Abstract
Francisella tularensis replicates in macrophages and dendritic cells, but interactions with other cell types have not been well described. F. tularensis LVS invaded and replicated within alveolar epithelial cell lines. Following intranasal inoculation of C57BL/6 mice, Francisella localized to the alveolus and replicated within alveolar type II epithelial cells.
Francisella tularensis, the etiological agent of tularemia, is a zoonotic pathogen with a broad host range, spanning from protists to humans. The organism is transmitted to humans through handling of contaminated material, insect bites, or inhalation (6, 10). It has been determined that contact with 25 or fewer bacteria is sufficient to cause disease (16, 17). Following contact, the bacteria disseminate to the liver, spleen, and lungs regardless of the initial transmission route (7, 10).
The low infectious dose, myriad of transmission routes, broad host range, and severity of disease caused by F. tularensis led a number of nations to develop and stockpile this organism as a biological weapon (9), yet little is known about the basis of its pathogenesis or virulence. It has been reported that macrophages and, potentially, dendritic cells serve as the primary host cells for growth of Francisella in humans and other animals (5, 18). This conclusion is supported by the observations that F. tularensis and other closely related Francisella species survive and replicate in human and rodent macrophages (1, 4) and that many of the identified attenuating mutations impair intramacrophage growth (2, 11, 12, 14, 15).
Clearly, intramacrophage survival is an important virulence property of Francisella. However, apart from one report of hepatocyte association in infected liver (8), the potential contribution of other host cell interactions to F. tularensis virulence and pathogenesis remains untested. Given the severity of tularemia acquired by inhalation, we sought to address this possibility by using in vitro and in vivo models to examine whether Francisella invades and replicates within epithelial cells of the lung.
Francisella tularensis LVS invades and replicates within lung epithelial cells in vitro.
To determine whether Francisella could invade and replicate within lung epithelial cells, in vitro invasion and replication assays were performed using the human alveolar type II (ATII) epithelial cell-derived cell line A549 (ATCC), the mouse ATII cell-derived cell line MLE-12 (ATCC), and the mouse lung epithelial cell-derived cell line Tc-1 (ATCC). For comparison, the mouse macrophage-like cell line J774A.1 (ATCC) was also used. Intracellular bacteria were enumerated by a gentamicin protection assay. The cell lines were grown to confluence in 24-well plates and inoculated with F. tularensis LVS at a multiplicity of infection of 100:1. Four hours after inoculation, the cells were washed with phosphate-buffered saline (PBS), and medium containing gentamicin (25 μg/ml) was added to kill extracellular bacteria.
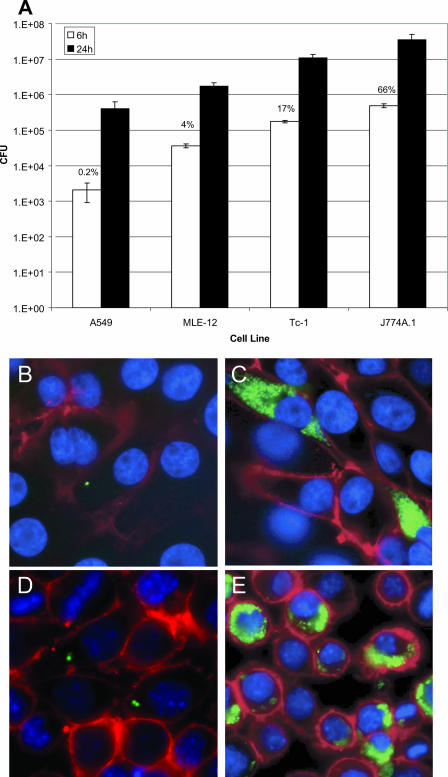
Intracellular organisms were recovered from all cell lines 6 and 24 h postinoculation (Fig. 1A). The number of intracellular organisms recovered 6 h postinoculation and the percentage of infected cells varied among the lung epithelial cell lines, with the fewest intracellular Francisella organisms recovered from the human ATII cell line, A549. The percentage of infected epithelial cells ranged from 0.2% of A549 cells to 17% of Tc-1 cells (Fig. 1A). The number of intracellular bacteria recovered from each lung epithelial cell line at 6 h was smaller than the number recovered from J774A.1 cells, as was the percentage of infected cells, indicating that entry into epithelial cells may be a less efficient process than uptake by macrophages.
FIG. 1.
F. tularensis LVS invades and replicates within ATII cell lines in vitro. (A) Intracellular bacteria recovered from A549, MLE-12, Tc-1, and J774A.1 cells 6 and 24 h postinoculation. The percentages above the bars represent percentages of infected cells. (B and C) Fluorescence imaging of A549 cells inoculated with GFP-expressing LVS 6 h (B) and 24 h (C) following inoculation. Cell borders were visualized by rhodamine-phalloidin (Molecular Probes) staining (red), and nuclei were visualized with 4′,6′-diamidino-2-phenylindole (DAPI; blue). (D and E) Fluorescence imaging of J774A.1 cells inoculated with GFP-expressing LVS (green) 6 h (D) and 24 h (E) postinoculation. Cell borders were visualized using biotinylated lectin from Lens culinaris and streptavidin-conjugated Alexa Fluor 647 (Molecular Probes) (red), and nuclei were stained with DAPI (blue). Intracellular replication experiments were carried out in triplicate; error bars represent standard deviations of the means.
The number of intracellular bacteria increased by an average of 100-fold during the following 18 h in each cell line, representing an intracellular doubling time of roughly 3 h (Fig. 1A). Intracellular localization and proliferation were confirmed using fluorescence microscopy and digital image deconvolution (Fig. 1B to E). From 6 to 24 h postinoculation, the relative increase of intracellular bacteria within lung epithelial cells was similar to that observed within J774A.1 cells, indicating that F. tularensis LVS replicated to the same degree within lung epithelial cells as in macrophages.
There are many reports of Francisella replicating within macrophages in vitro, and here we report its ability to replicate within cultured lung epithelial cells. Whereas some work has been done to examine localization of Francisella in the liver (8), little is known about the localization of inhaled Francisella in the lung. Bosio and Dow recently reported that Francisella was associated primarily with dendritic cells isolated from bronchioalveolar lavage fluid of mice 1 hour after inhalation (5). However, the localization of bacteria in lung tissue throughout the course of infection has not been addressed.
Following inhalation, Francisella localizes to the alveolus.
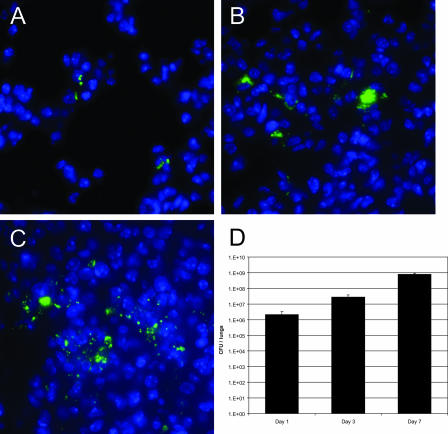
To determine the localization of Francisella in the airway following inhalation, anesthetized 6- to 8-week-old female C57BL/6 mice were inoculated intranasally with 105 CFU of F. tularensis LVS expressing green fluorescent protein (GFP) suspended in 50 μl of PBS. (All mouse work was performed according to IACUC-approved protocol.) Immunofluorescence analysis was performed on formalin-fixed and paraffin-embedded tissue sections obtained from nasal turbinates, trachea, and lungs harvested 1, 3, and 7 days postinoculation. No bacteria were observed in turbinates or trachea. In the lung, few bacteria associated with the apical surface of bronchial epithelial cells, while the majority colocalized with alveolar cells (Fig. 2). Fluorescence imaging of sequential vertical planes revealed that most infected alveolar cells contained multiple bacteria throughout the cytoplasm, indicative of intracellular replication (data not shown). Bacterial replication within ciliated or nonciliated (Clara) bronchial epithelial cells was not observed. The absolute number of bacteria (Fig. 2D) and the number of infected alveolar cells increased by day 3 (Fig. 2B). By day 7, F. tularensis within the lung was widespread but remained exclusively in the alveolus (Fig. 2C). Throughout the course of infection, the amount of extracellular space observed in the network of alveolar cells decreased, causing the alveolar cells to appear more condensed (Fig. 2).
FIG. 2.
F. tularensis localizes to the alveolus following inhalation. Mice were intranasally inoculated with 105 CFU of F. tularensis LVS expressing GFP. One, three, and seven days postinoculation, lungs were harvested and prepared for immunofluorescence analysis. (A to C) Bacterial localization was determined by probing lung sections with a fluorescently labeled antibody to GFP (green). Nuclei were stained with DAPI (blue) to visualize lung cells. Representative images of the alveoli of infected mice 1 (A), 3 (B), and 7 (C) days postinoculation. (D) Bacterial recovery from lungs 1, 3, and 7 days following intranasal inoculation with 105 CFU LVS. Each bar represents mean recovery from three mice; error bars represent standard deviations of the means.
Inhaled Francisella colocalizes to and replicates within ATII cells in vivo.
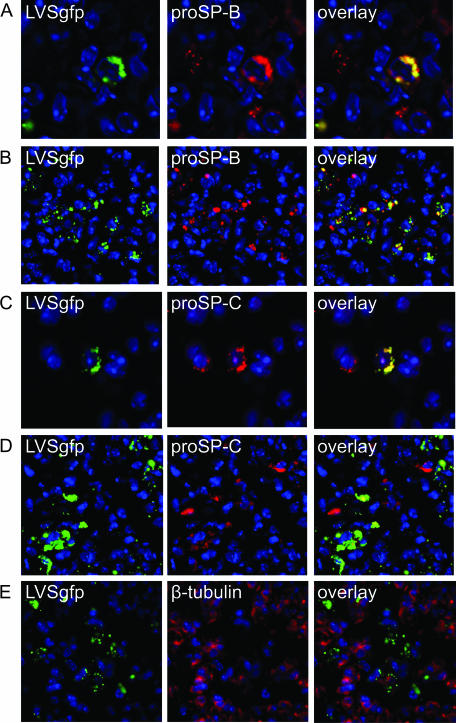
Given that Francisella invaded and replicated within ATII-derived cell lines in vitro, we probed infected lung tissue sections with antibodies to the nonsecreted surfactant protein precursors proSP-B and proSB-C (Chemicon) to determine whether Francisella localized to and replicated within ATII cells in vivo following inhalation. proSP-B is produced by ATII cells and nonciliated bronchiolar Clara cells (13), whereas proSP-C is produced by ATII cells exclusively (3). Three days following inoculation, the majority of alveolar cells associated with F. tularensis also bound antibodies to the nonsecreted surfactant protein precursors proSP-B and proSB-C (Fig. 3A to D). Some cells associated with bacteria were not positive for proSP-B or proSP-C, indicating that Francisella interacts with other cell types in the lung following inhalation.
FIG. 3.
Following inhalation, F. tularensis LVS expressing GFP colocalized with proSP-B and proSP-C, proteins produced by ATII epithelial cells. Bacterial localization was determined with a fluorescently labeled antibody to GFP (green). Nuclei were stained with DAPI (blue). Sections were probed with fluorescently labeled antibody to proSP-B (red) (A and B), proSP-C (red) (C and D) to identify ATII cells and β-tubulin (red) (E). Representative images are from lung sections 3 days postinoculation.
In addition to the colocalization with proSP proteins, microscopy of sequential vertical planes confirmed that bacteria were inside infected ATII cells (data not shown). Rabbit antibody specific for β-tubulin (Abcam) did not colocalize with F. tularensis (Fig. 3E), indicating that the colocalization of Francisella with rabbit proSP antibodies was not due to bacteria nonspecifically binding rabbit antibodies, nor did the proSP antibodies cross-react with cultured Francisella organisms (data not shown). These collective data demonstrate that F. tularensis replicates within ATII cells following inhalation and the proportion of ATII cells harboring bacteria increases during the course of pneumonic tularemia.
Bacteria were also observed in probed sections that did not colocalize with proSP-B and proSP-C (Fig. 3), indicating that ATII cells are not the only alveolar cell type harboring replicating Francisella. Macrophages and dendritic cells have been reported as potential host cells for replicating Francisella organisms (1, 4, 5). Due to difficulties in staining for surface macrophage and dendritic cell markers in embedded lung sections, we utilized dispase digestion of infected mouse lungs to stain for surface markers and also to assess our results from the embedded tissue staining.
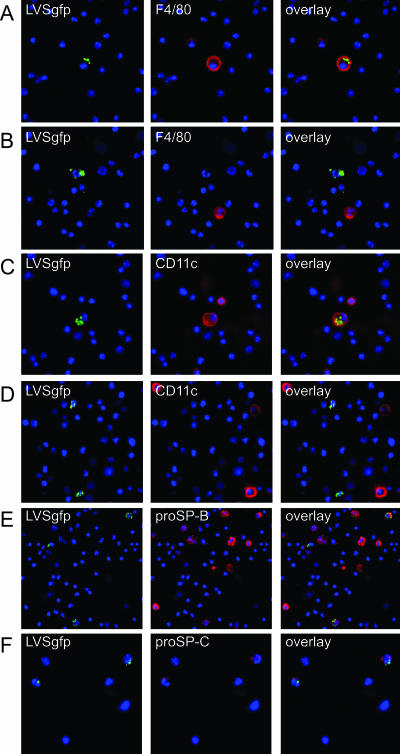
Three days after inoculation with LVS expressing GFP, lungs were infused and incubated with the neutral protease dispase (BD Biosciences). Digested tissue was washed in PBS and subsequently filtered through 40- and 20-μm-pore-size mesh. Staining with fluorescently labeled antibody specific for the surface markers F4/80 (eBioscience) and CD11c (eBioscience) was performed prior to fixation with 4% paraformaldehyde. Staining for the intracellular markers proSP-B and proSP-C occurred following fixation and required the use of Cytoperm (BD Biosciences) to permeabilize the cells. F. tularensis LVS was observed within cells expressing F4/80, CD11c, proSP-B, and proSP-C (Fig. 4), indicating that following inhalation, bacteria survive and replicate within macrophages, dendritic cells, and ATII cells.
FIG. 4.
F. tularensis LVS expressing GFP colocalized with cells expressing the macrophage marker F4/80, the dendritic cell marker CD11c, and the ATII cell markers proSP-B and proSP-C. Nuclei were stained with DAPI (blue). Mouse lung cells were probed with fluorescently labeled antibody to F4/80 (red) (A and B), CD11c (red) (C and D), proSP-B (red) (E), and proSP-C (red) (F). Representative images are from lung cells 3 days postinoculation.
Here we report that in addition to replicating within macrophages and dendritic cells, F. tularensis invades and replicates within alveolar type II epithelial cells, indicating that interaction with these cells following inhalation may be an important component of pneumonic tularemia. Future work will analyze the proportion of various cell types that are infected in the lung as well as attempt to identify the contribution of ATII cell invasion and replication to the disease progression of pneumonic tularemia.
Acknowledgments
We gratefully acknowledge the technical support and invaluable contributions of Yan Zhao and Kimberly Burns and thank Mats Forsman for sending us the pKK214GFP plasmid prepublication. We also thank Jo Rae Wright for sharing her expertise on lung biology and Robert Fulcher for editing assistance and general advisement.
This work was supported by a Southeast Regional Center of Excellence in Biodefense and Emerging Infections grant (NIH/NIAID U54-AI057157) and by the National Institutes of Health (R21-AI053399).
Editor: D. L. Burns
Footnotes
Published ahead of print on 6 November 2006.
REFERENCES
- 1.Anthony, L. D., R. D. Burke, and F. E. Nano. 1991. Growth of Francisella spp. in rodent macrophages. Infect. Immun. 59:3291-3296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Baron, G. S., and F. E. Nano. 1998. MglA and MglB are required for the intramacrophage growth of Francisella novicida. Mol. Microbiol. 29:247-259. [DOI] [PubMed] [Google Scholar]
- 3.Beers, M. F., and S. Mulugeta. 2005. Surfactant protein C biosynthesis and its emerging role in conformational lung disease. Annu. Rev. Physiol. 67:663-696. [DOI] [PubMed] [Google Scholar]
- 4.Bolger, C. E., C. A. Forestal, J. K. Italo, J. L. Benach, and M. B. Furie. 2005. The live vaccine strain of Francisella tularensis replicates in human and murine macrophages but induces only the human cells to secrete proinflammatory cytokines. J. Leukoc. Biol. 77:893-897. [DOI] [PubMed] [Google Scholar]
- 5.Bosio, C. M., and S. W. Dow. 2005. Francisella tularensis induces aberrant activation of pulmonary dendritic cells. J. Immunol. 175:6792-6801. [DOI] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention. 2005. Tularemia transmitted by insect bites—Wyoming, 2001-2003. Morb. Mortal. Wkly. Rep. 54:170-173. [PubMed] [Google Scholar]
- 7.Conlan, J. W., W. Chen, H. Shen, A. Webb, and R. KuoLee. 2003. Experimental tularemia in mice challenged by aerosol or intradermally with virulent strains of Francisella tularensis: bacteriologic and histopathologic studies. Microb. Pathog. 34:239-248. [DOI] [PubMed] [Google Scholar]
- 8.Conlan, J. W., and R. J. North. 1992. Early pathogenesis of infection in the liver with the facultative intracellular bacteria Listeria monocytogenes, Francisella tularensis, and Salmonella typhimurium involves lysis of infected hepatocytes by leukocytes. Infect. Immun. 60:5164-5171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dennis, D. T., T. V. Inglesby, D. A. Henderson, J. G. Bartlett, M. S. Ascher, E. Eitzen, A. D. Fine, A. M. Friedlander, J. Hauer, M. Layton, S. R. Lillibridge, J. E. McDade, M. T. Osterholm, T. O'Toole, G. Parker, T. M. Perl, P. K. Russell, and K. Tonat. 2001. Tularemia as a biological weapon: medical and public health management. JAMA 285:2763-2773. [DOI] [PubMed] [Google Scholar]
- 10.Ellis, J., P. C. Oyston, M. Green, and R. W. Titball. 2002. Tularemia. Clin. Microbiol. Rev. 15:631-646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Golovliov, I., A. Sjostedt, A. Mokrievich, and V. Pavlov. 2003. A method for allelic replacement in Francisella tularensis. FEMS Microbiol. Lett. 222:273-280. [DOI] [PubMed] [Google Scholar]
- 12.Gray, C. G., S. C. Cowley, K. K. Cheung, and F. E. Nano. 2002. The identification of five genetic loci of Francisella novicida associated with intracellular growth. FEMS Microbiol. Lett. 215:53-56. [DOI] [PubMed] [Google Scholar]
- 13.Guttentag, S. H., M. F. Beers, B. M. Bieler, and P. L. Ballard. 1998. Surfactant protein B processing in human fetal lung. Am. J. Physiol. 275:L559-L566. [DOI] [PubMed] [Google Scholar]
- 14.Lauriano, C. M., J. R. Barker, F. E. Nano, B. P. Arulanandam, and K. E. Klose. 2003. Allelic exchange in Francisella tularensis using PCR products. FEMS Microbiol. Lett. 229:195-202. [DOI] [PubMed] [Google Scholar]
- 15.Lauriano, C. M., J. R. Barker, S. S. Yoon, F. E. Nano, B. P. Arulanandam, D. J. Hassett, and K. E. Klose. 2004. MglA regulates transcription of virulence factors necessary for Francisella tularensis intraamoebae and intramacrophage survival. Proc. Natl. Acad. Sci. USA 101:4246-4249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Saslaw, S., H. T. Eigelsbach, J. A. Prior, H. E. Wilson, and S. Carhart. 1961. Tularemia vaccine study. II. Respiratory challenge. Arch. Intern. Med. 107:702-714. [DOI] [PubMed] [Google Scholar]
- 17.Saslaw, S., H. T. Eigelsbach, H. E. Wilson, J. A. Prior, and S. Carhart. 1961. Tularemia vaccine study. I. Intracutaneous challenge. Arch. Intern. Med. 107:689-701. [DOI] [PubMed] [Google Scholar]
- 18.Titball, R. W., A. Johansson, and M. Forsman. 2003. Will the enigma of Francisella tularensis virulence soon be solved? Trends Microbiol. 11:118-123. [DOI] [PubMed] [Google Scholar]