Abstract
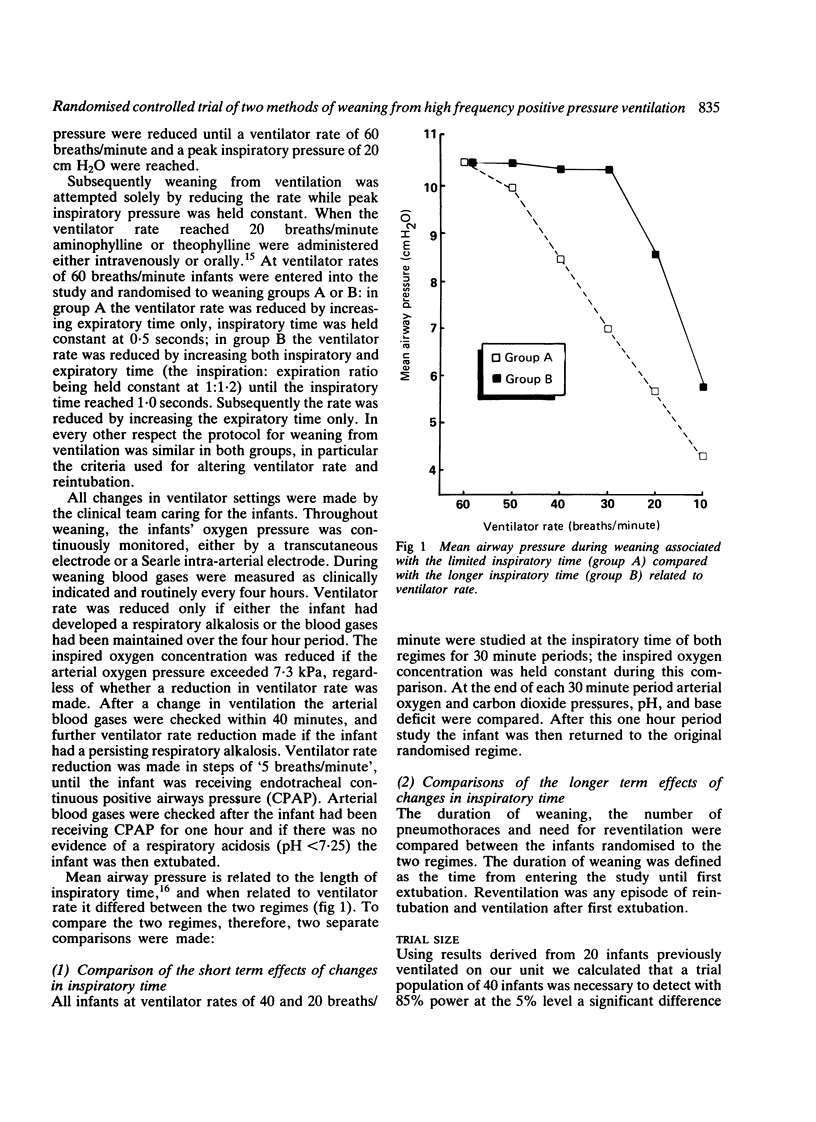
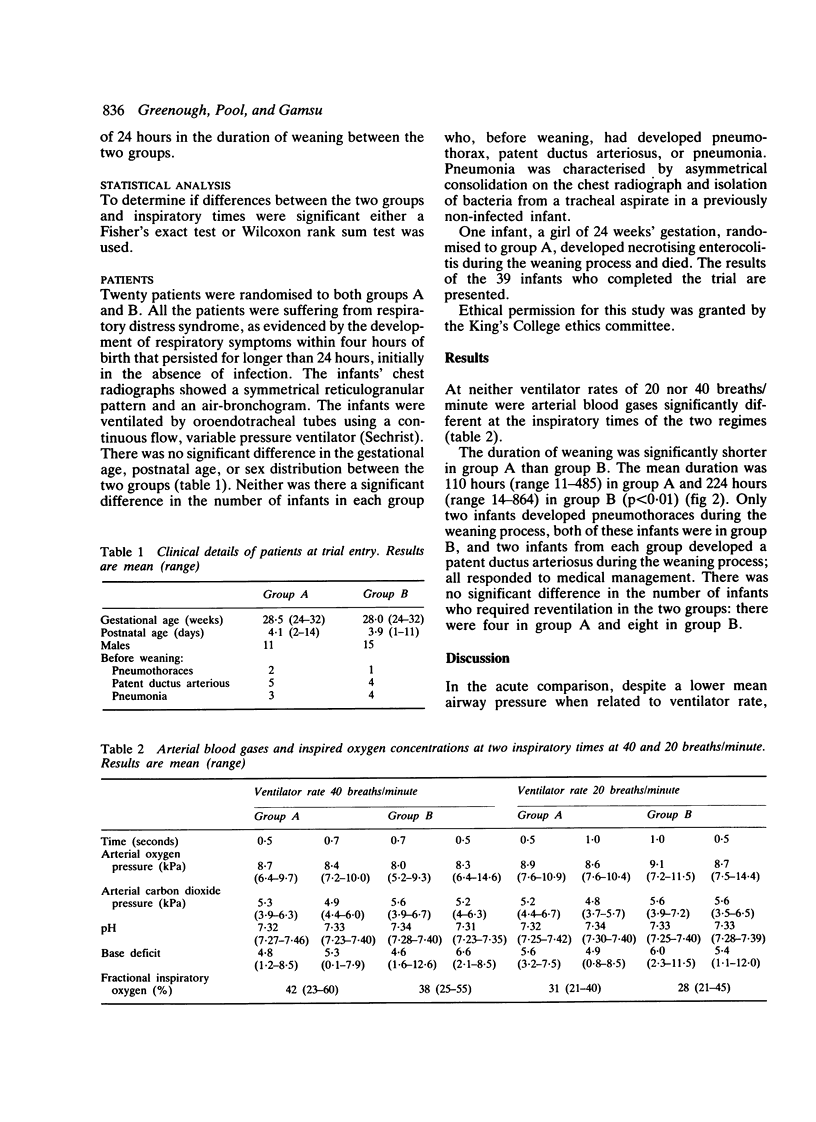
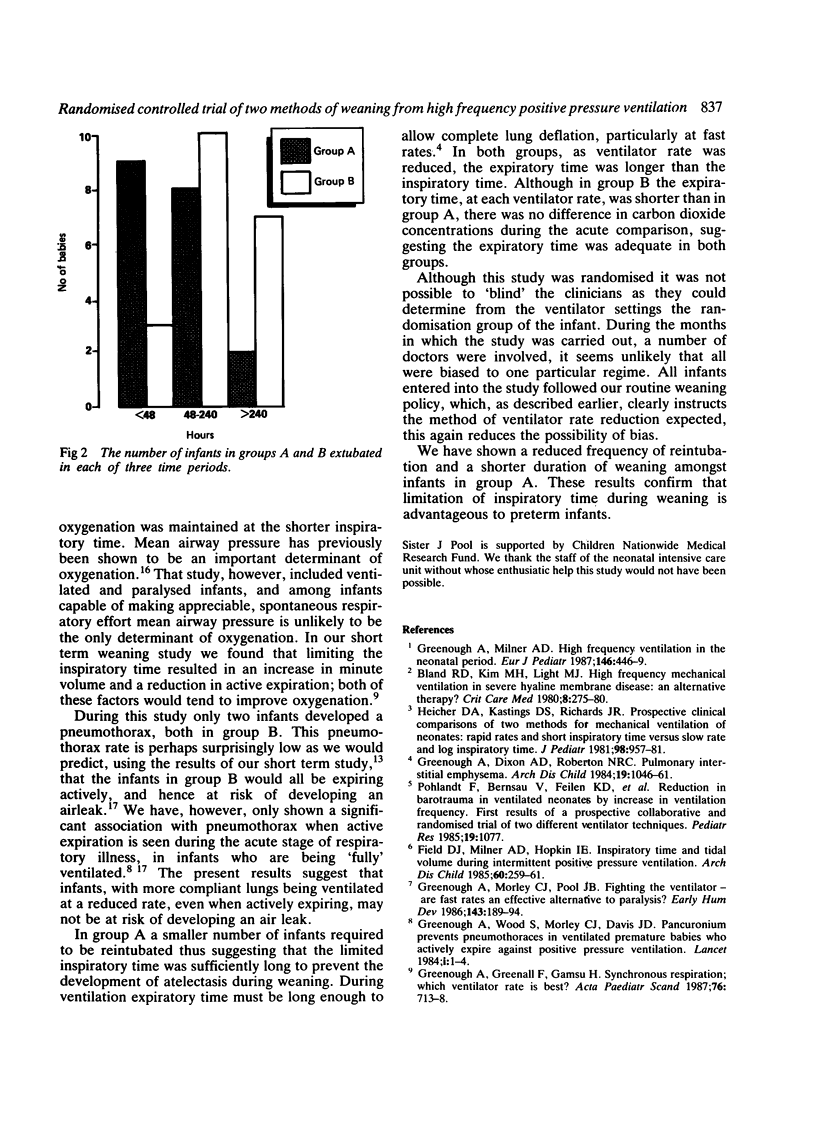
Forty preterm infants suffering from respiratory distress syndrome were entered into a randomised controlled trial to assess the importance of the length of inspiratory time during weaning from high frequency positive pressure ventilation (HFPPV). Two weaning regimes were compared: in one (group A) inspiratory time was limited to 0.5 seconds throughout weaning, in the other (group B) ventilator rate was reduced by increasing both inspiratory and expiratory time (inspiration:expiration ratio constant) until inspiratory time reached 1.0 seconds. At ventilator rates of 20 and 40 breaths/minute an acute comparison was made in all 40 infants of the two inspiratory times; despite the lower mean airway pressure associated with the shorter inspiratory time blood gases were maintained. There was no difference in the incidence of pneumothoraces or need for reventilation between the two regimens but infants in group A had a shorter duration of weaning. We conclude limitation of inspiratory time to 0.5 seconds during weaning from HFPPV is advantageous to preterm infants with respiratory distress syndrome.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bland R. D., Kim M. H., Light M. J., Woodson J. L. High frequency mechanical ventilation in severe hyaline membrane disease an alternative treatment? Crit Care Med. 1980 May;8(5):275–280. doi: 10.1097/00003246-198005000-00001. [DOI] [PubMed] [Google Scholar]
- Boros S. J. Variations in inspiratory:expiratory ratio and airway pressure wave form during mechanical ventilation: the significance of mean airway pressure. J Pediatr. 1979 Jan;94(1):114–117. doi: 10.1016/s0022-3476(79)80372-8. [DOI] [PubMed] [Google Scholar]
- Field D., Milner A. D., Hopkin I. E. Inspiratory time and tidal volume during intermittent positive pressure ventilation. Arch Dis Child. 1985 Mar;60(3):259–261. doi: 10.1136/adc.60.3.259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenough A., Dixon A. K., Roberton N. R. Pulmonary interstitial emphysema. Arch Dis Child. 1984 Nov;59(11):1046–1051. doi: 10.1136/adc.59.11.1046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenough A., Elias-Jones A., Pool J., Morley C. J., Davis J. A. The therapeutic actions of theophylline in preterm ventilated infants. Early Hum Dev. 1985 Oct;12(1):15–22. doi: 10.1016/0378-3782(85)90132-x. [DOI] [PubMed] [Google Scholar]
- Greenough A., Greenall F., Gamsu H. R. Inspiratory times when weaning from mechanical ventilation. Arch Dis Child. 1987 Dec;62(12):1269–1270. doi: 10.1136/adc.62.12.1269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenough A., Greenall F., Gamsu H. Synchronous respiration: which ventilator rate is best? Acta Paediatr Scand. 1987 Sep;76(5):713–718. doi: 10.1111/j.1651-2227.1987.tb10554.x. [DOI] [PubMed] [Google Scholar]
- Greenough A., Milner A. D. High frequency ventilation in the neonatal period. Eur J Pediatr. 1987 Sep;146(5):446–449. doi: 10.1007/BF00441591. [DOI] [PubMed] [Google Scholar]
- Greenough A., Morley C. J., Pool J. Fighting the ventilator--are fast rates an effective alternative to paralysis? Early Hum Dev. 1986 Apr;13(2):189–194. doi: 10.1016/0378-3782(86)90007-1. [DOI] [PubMed] [Google Scholar]
- Greenough A., Morley C., Davis J. Interaction of spontaneous respiration with artificial ventilation in preterm babies. J Pediatr. 1983 Nov;103(5):769–773. doi: 10.1016/s0022-3476(83)80483-1. [DOI] [PubMed] [Google Scholar]
- Greenough A., Pool J., Greenall F., Morley C., Gamsu H. Comparison of different rates of artificial ventilation in preterm neonates with respiratory distress syndrome. Acta Paediatr Scand. 1987 Sep;76(5):706–712. doi: 10.1111/j.1651-2227.1987.tb10553.x. [DOI] [PubMed] [Google Scholar]
- Greenough A. The premature infant's respiratory response to mechanical ventilation. Early Hum Dev. 1988 May;17(1):1–5. doi: 10.1016/s0378-3782(88)80051-3. [DOI] [PubMed] [Google Scholar]
- Greenough A., Wood S., Morley C. J., Davis J. A. Pancuronium prevents pneumothoraces in ventilated premature babies who actively expire against positive pressure inflation. Lancet. 1984 Jan 7;1(8367):1–3. doi: 10.1016/s0140-6736(84)90177-6. [DOI] [PubMed] [Google Scholar]
- Heicher D. A., Kasting D. S., Harrod J. R. Prospective clinical comparison of two methods for mechanical ventilation of neonates: rapid rate and short inspiratory time versus slow rate and long inspiratory time. J Pediatr. 1981 Jun;98(6):957–961. doi: 10.1016/s0022-3476(81)80604-x. [DOI] [PubMed] [Google Scholar]
- Primhak R. A. Factors associated with pulmonary air leak in premature infants receiving mechanical ventilation. J Pediatr. 1983 May;102(5):764–768. doi: 10.1016/s0022-3476(83)80254-6. [DOI] [PubMed] [Google Scholar]
- Ramsden C. A., Reynolds E. O. Ventilator settings for newborn infants. Arch Dis Child. 1987 May;62(5):529–538. doi: 10.1136/adc.62.5.529. [DOI] [PMC free article] [PubMed] [Google Scholar]


