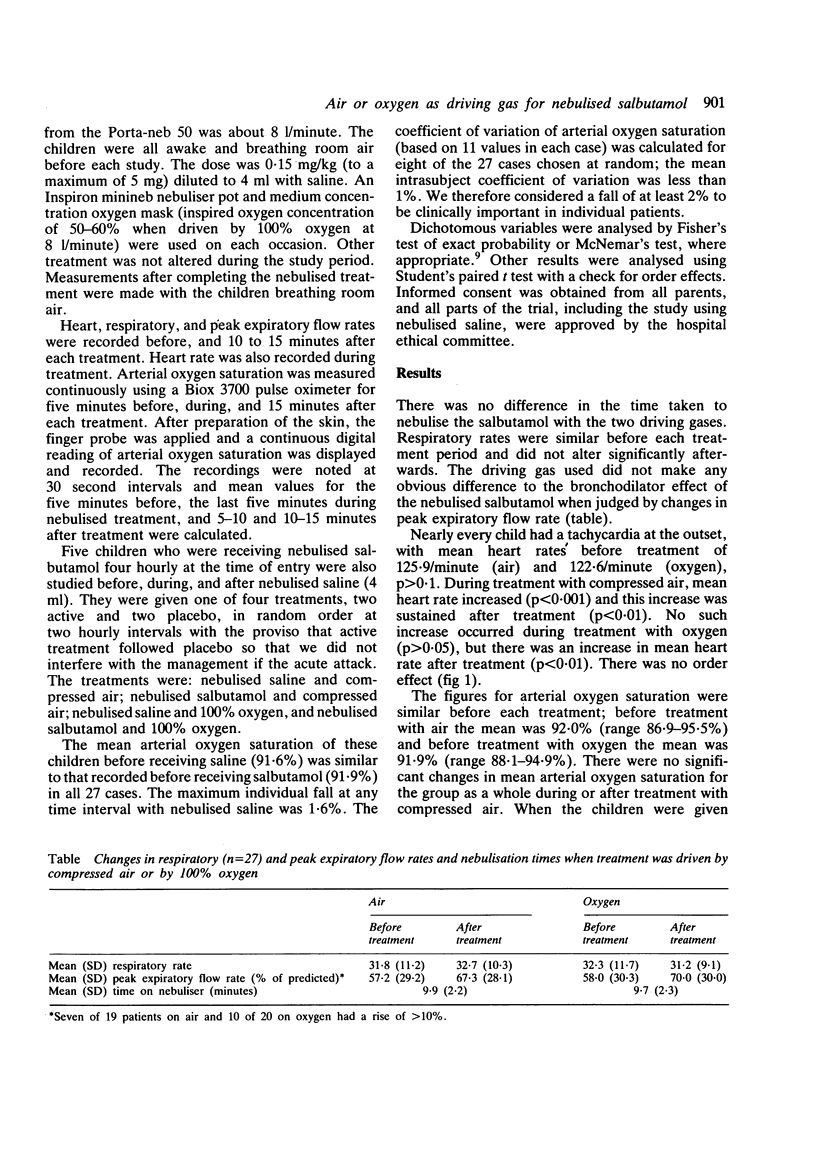
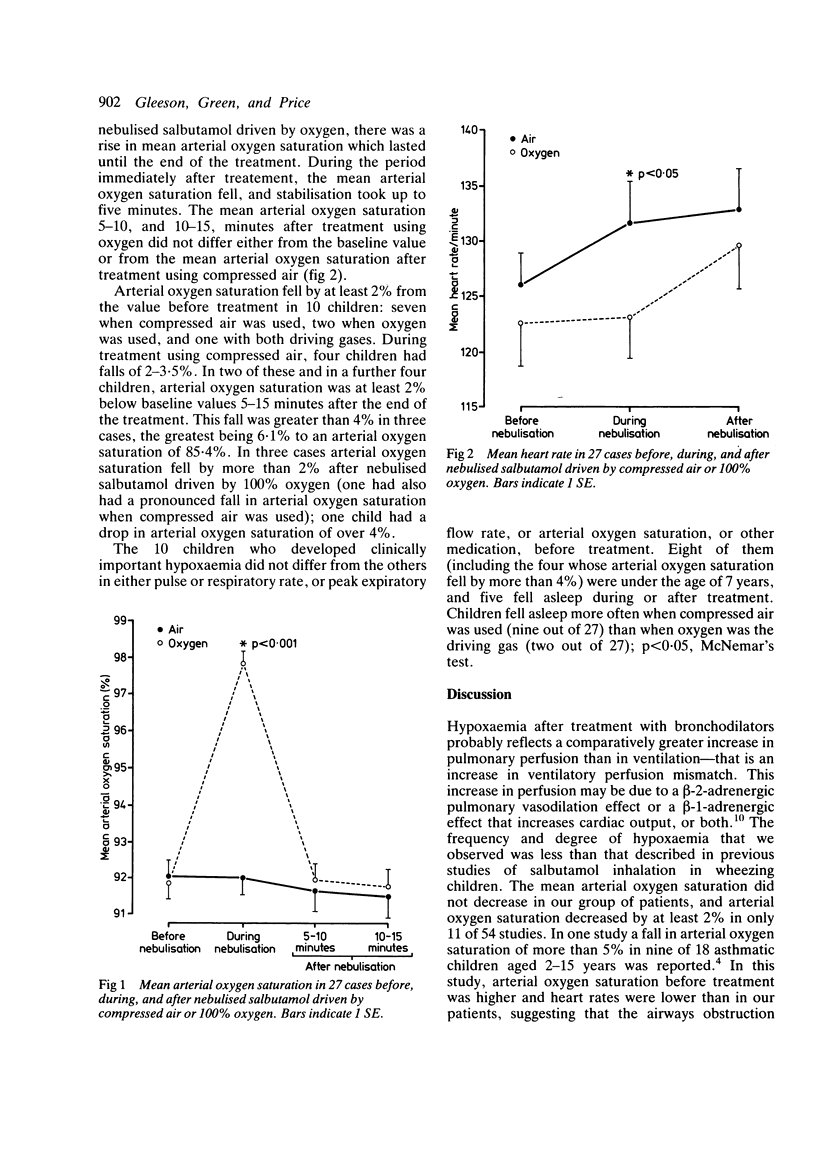
The effects of nebulised salbutamol driven by compressed air or oxygen were compared in a randomised crossover study during 27 attacks of acute asthma. Arterial oxygen saturation fell by 2-6% during or after treatment in 10 cases: seven with compressed air, two with oxygen, and one with both driving gases. Hypoxaemia occurred in younger children and in those who fell asleep, but was not related to the level of arterial oxygen saturation before treatment or the size of the response to bronchodilator therapy. More children fell asleep with compressed air nebulisation. Arterial oxygen saturation improved and heart rates remained stable during treatment when oxygen was the driving gas. After treatment, however, arterial oxygen saturation fell and heart rates rose to values that were similar to those after treatment with compressed air. The falls in arterial oxygen saturation we observed, though comparatively small, would be clinically important on the steep part of the oxygen dissociation curve, and our results emphasise that families with home nebulisers should seek medical advice early when their children develop severe asthma. The benefits of using oxygen as the driving gas during nebulisation were transient, and in severe asthma treatment with oxygen needs to be continued after the nebulised salbutamol has been given.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Catterall J. R., Douglas N. J., Calverley P. M., Brash H. M., Brezinova V., Shapiro C. M., Flenley D. C. Irregular breathing and hypoxaemia during sleep in chronic stable asthma. Lancet. 1982 Feb 6;1(8267):301–304. doi: 10.1016/s0140-6736(82)91567-7. [DOI] [PubMed] [Google Scholar]
- Harris L. Comparison of the effect on blood gases, ventilation, and perfusion of isoproterenol-phenylephrine and salbutamol aerosols in chronic bronchitis with asthma. J Allergy Clin Immunol. 1972 Feb;49(2):63–71. doi: 10.1016/0091-6749(72)90057-7. [DOI] [PubMed] [Google Scholar]
- Prendiville A., Green S., Silverman M. Paradoxical response to nebulised salbutamol in wheezy infants, assessed by partial expiratory flow-volume curves. Thorax. 1987 Feb;42(2):86–91. doi: 10.1136/thx.42.2.86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prendiville A., Rose A., Maxwell D. L., Silverman M. Hypoxaemia in wheezy infants after bronchodilator treatment. Arch Dis Child. 1987 Oct;62(10):997–1000. doi: 10.1136/adc.62.10.997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sears M. R., Rea H. H., Fenwick J., Gillies A. J., Holst P. E., O'Donnell T. V., Rothwell R. P. 75 deaths in asthmatics prescribed home nebulisers. Br Med J (Clin Res Ed) 1987 Feb 21;294(6570):477–480. doi: 10.1136/bmj.294.6570.477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solimano A. J., Smyth J. A., Mann T. K., Albersheim S. G., Lockitch G. Pulse oximetry advantages in infants with bronchopulmonary dysplasia. Pediatrics. 1986 Nov;78(5):844–849. [PubMed] [Google Scholar]
- Southall D. P., Bignall S., Stebbens V. A., Alexander J. R., Rivers R. P., Lissauer T. Pulse oximeter and transcutaneous arterial oxygen measurements in neonatal and paediatric intensive care. Arch Dis Child. 1987 Sep;62(9):882–888. doi: 10.1136/adc.62.9.882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tal A., Pasterkamp H., Leahy F. Arterial oxygen desaturation following salbutamol inhalation in acute asthma. Chest. 1984 Dec;86(6):868–869. doi: 10.1378/chest.86.6.868. [DOI] [PubMed] [Google Scholar]


