Abstract
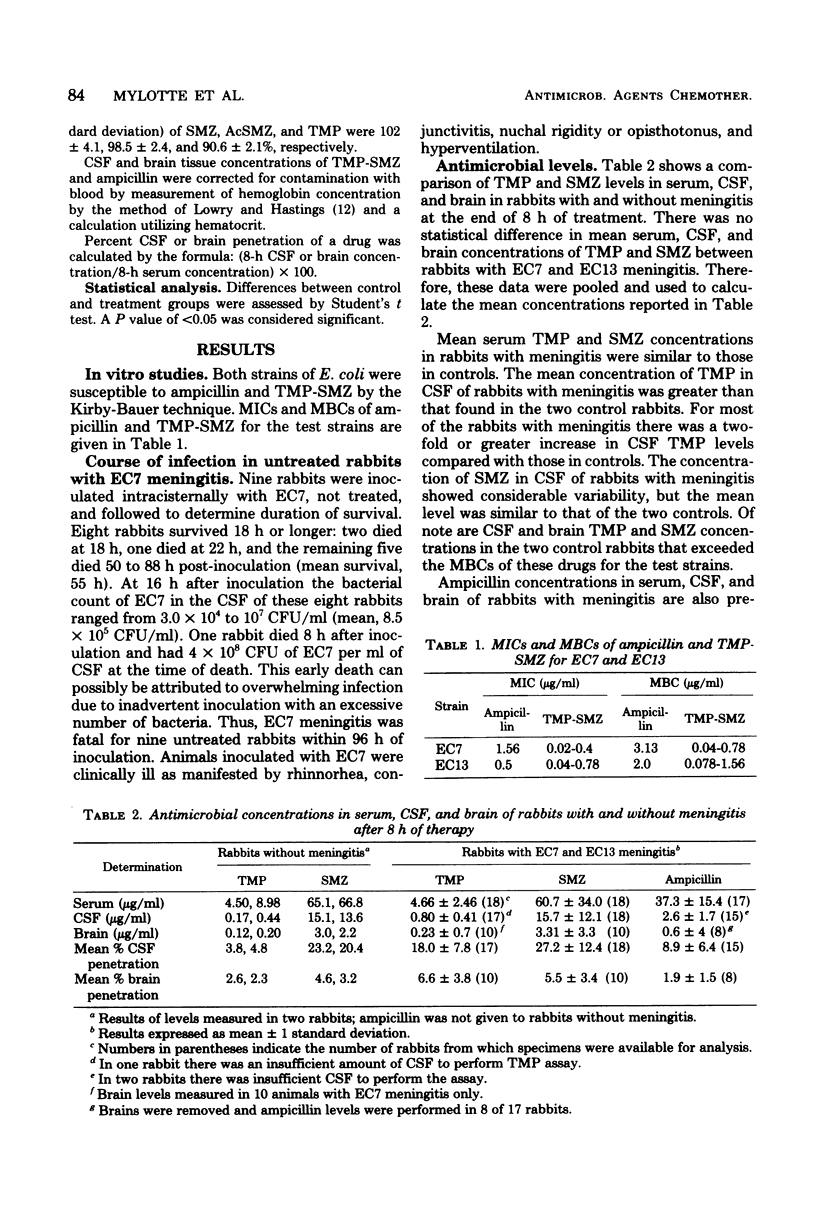
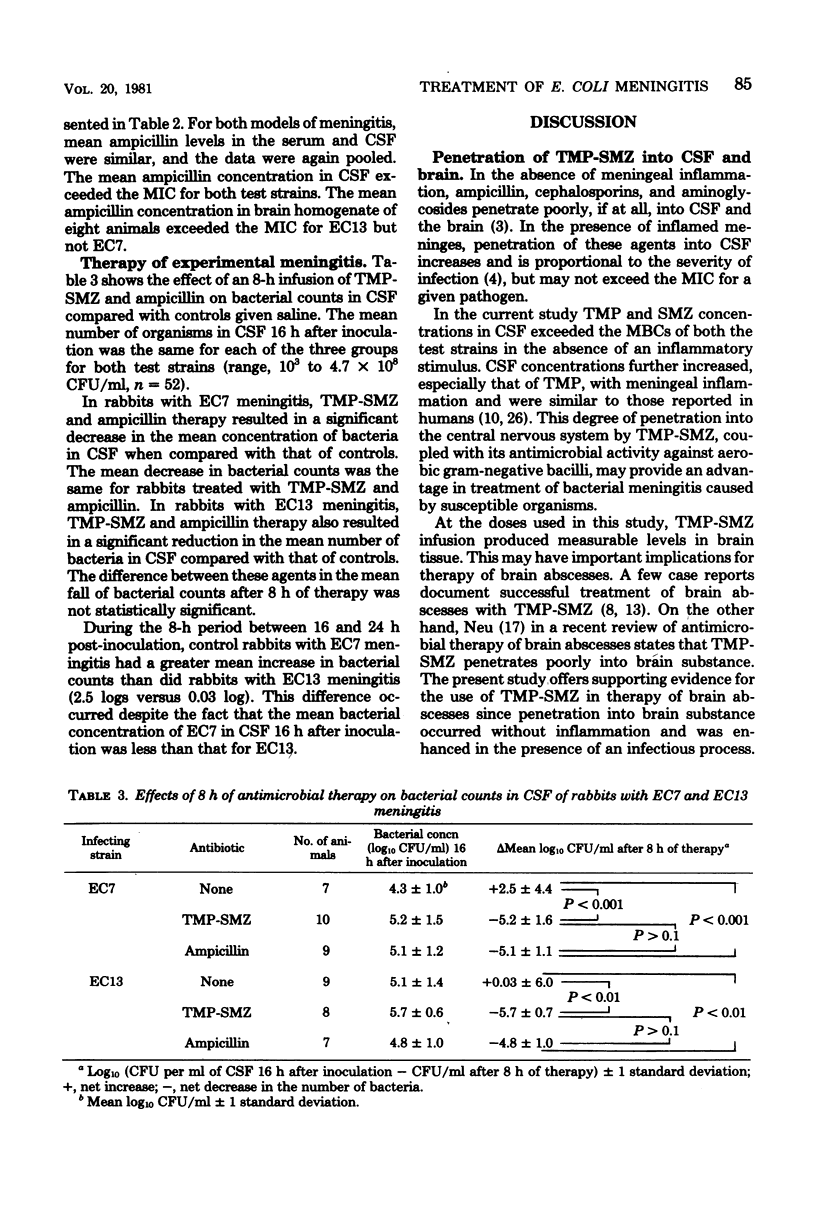
We used two strains of ampicillin-susceptible Escherichia coli to produce meningitis in rabbits and utilized these models (i) to compare the killing effects of parenteral trimethoprim-sulfamethoxazole (TMP-SMZ) and ampicillin on E. coli in cerebrospinal fluid after 8 h of treatment and (ii) to measure the penetration of TMP-SMZ and ampicillin into cerebrospinal fluid and the brain. At 16 h after intracisternal inoculation with a test strain, rabbits were treated with TMP (6 mg/kg per h) and SMZ (30 mg/kg per h), ampicillin (40 mg/kg per h), or saline intravenously for 8 h. TMP-SMZ levels were measured by high-pressure liquid chromatography, and ampicillin levels were measured by microbiological assay. Mean +/- standard deviation concentrations of TMP, SMZ, and ampicillin in cerebrospinal fluid (mean percent penetration) at the completion of 8 h of therapy were 0.80 +/- 0.41 (18%), 15.7 +/- 21.1 (27.2%), and 2.6 +/- 1.7 (8.9%) microgram/ml, respectively. TMP, SMZ, and ampicillin levels in brain homogenate after 8 h of therapy were 0.23 +/- 0.07 (6.6%), 3.31 +/- 3.3 (5.5%), and 0.6 +/- 4.53 (1.9%) microgram/g, respectively. TMP-SMZ infusion for 8 h produced a significant reduction in mean bacterial counts in cerebrospinal fluid in both models of meningitis compared with saline controls. The decrease in mean bacterial counts with TMP-SMZ therapy was equivalent to that produced by ampicillin.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Beam T. R., Jr, Allen J. C. Blood, brain, and cerebrospinal fluid concentrations of several antibiotics in rabbits with intact and inflamed meninges. Antimicrob Agents Chemother. 1977 Dec;12(6):710–716. doi: 10.1128/aac.12.6.710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beam T. R., Jr, Allen J. C. Comparison of cefamandole, cephalothin, ampicillin, and chloramphenicol in experimental Escherichia coli meningitis. Antimicrob Agents Chemother. 1980 Jan;17(1):37–42. doi: 10.1128/aac.17.1.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farid Z., Girgis N. I., Yassin W. Letter: Trimethoprim-sulfamethoxazole and bacterial meningitis. Ann Intern Med. 1976 Jan;84(1):50–51. doi: 10.7326/0003-4819-84-1-50. [DOI] [PubMed] [Google Scholar]
- Greene B. M., Thomas F. E., Jr, Alford R. H. Letter: Trimethoprim-sulfamethoxazole and brain abscess. Ann Intern Med. 1975 Jun;82(6):812–813. doi: 10.7326/0003-4819-82-6-812. [DOI] [PubMed] [Google Scholar]
- Grose W. E., Bodey G. P., Loo T. L. Clinical pharmacology of intravenously administered trimethoprim-sulfamethoxazole. Antimicrob Agents Chemother. 1979 Mar;15(3):447–451. doi: 10.1128/aac.15.3.447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirwan W. O. Cerebrospinal fluid cotrimoxazole levels. J Ir Med Assoc. 1974 Feb 9;67(3):76–77. [PubMed] [Google Scholar]
- Kramer P. W., Griffith R. S., Campbell R. L. Antibiotic penetration of the brain. A comparative study. J Neurosurg. 1969 Sep;31(3):295–302. doi: 10.3171/jns.1969.31.3.0295. [DOI] [PubMed] [Google Scholar]
- Maderazo E. G., Quintiliani R. Treatment of nocardial infection with trimethoprim and sulfamethoxazole. Am J Med. 1974 Oct;57(4):671–675. doi: 10.1016/0002-9343(74)90022-9. [DOI] [PubMed] [Google Scholar]
- McCracken G. H., Jr, Mize S. G., Threlkeld N. Intraventricular gentamicin therapy in gram-negative bacillary meningitis of infancy. Report of the Second Neonatal Meningitis Cooperative Study Group. Lancet. 1980 Apr 12;1(8172):787–791. [PubMed] [Google Scholar]
- McCracken G. H., Jr The rate of bacteriologic response to antimicrobial therapy in neonatal meningitis. Am J Dis Child. 1972 Jun;123(6):547–553. doi: 10.1001/archpedi.1972.02110120071004. [DOI] [PubMed] [Google Scholar]
- Morzaria R. N., Walton I. G., Pickering D. Neonatal meningitis treated with trimethoprim and sulphamethoxazole. Br Med J. 1969 May 24;2(5655):511–512. doi: 10.1136/bmj.2.5655.511-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- PLORDE J. J., GARCIA M., PETERSDORF R. G. STUDIES ON THE PATHOGENESIS OF MENINGITIS. IV. PENICILLIN LEVELS IN THE CEREBROSPINAL FLUID IN EXPERIMENTAL MENINGITIS. J Lab Clin Med. 1964 Dec;64:960–969. [PubMed] [Google Scholar]
- Pelton S. I., Shurin P. A., Klein J. O., Finland M. Quantitative inhibition of Haemophilus influenzae by trimethoprim/sulfamethoxazole. Antimicrob Agents Chemother. 1977 Dec;12(6):649–654. doi: 10.1128/aac.12.6.649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perfect J. R., Lang S. D., Durack D. T. Comparison of cotrimoxazole, ampicillin, and chloramphenicol in treatment of experimental Haemophilus influenzae type B meningitis. Antimicrob Agents Chemother. 1980 Jan;17(1):43–48. doi: 10.1128/aac.17.1.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roy L. P. Sulphamethoxazole-trimethoprim in infancy. Med J Aust. 1971 Jan 16;1(3):148–150. doi: 10.5694/j.1326-5377.1971.tb87481.x. [DOI] [PubMed] [Google Scholar]
- Sabel K. G., Brandberg A. Treatment of meningitis and septicemia in infancy with a sulphamethoxazole/trimethorpim combination. Acta Paediatr Scand. 1975 Jan;64(1):25–32. doi: 10.1111/j.1651-2227.1975.tb04376.x. [DOI] [PubMed] [Google Scholar]
- Sheretz R. J., Dacey R., Sande M. A. Cefamandole in the therapy of experimental pneumococcal meningitis. J Antimicrob Chemother. 1976 Jun;2(2):159–165. doi: 10.1093/jac/2.2.159. [DOI] [PubMed] [Google Scholar]
- Strausbaugh L. J., Mandaleris C. D., Sande M. A. Cefamandole and ampicillin therapy in experimental Haemophilus influenzae meningitis. J Infect Dis. 1977 Feb;135(2):210–216. doi: 10.1093/infdis/135.2.210. [DOI] [PubMed] [Google Scholar]
- Svedhem A., Iwarson S. Cerebrospinal fluid concentrations of trimethoprim during oral and parenteral treatment. J Antimicrob Chemother. 1979 Nov;5(6):717–720. doi: 10.1093/jac/5.6.717. [DOI] [PubMed] [Google Scholar]
- Wilfert C. M. E. coli meningitis: K1 antigen and virulence. Annu Rev Med. 1978;29:129–136. doi: 10.1146/annurev.me.29.020178.001021. [DOI] [PubMed] [Google Scholar]


