Abstract
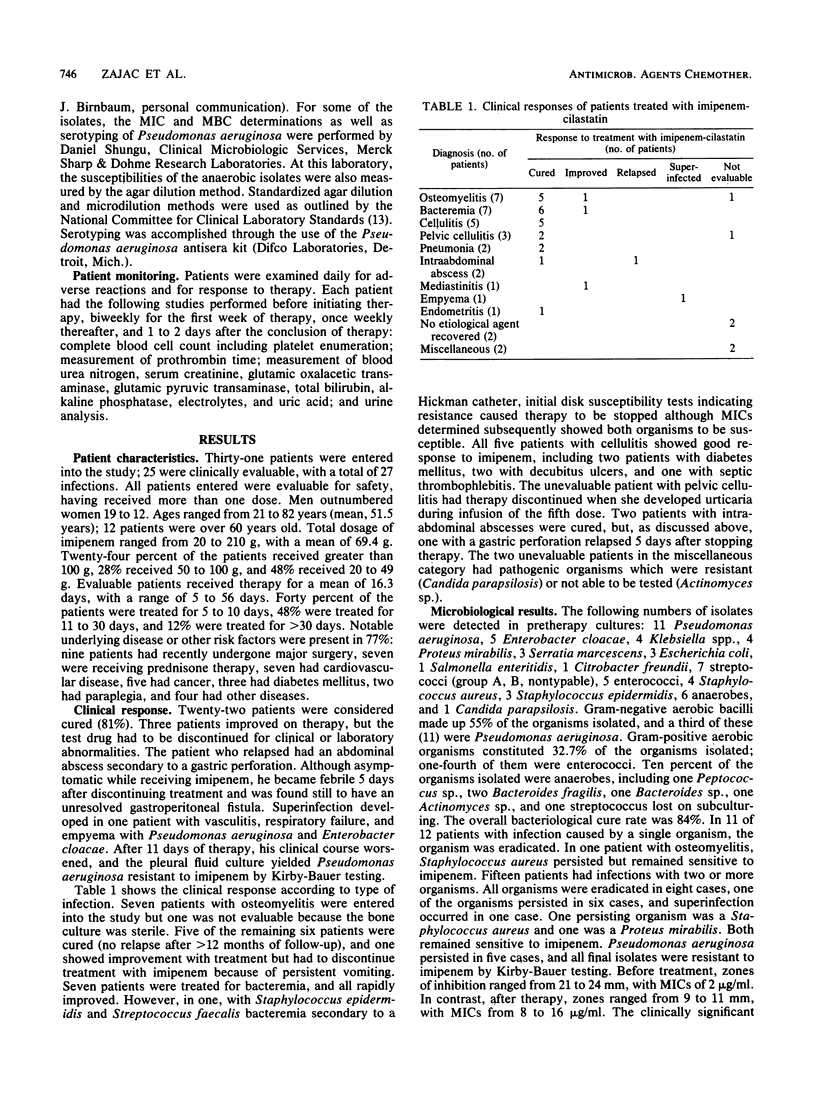
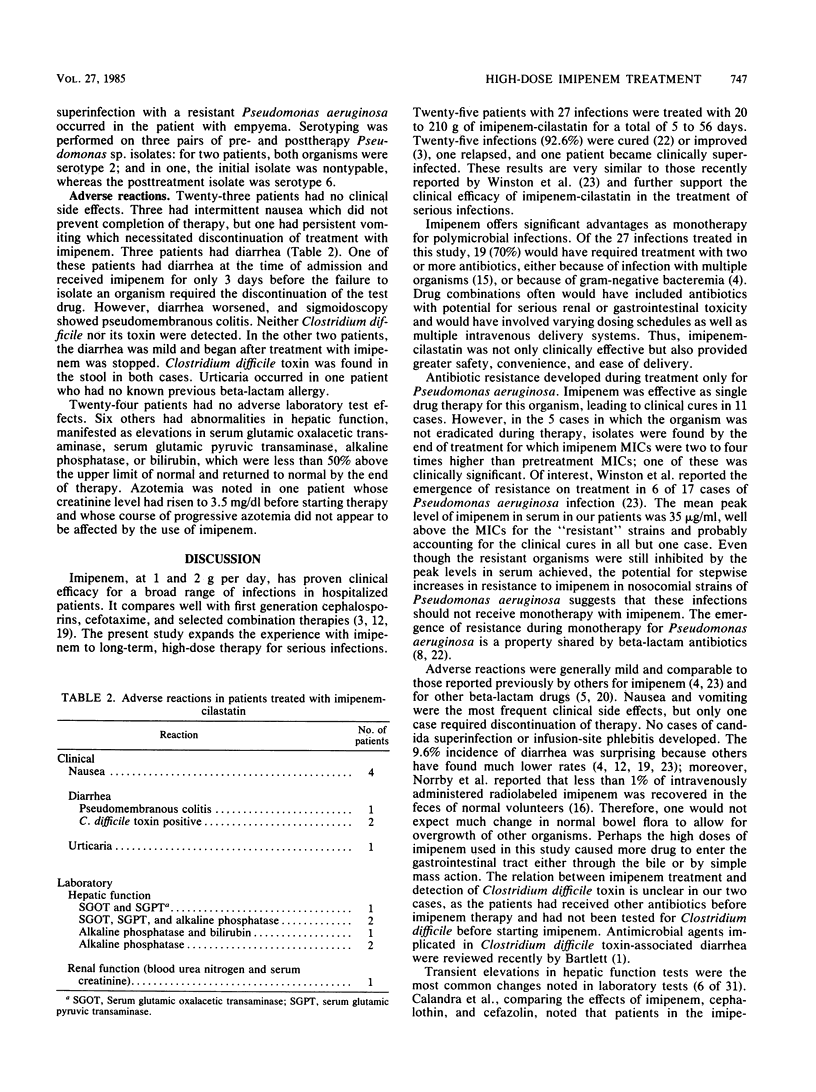
Imipenem-cilastatin was given in doses of 1 g intravenously every 6 h to 31 patients. Twenty-five patients, with 27 infections, were clinically evaluable and received 20 to 210 g of imipenem for a duration of 5 to 56 days (average 16.3 days). Infections included seven cases of osteomyelitis, seven of bacteremia, five of cellulitis, two of pneumonia, three of pelvic cellulitis, two of intraabdominal abscess, and one each of empyema, mediastinitis, and endometritis. Fifty-five percent of the infections were caused by gram-negative bacilli, 33% were due to gram-positive organisms, and 10% were caused by anaerobes. Twenty-two patients (81%) were cured, three improved, one relapsed, and one became superinfected with a resistant organism. In 5 of 11 cases with Pseudomonas aeruginosa, the imipenem MIC for organisms isolated by the end of treatment was higher than it was initially, raising concern that imipenem should not be used alone to treat Pseudomonas aeruginosa infections. Twenty-one patients had no adverse reaction; of the remaining 10 patients, 4 had nausea, 1 had urticaria, and 6 had mild abnormalities in hepatic function; three episodes of diarrhea included two with Clostridium difficile toxin in stool and one with pseudomembranous colitis, as determined by sigmoidoscopy. Levels of creatinine, hemoglobin, leukocytes, platelets, prothrombin, and urine components were unchanged. Imipenem-cilastatin is a clinically effective antibiotic with freedom from nephrotoxicity and hematological abnormalities in the large doses used in this study.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bartlett J. G. Antimicrobial agents implicated in Clostridium difficile toxin-associated diarrhea of colitis. Johns Hopkins Med J. 1981 Jul;149(1):6–9. [PubMed] [Google Scholar]
- Bauer A. W., Kirby W. M., Sherris J. C., Turck M. Antibiotic susceptibility testing by a standardized single disk method. Am J Clin Pathol. 1966 Apr;45(4):493–496. [PubMed] [Google Scholar]
- Baumgartner J. D., Glauser M. P. Comparative study of imipenem in severe infections. J Antimicrob Chemother. 1983 Dec;12 (Suppl 500):141–148. doi: 10.1093/jac/12.suppl_d.141. [DOI] [PubMed] [Google Scholar]
- Drusano G. L., Schimpff S. C., Hewitt W. L. The acylampicillins: mezlocillin, piperacillin, and azlocillin. Rev Infect Dis. 1984 Jan-Feb;6(1):13–32. doi: 10.1093/clinids/6.1.13. [DOI] [PubMed] [Google Scholar]
- Drusano G. L., Standiford H. C., Bustamante C., Forrest A., Rivera G., Leslie J., Tatem B., Delaportas D., MacGregor R. R., Schimpff S. C. Multiple-dose pharmacokinetics of imipenem-cilastatin. Antimicrob Agents Chemother. 1984 Nov;26(5):715–721. doi: 10.1128/aac.26.5.715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eron L. J., Hixon D. L., Park C. H., Goldenberg R. I., Poretz D. M. Imipenem versus moxalactam in the treatment of serious infections. Antimicrob Agents Chemother. 1983 Dec;24(6):841–846. doi: 10.1128/aac.24.6.841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahan J. S., Kahan F. M., Goegelman R., Currie S. A., Jackson M., Stapley E. O., Miller T. W., Miller A. K., Hendlin D., Mochales S. Thienamycin, a new beta-lactam antibiotic. I. Discovery, taxonomy, isolation and physical properties. J Antibiot (Tokyo) 1979 Jan;32(1):1–12. doi: 10.7164/antibiotics.32.1. [DOI] [PubMed] [Google Scholar]
- Kropp H., Sundelof J. G., Hajdu R., Kahan F. M. Metabolism of thienamycin and related carbapenem antibiotics by the renal dipeptidase, dehydropeptidase. Antimicrob Agents Chemother. 1982 Jul;22(1):62–70. doi: 10.1128/aac.22.1.62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kropp H., Sundelof J. G., Kahan J. S., Kahan F. M., Birnbaum J. MK0787 (N-formimidoyl thienamycin): evaluation of in vitro and in vivo activities. Antimicrob Agents Chemother. 1980 Jun;17(6):993–1000. doi: 10.1128/aac.17.6.993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marier R. L., McCloskey R. V., Dickenson G., Sanders C. V., Aldridge K. E., Hoffman T., Gutterman D., Janney A. Comparative clinical trial of imipenem-cilastatin (N-formimidoyl-thienamycin-dehydropeptidase inhibitor) and cefazolin. J Antimicrob Chemother. 1983 Dec;12 (Suppl 500):133–139. doi: 10.1093/jac/12.suppl_d.133. [DOI] [PubMed] [Google Scholar]
- Neu H. C., Labthavikul P. Comparative in vitro activity of N-formimidoyl thienamycin against gram-positive and gram-negative aerobic and anaerobic species and its beta-lactamase stability. Antimicrob Agents Chemother. 1982 Jan;21(1):180–187. doi: 10.1128/aac.21.1.180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norrby S. R., Alestig K., Björnegård B., Burman L. A., Ferber F., Huber J. L., Jones K. H., Kahan F. M., Kahan J. S., Kropp H. Urinary recovery of N-formimidoyl thienamycin (MK0787) as affected by coadministration of N-formimidoyl thienamycin dehydropeptidase inhibitors. Antimicrob Agents Chemother. 1983 Feb;23(2):300–307. doi: 10.1128/aac.23.2.300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norrby S. R., Björnegård B., Ferber F., Jones K. H. Pharmacokinetics of imipenem in healthy volunteers. J Antimicrob Chemother. 1983 Dec;12 (Suppl 500):109–124. doi: 10.1093/jac/12.suppl_d.109. [DOI] [PubMed] [Google Scholar]
- RIchmond M. H. The semi-synthetic thienamycin derivative MK0787 and its properties with respect to a range of beta-lactamases from clinically relevant bacterial species. J Antimicrob Chemother. 1981 Mar;7(3):279–285. doi: 10.1093/jac/7.3.279. [DOI] [PubMed] [Google Scholar]
- Romagnoli M. F., Fu K. P., Neu H. C. The antibacterial activity of thienamycin against multiresistant bacteria-comparison with beta-lactamase stable compounds. J Antimicrob Chemother. 1980 Sep;6(5):601–606. doi: 10.1093/jac/6.5.601. [DOI] [PubMed] [Google Scholar]
- Smith C. R. Cefotaxime and cephalosporins: adverse reactions in perspective. Rev Infect Dis. 1982 Sep-Oct;4 (Suppl):S481–S488. doi: 10.1093/clinids/4.supplement_2.s481. [DOI] [PubMed] [Google Scholar]
- Tally F. P., Jacobus N. V., Gorbach S. L. In vitro activity of N-formimidoyl thienamycin (MK0787). Antimicrob Agents Chemother. 1980 Oct;18(4):642–644. doi: 10.1128/aac.18.4.642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winston D. J., McGrattan M. A., Busuttil R. W. Imipenem therapy of Pseudomonas aeruginosa and other serious bacterial infections. Antimicrob Agents Chemother. 1984 Nov;26(5):673–677. doi: 10.1128/aac.26.5.673. [DOI] [PMC free article] [PubMed] [Google Scholar]


