Abstract
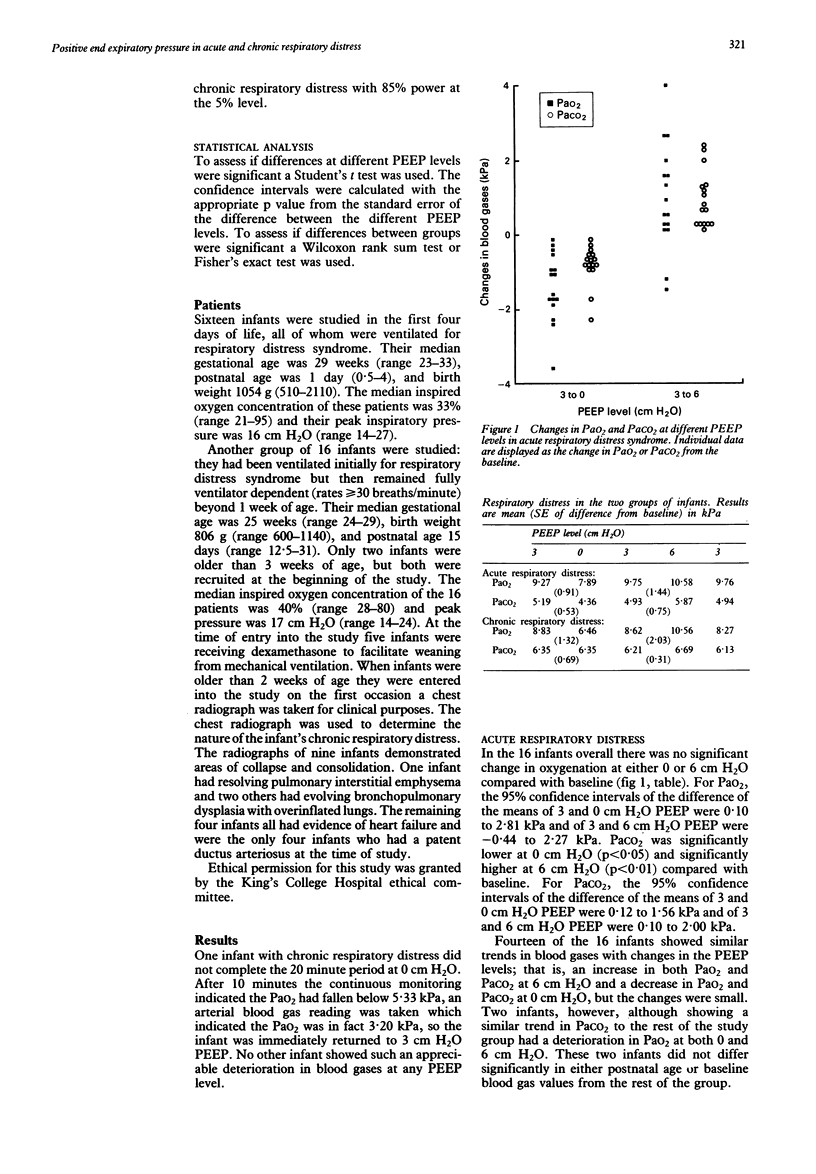
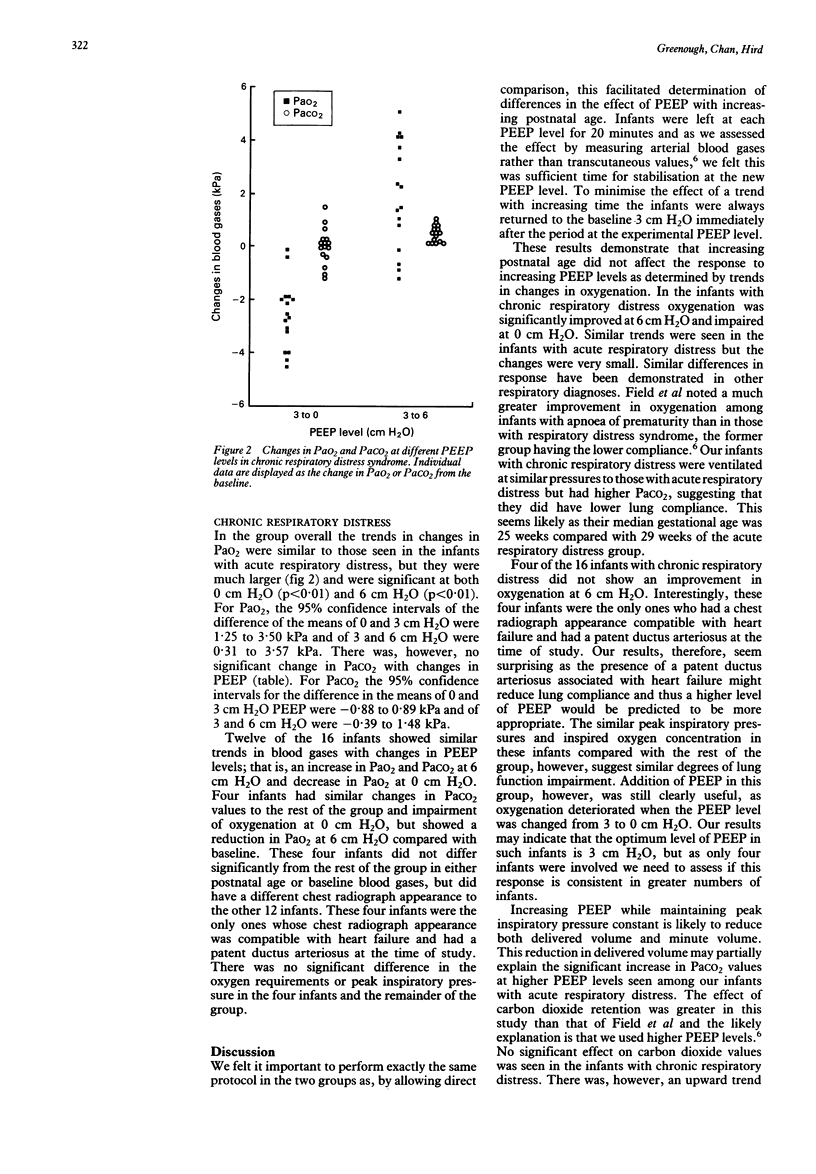
The optimum level of positive end expiratory pressure (PEEP) was determined in 16 infants with respiratory distress syndrome (median gestational age 29 weeks, median postnatal age 1 day) and in 16 infants with chronic respiratory distress (median gestational age 25 weeks, median postnatal age 15 days). All infants were studied at a PEEP sequence of 3, 0, 3, 6, and 3 cm H2O, all other ventilator parameters being kept constant. Each PEEP level was maintained for 20 minutes and at the end of each period arterial blood gas was checked. During acute respiratory distress syndrome there were no significant changes in oxygenation but arterial carbon dioxide tension (PaCO2) significantly decreased from a mean of 4.93 kPa at 3 cm H2O to 4.40 kPa at 0 cm H2O and increased to a mean of 5.87 kPa at 6 cm H2O. In the infants with chronic respiratory distress, oxygenation fell from a mean of 8.66 kPa at 3 cm H2O to 6.40 kPa at 0 cm H2O and improved at 6 cm H2O to a mean of 10.50 kPa. There were no significant changes in PaCO2. We conclude that addition of PEEP, up to 6 cm H2O, may be useful even after the first week of life. High levels of PEEP, however, have previously been reported, in certain infants, to result in circulatory disturbance. It is therefore important to assess the use of 6 cm H2O PEEP in a controlled study of longer term clinical outcome.
Full text
PDF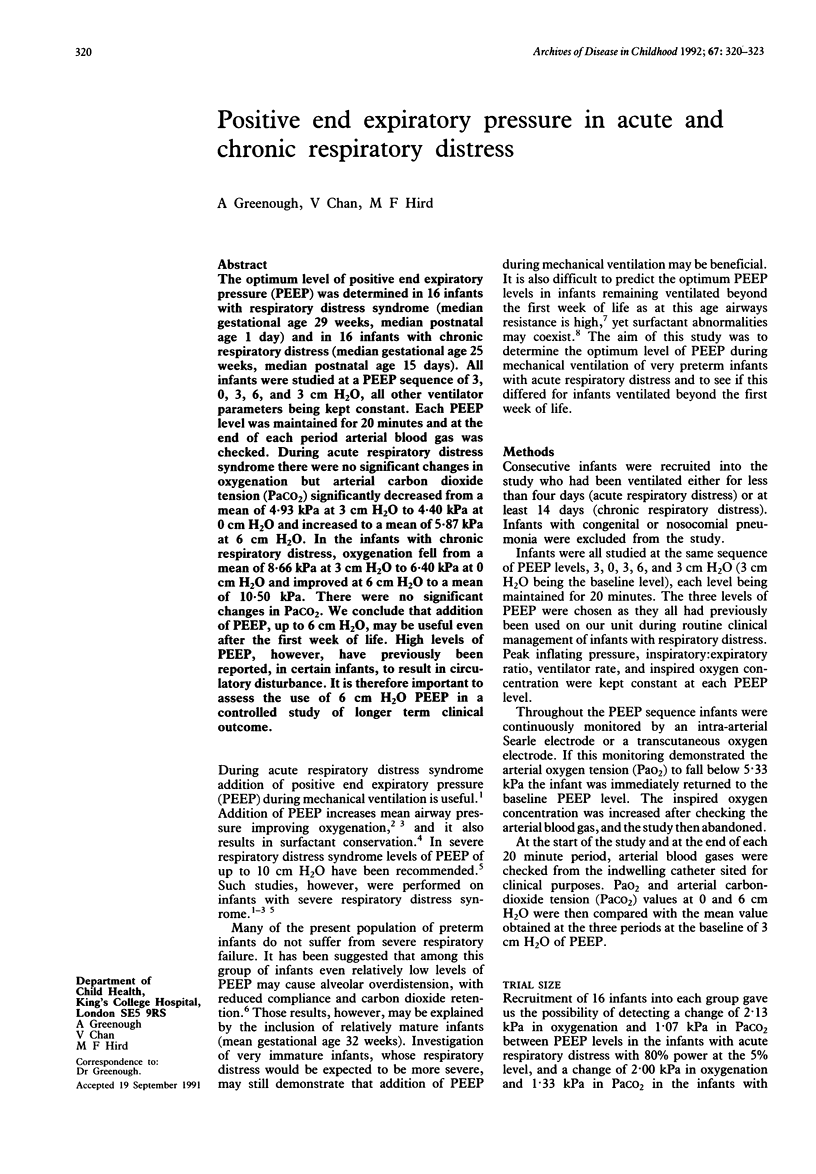

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Boros S. J., Campbell K. A comparison of the effects of high frequency--low tidal volume and low frequency--high tidal volume mechanical ventilation. J Pediatr. 1980 Jul;97(1):108–112. doi: 10.1016/s0022-3476(80)80146-6. [DOI] [PubMed] [Google Scholar]
- Boros S. J. Variations in inspiratory:expiratory ratio and airway pressure wave form during mechanical ventilation: the significance of mean airway pressure. J Pediatr. 1979 Jan;94(1):114–117. doi: 10.1016/s0022-3476(79)80372-8. [DOI] [PubMed] [Google Scholar]
- Chakrabarti M. K., Holdcroft A., Sapsed-Byrne S., Whitwam J. G. Circulatory depression with high peep in the surfactant-deficient rabbit. Br J Anaesth. 1989 Dec;63(6):732–735. doi: 10.1093/bja/63.6.732. [DOI] [PubMed] [Google Scholar]
- Field D., Milner A. D., Hopkin I. E. Effects of positive end expiratory pressure during ventilation of the preterm infant. Arch Dis Child. 1985 Sep;60(9):843–847. doi: 10.1136/adc.60.9.843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenough A. Bronchopulmonary dysplasia: early diagnosis, prophylaxis, and treatment. Arch Dis Child. 1990 Oct;65(10 Spec No):1082–1088. doi: 10.1136/adc.65.10_spec_no.1082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hyde I., English R. E., Williams J. D. The changing pattern of chronic lung disease of prematurity. Arch Dis Child. 1989 Apr;64(4 Spec No):448–451. doi: 10.1136/adc.64.4_spec_no.448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnston W. E., Vinten-Johansen J., Santamore W. P., Case L. D., Little W. C. Mechanism of reduced cardiac output during positive end-expiratory pressure in the dog. Am Rev Respir Dis. 1989 Nov;140(5):1257–1264. doi: 10.1164/ajrccm/140.5.1257. [DOI] [PubMed] [Google Scholar]
- Richardson C. P., Jung A. L. Effects of continuous positive airway pressure on pulmonary function and blood gases of infants with respiratory distress syndrome. Pediatr Res. 1978 Jul;12(7):771–774. doi: 10.1203/00006450-197807000-00006. [DOI] [PubMed] [Google Scholar]
- Stewart A. R., Finer N. N., Peters K. L. Effects of alterations of inspiratory and expiratory pressures and inspiratory/expiratory ratios on mean airway pressure, blood gases, and intracranial pressure. Pediatrics. 1981 Apr;67(4):474–481. [PubMed] [Google Scholar]
- Wilkie R. A., Bryan M. H. Effect of bronchodilators on airway resistance in ventilator-dependent neonates with chronic lung disease. J Pediatr. 1987 Aug;111(2):278–282. doi: 10.1016/s0022-3476(87)80087-2. [DOI] [PubMed] [Google Scholar]
- Wyszogrodski I., Kyei-Aboagye K., Taeusch H. W., Jr, Avery M. E. Surfactant inactivation by hyperventilation: conservation by end-expiratory pressure. J Appl Physiol. 1975 Mar;38(3):461–466. doi: 10.1152/jappl.1975.38.3.461. [DOI] [PubMed] [Google Scholar]


