Abstract
We have synthesized a new benzomorphan derivative, 2R-[2α,3(S*),6α]-1,2,3,4,5,6-hexahydro-6,11,11-trimethyl-3-[2-(phenylmethoxy)propyl]-2,6-methano-3-benzazocin-10-ol hydrochloride (BIII 890 CL), which displaced [3H]batrachotoxinin A-20α-benzoate from neurotoxin receptor site 2 of the Na+ channel in rat brain synaptosomes (IC50 = 49 nM), but exhibited only low affinity for 65 other receptors and ion channels. BIII 890 CL inhibited Na+ channels in cells transfected with type IIA Na+ channel α subunits and shifted steady-state inactivation curves to more negative potentials. The IC50 value for the inactivated Na+ channel was much lower (77 nM) than for Na+ channels in the resting state (18 μM). Point mutations F1764A and Y1771A in transmembrane segment S6 in domain IV of the α subunit reduced the voltage- and frequency-dependent block, findings which suggest that BIII 890 CL binds to the local anesthetic receptor site in the pore. BIII 890 CL inhibited veratridine-induced glutamate release in brain slices, as well as glutamate release and neurotoxicity in cultured cortical neurons. BIII 890 CL (3–30 mg/kg s.c.) reduced lesion size in mice and rats when administered 5 min after permanent focal cerebral ischemia at doses that did not impair motor coordination. In contrast to many other agents, BIII 890 CL was neuroprotective in both cortical and subcortical regions of the rat brain. Our results demonstrate that BIII 890 CL is a potent, selective, and highly use-dependent Na+ channel blocker that protects brain tissue from the deleterious effects of focal cerebral ischemia in rodents.
Cerebrovascular disease is a major cause of death and disability (1) because neurons and glia die as the brain is deprived of a continuous supply of oxygenated blood. Brain cells do not simply die of loss of energy. Stroke triggers a vicious cycle of electrical and chemical events, including ischemic depolarization, release of glutamate, and changes in calcium homeostasis (2). Current neuroprotective strategies concentrate on interfering with one or more of these processes. Initially, glutamate receptor antagonists promised new therapeutic potential (3) because the N-methyl-d-aspartate (NMDA) receptor–channel complex was implicated in neuronal loss in animal models of cerebral ischemia (4, 5). However, several NMDA receptor antagonists have been unsuccessful in phase III clinical trails. They possess several drawbacks. For instance, they cause changes in blood pressure and impair motor coordination at therapeutic doses (6, 7). Consequently, many researchers have focused on alternative targets, such as voltage-gated Na+ channels (8).
Voltage-gated Na+ channels are thought to play a key role in excitotoxic damage. Na+ channel blockers inhibit neuronal depolarization, glutamate release, and Na+ influx, thereby reducing Ca2+ influx by means of Ca2+ channels, NMDA receptor channels, and reversal of the Na+/Ca2+ exchanger (9). Because these effects reduce neuronal damage, Na+ channel blockers could be useful for the treatment of thromboembolic stroke. Voltage-gated Na+ channels have three distinct functional states: resting, active, and inactivated. Blockers of neuronal Na+ channels, such as local anesthetics, preferentially bind to the open and inactivated states of the channel with high affinity and act in a frequency- and voltage-dependent manner (10, 11). These properties would be useful attributes for neuroprotective drugs because they would preferentially block Na+ channels in depolarized tissue without inhibiting normal physiological functions. However, the low affinity and weak voltage dependence of existing Na+ channel blockers are probably insufficient for adequate differentiation of therapeutic effects from side effects in cerebral ischemia.
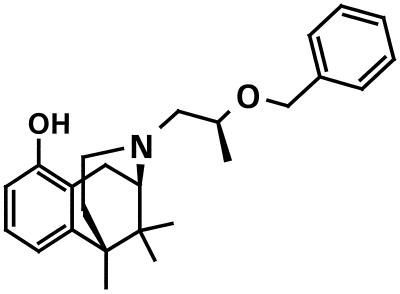
Several blockers of voltage-gated Na+ channels have been tested in clinical trials with mixed success. Lifarizine caused hypotension in patients (12), an observation which illustrates the poor specificity of this agent. Indeed, both lifarizine and lubeluzole block voltage-gated Ca2+ channels as well as Na+ channels (13, 14), and clinical trials with these agents have been discontinued (15). There is, therefore, considerable need for a specific, high-affinity blocker of voltage-gated Na+ channels to investigate the role of this channel in cerebral ischemia and to develop novel therapeutic approaches to stroke. Dextromethorphan is a benzomorphan derivative that noncompetitively blocks NMDA receptors as well as inhibiting voltage-dependent Na+ and Ca2+ channels in rat cortical neurons (16). Our group has previously shown that it is possible to synthesize a benzomorphan derivative that specifically blocks NMDA-induced currents through glutamate receptors (17, 18). We have now synthesized BIII 890 CL (Fig. 1), a benzomorphan derivative that is a potent, specific, and highly use-dependent blocker of voltage-dependent Na+ channels, and used it to investigate the role of such channels in cerebral ischemia.
Figure 1.
The chemical structure of BIII 890 CL
Materials and Methods
In Vitro Binding.
[3H]Batrachotoxinin-A-20-α-benzoate (BTX-b) with a specific activity of 54 Ci/mmol was purchased from DuPont/NEN. Specific [3H]BTX-b binding (19) was measured in synaptosomal preparations of rat cerebral cortex as previously described (20). All other binding experiments were performed in the laboratory of Cerep (Le Bois l'Évêque, France) and Panlabs (Bothell, WA) according to standard techniques.
Veratridine-Induced Glutamate Release in Brain Slices.
The assay was performed as previously described (20, 21). Crosschopped slices, 0.2 mm thick, from rat brain cortex or striatum of Wistar rats (Boehringer Ingelheim) were randomly distributed into microcentrifuge tubes (equivalent to about 430 μg of protein) and incubated for 15 min with or without veratridine (3 μM) from Research Biochemicals (Natick, MA) with an Eppendorf model 5437 Thermomixer. The test drug was present throughout the incubation period. The concentration of glutamate was measured by high-performance liquid chromatography and fluorescence detection after derivatization with o-phthalaldehyde as previously described (22). Protein was determined according to the Coomassie blue procedure (23).
Electrophysiological Experiments.
Investigations were performed by using tsA-201 cells transiently transfected with wild-type (WT) or mutant brain type II Na+ channel α subunits as previously described (24, 25). Cells were investigated in the “whole-cell” configuration of the patch-clamp technique. The extracellular solution contained (mM) 140 NaCl, 5 CsCl, 1.8 CaCl2, 1.0 MgCl2, 10 glucose, and 10 Hepes (pH 7.4 adjusted with NaOH). The intracellular solution contained 90 CsF, 50 CsCl, 10 CsEGTA, 10 NaF, 2 MgCl2, and 10 Hepes (pH adjusted with CsOH). Recording pipettes had resistances of 0.8–1.8 MΩ when filled with intracellular solution. Approximately 80% of series resistance was compensated. Residual linear leakage and capacitance were subtracted by using a P/4 protocol where appropriate. Data analysis and curve fitting were performed by using SigmaPlot from SPSS (Erkrath, Germany). Unless otherwise indicated, holding and test potentials were −100 and 0 mV for rbNaIIA WT and F1764A, and −120 and 0 mV for Y1771A. The following stimulation protocols were used: (i) Block of resting channels: The compound's effect was recorded with a single test pulse to 0 mV from the holding potential after appropriate preincubation (typically 3 min). (ii) Shift of steady-state inactivation curves: Prepulses of 1 s duration and various potentials were applied in the absence and presence of a given drug concentration. The data points were normalized and fitted by Boltzmann functions. (iii) Affinity for inactivated channels: Cells were depolarized to −40 mV for 5 s (which induced >95% inactivation), and a test pulse to 0 mV was applied after stepping back for 10 ms to the holding potential. This interval was long enough to remove most of the fast inactivation of unblocked channels, but short enough to prevent drug unbinding. The protocol was repeated until steady-state responses were obtained in the absence and presence of a given drug concentration. (iv) Stimulus-dependent block: Cells were stimulated with trains of 100 pulses (frequency: 5 Hz), and the currents were normalized to the amplitude of the first response. Grouped data are presented as means ± SEM of three to six cells for each experiment.
Neurotoxicity Experiments and Glutamate Analysis.
Confluent cultures of astrocytes were used to condition medium for the maintenance of cortical neurons. Astrocytes were prepared from newborn Wistar rats (P1–2) according to a previously described method (26). Cells from one cortex were cultured in a 75-cm2 flask with 20 ml DMEM/10% FCS from GIBCO in a humid atmosphere supplemented with 10% CO2. After 2 wk when the cell layer was confluent, the cells were shaken vigorously at 120 rpm overnight at 37°C in a Braun rotary shaker (Schöffengrund, Germany) to remove any residual neurons. The cells were then washed three times with PBS, and 30 ml of the B27/Neurobasal (27) medium from GIBCO was added and incubated at 37°C to allow the astrocytes to condition the medium. The astrocyte-conditioned medium was decanted, frozen in liquid N2 and stored at −80°C. Primaria 96-well plates (Falcon) were coated with poly-l-lysine (30 μg/cm2) and laminin (0.3 μg/cm2). Serum-free primary cultures of cortical neurons were prepared from embryonic Wistar rat (E18–19) brains according to previously described methods (26, 28). The neurons were counted and diluted, and an aliquot containing 50,000 cells in 60 μl B27/Neurobasal medium was added to each coated well. One day later, we added cytosine β-d-arabinofuranoside (5 μM) to inhibit proliferation of dividing nonneuronal cells. Cortical neurons were maintained 13–14 days in culture before performing the experiments. Neurons were treated with veratridine (10 μM) for 20 min, the compound was washed out, and the effects were quantified 24 h later. The cell viability was measured with a cell titer 96 kit from Promega, whereby a tetrazolium salt is converted by dehydrogenases of mitochondria of living cells into a blue derivative (29) that can be quantified at 570 nm by a plate reader. We added BIII 890 CL together with veratridine for 20 min and measured the number of living cells 24 h later. The concentration of glutamate in the cell culture medium was measured by high performance liquid chromatography as previously described (22). Peak identification was performed with external standards, and concentrations were calculated on the basis of peak height.
Middle Cerebral Artery (MCA) Occlusion in the Mouse.
The method employed was performed as previously described (17). Male mice (NMRI) from Iffa Credo weighing 20–30 g were anesthetized with isoflurane (2%) in room air. They were treated with BIII 890 CL at doses of 3, 10, and 30 mg/kg administered s.c. at 5 min and 3 h after occlusion. Control mice underwent occlusion of the MCA and received an equal volume of saline administered at the corresponding time points. The animals were carefully observed during recovery from anesthesia, and their body temperature was maintained at 37°C. The animals were sacrificed by injecting an overdose of tribromethanol (2.5%) 48 h after occlusion, the brains removed and stained by placing in an aqueous solution (1%) of 2,3,5-triphenyl-2H-tetrazolium chloride, and the cortical infarct areas measured with a video camera and Mocha image analysis software from Jandel Scientific (Erkrath, Germany).
MCA Occlusion in the Rat.
The method employed has been previously described (30). Male Fischer rats (F-344-ICO) from Iffa Credo weighing 209–301 g were anesthetized isoflurane (3% induction and 1% maintenance) in room air. They were treated with BIII 890 CL at doses of 3, 10, and 30 mg/kg administered s.c. at 5 min and 3 h after commencing ischemia. Control rats, which also underwent MCA occlusion, received an equal volume of saline at corresponding time points. The brains were fixed in 7.5% formalin, embedded, sliced, and stained with cresyl violet. The area of infarcted tissue for each slice was determined with a computer-based image analysis system from VIDAS (Zeiss, Germany), and the infarct volume was calculated.
Assessment of Motor Coordination by the Rotarod Method.
The ability of mice to maintain themselves on a horizontal, turning rod was used to assess whether BIII 890 CL affects motor coordination. The method and apparatus has been previously described (6). The apparatus consisted of a rod with a diameter of 2.5 cm that was suspended horizontally 50 cm above a plain working area. The rod was turned at a speed of 4 rev/min by an electric motor. Groups of five animals were placed on the turning rod 15 min after administration of 30 mg/kg s.c. BIII 890 CL, and the number of animals falling from the rod over a 3-min period was determined. All animals studies were conducted in accordance with German Animal Protection Laws (Tierschutzgesetz) and the principles expressed in the Declaration of Helsinki.
Results
Receptor Binding Studies.
Local anesthetics and related channel blockers are negative allosteric inhibitors of BTX-b binding (19). We initially determined the ability of BIII 890 CL to displace [3H]BTX-b from neurotoxin site 2 of voltage-gated Na+ channels in rat brain synaptosomal preparations. The IC50 of BIII 890 CL for this binding site was 49.1 ± 7.6 nM with a Hill coefficient of 1.34 ± 0.18 (n = 7). We also investigated whether BIII 890 CL displaced [3H]tetrodotoxin (TTX) from site 1 of the same channel and found no activity at concentrations up to 10,000 nM. We then studied the ability of BIII 890 CL to displace 65 other different radioligands from their respective binding sites in the central and peripheral nervous system. The results displayed in Table 1 demonstrate that BIII 890 CL is highly specific for displacement of radioligand from neurotoxin receptor site 2 of the Na+ channel and has little effect on many other receptors, including glutamate receptors and the dihydropyridine receptor of calcium channels.
Table 1.
BIII 890 CL binding to receptors
| Target | IC50, nM |
|---|---|
| BTX | 49 |
| TTX | >10,000 |
| NMDA (MK-801, glutamate, glycine), AMPA | >10,000 |
| Ca2+ dihydropyridine | >10,000 |
| Ca2+ (verapamil) | 2,680 |
| Ca2+ (diltiazem) | 719 |
| K+ channel (voltage dep., ATP sensit., Ca2+ dep.) | >10,000 |
| Cl− channel, GABAA, glycine | >10,000 |
| Adrenergic (α1, α2, β1, β2), dopaminergic (D1, D2, D3, D4) | >10,000 |
| Serotoninergic (5-HT1, 5-HT2, 5-HT3) | >10,000 |
| Adenosine (A1, A2), histamine (H1, H3) | >10,000 |
| Muscarinic (M1, M2, M3, M4), nicotinic (α4β2) | >10,000 |
| Cholecystokinin, thromboxane A2, LTB4, PAF | >10,000 |
| Endothelin, angiotensin, bradykinin, TRH | >10,000 |
| VIP, NK1, NPY2, insulin, galanin, phorbol ester | >10,000 |
| Glucocorticoid, estrogen, testosterone, progesterone | >10,000 |
| Opiate: delta | >10,000 |
| kappa | 1,000 |
| mu | 3,000 |
| Sigma (DTG, pentazocine) | 1,000 |
| EGF TK, calcineurin, calpain, NOS | >10,000 |
| MAOA, MAOB, PKCα, PKCβ | >100,000 |
BIII 890 CL Inhibits Voltage-Gated Sodium Channels.
A compound with such inhibitory effects on BTX-b binding is likely to be a modulator of voltage-gated Na+ channel function. We therefore performed electrophysiological experiments to characterize the effects of BIII 890 CL in more detail. BIII 890 CL reduced Na+ currents but had no effect on the kinetics of activation and inactivation (Fig. 2A, Inset) or on the voltage dependence of activation (not shown). Since BTX-b binding is inhibited by local anesthetics (24, 31), which preferentially block Na+ channels in their inactivated state, we investigated the effects of BIII 890 CL on the voltage dependence of inactivation. With 1-s prepulses, 1 μM and 10 μM of the compound shifted the midpoints of the steady-state inactivation curves by −5.8 ± 0.5 mV and −27.4 ± 5.0 mV, respectively (Fig. 2A), as expected if BIII 890 CL binds preferentially to Na+ channels in their inactivated state. To characterize the interaction of BIII 890 CL with inactivated sodium channels in more detail, we recorded Na+ currents following depolarizing prepulses that induced almost complete inactivation of the channels but did not activate them. These experiments yielded an IC50 value of 77 ± 12 nM (Hill coefficient, −1.29 ± 0.27; n = 6; Fig. 2B) for the blockade of inactivated channels in WT cells. The block of resting rIIA α subunits was investigated by holding the cell under study at a membrane potential of −100 mV. Under these conditions, BIII 890 CL inhibited membrane currents in response to a test pulse to 0 mV with an IC50 value of 18 ± 3.4 μM (Hill coefficient, −0.90 ± 0.13; n = 6; Fig. 2B). Thus, BIII 890 CL discriminates by a factor of 230 between block of resting and inactivated Na+ channels.
Figure 2.
Effects of BIII 890 CL on Na+ currents in cells expressing rbIIA channels. (A) BIII 890 CL-dependent shift in the voltage-dependence of NaIIA WT channel availability. Inactivation curves from a typical cell are shown in the absence or presence of 1 μM or 10 μM BIII 890 CL. Data were normalized to the most negative control value at each concentration and fitted by Boltzmann functions. (Inset) Typical current traces in response to depolarization to 0 mV following a prepulse of −70 mV with and without BIII 890 CL (10 μM). (B) Concentration-response curves for the blockade of WT and IVS6 mutants by BIII 890 CL. Resting WT channels were inhibited with an IC50 value of 18 μM, whereas the concentration for half-maximum block was only 77 nM for inactivated channels. Mutations of the IVS6 region F1764A and Y1771A reduced affinities of inactivated channels to 349 and 619 nM, respectively. (C) Typical example of stimulus-dependent block of NaIIA channels by BIII 890 CL. At a concentration of 1.85 μM, BIII 890 CL induced pronounced activity-dependent block in WT channel-expressing cells. Stimulus-dependent inhibition was largely reduced in IVS6 mutants.
Mutations in the IVS6 Region Reduce Voltage- and Frequency-Dependent Block.
Mutations F1764A and Y1771A in transmembrane segment IVS6 of the Na+ channel α subunit have been shown to affect the interaction of local anesthetics, anticonvulsants, and antiarrhythmics with rIIA channels without strong inhibitory effects on steady-state inactivation (32, 33). This was also the case for the blockade of Na+ channels by BIII 890 CL. The IC50 values for block of inactivated Na+ channels was 349 ± 52 nM (Hill coefficient, −0.97 ± 0.14; n = 4) for the F1764A mutant and 619 ± 14 nM (Hill coefficient −1.00 ± 0.03; n = 3) for the Y1771A mutant. Thus, affinities for BIII 890 CL were reduced 4.5- and 8-fold for these mutants, compared with WT channels (Fig. 2B). Blockade of resting channels was not affected (data not shown). This compound induced stimulus-dependent blockade upon the application of a train of depolarizing stimuli. As shown in Fig. 2C, 1.85 μM BIII 890 CL induced pronounced activity-dependent inhibition of Na+ currents after 100 stimuli at 5 Hz in WT channels, whereas inhibition was almost absent in the two IVS6 mutants. These results indicate that BIII 890 CL is a high-affinity, stimulus-dependent blocker at the local anesthetic receptor site.
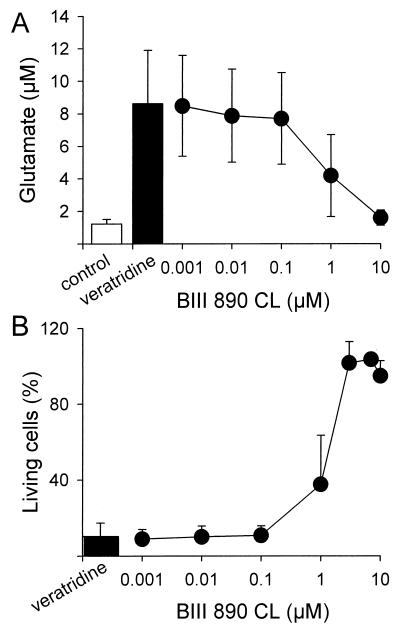
Inhibition of Veratridine-Stimulated Glutamate Release and Neurotoxicity in Brain Slices and Cultured Cortical Neurons.
We initially investigated the ability of BIII 890 CL to inhibit veratridine-induced glutamate release in brain slices from either cortex or striatum of rat brain. BIII 890 CL inhibited glutamate release stimulated by 3 μM veratridine with an IC50 of 0.29 ± 0.02 μM (n = 4) in cortical slices and an IC50 of 0.33 μM (n = 2) in striatal slices. Short veratridine treatments of cultured cortical neurons (20 min) initiate steady glutamate release that is maintained in the absence of veratridine for >24 h and leads to subsequent neuronal death (data not shown). BIII 890 CL prevented such glutamate release induced by the addition of 10 μM veratridine to cultures of cortical neurons with an IC50 of 1.2 μM (Fig. 3A). Moreover, BIII 890 CL also prevented the neurotoxicity induced by the addition of 10 μM veratridine in parallel cultures with an IC50 of 0.66 μM (Fig. 3B). Incubation with 10 μM BIII 890 CL completely inhibited the glutamate release and neurotoxicity induced by the addition of veratridine.
Figure 3.
The effect of BIII 890 CL on veratridine-induced glutamate release and neurotoxicity in serum-free cultures of rat cortical neurons. Neurons were treated with veratridine (10 μM) for 20 min either with or without different concentrations of BIII 890 CL, the compound was washed out, and the effects of veratridine on cell viability and glutamate release were quantified 24 h later. We expressed the number of living cells in each treatment group as a percentage of healthy untreated neurons.
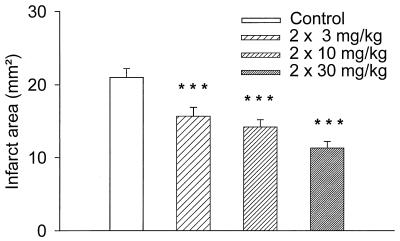
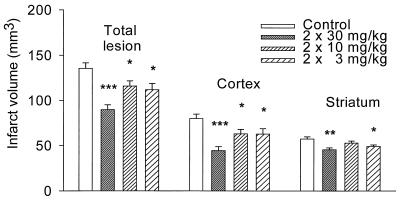
BIII 890 CL Reduces Lesion Size after Occlusion of MCA in Rodents.
BIII 890 CL administered at doses of 3, 10, and 30 mg/kg s.c. at 5 min and 3 h after commencing ischemia reduced the cortical infarct area in mice that had been subjected to focal cerebral ischemia by unilateral occlusion of the MCA (Fig. 4). The effects were statistically significant with the lowest dose tested (3 mg/kg s.c.). BIII 890 CL administered at doses of 3, 10, and 30 mg/kg also reduced the cerebral infarct volume in rats that had been subjected to focal cerebral ischemia by unilateral occlusion of the MCA (Fig. 5). Again, the effects achieved statistical significance with a dose of 3 mg/kg s.c. A more detailed histological analysis revealed that BIII 890 CL also exhibited significant neuroprotective effects in the striatum. None of these doses of BIII 890 CL elicited any evident side effects in the rats and mice. BIII 890 CL did not interfere with motor coordination at doses of up to 30 mg/kg as measured by the rotarod method.
Figure 4.
The effects of BIII 890 CL on the cortical infarct area in mice that had been subjected to focal cerebral ischemia by unilateral occlusion of the MCA. Mice were treated with BIII 890 CL at doses of 3, 10, and 30 mg/kg administered s.c. at 5 min and 3 h after occlusion. The cortical infarct areas were determined 48 h after occlusion of the MCA by staining with tetrazolium chloride and computer-aided image analysis. The results are expressed as the mean ± SEM of 24–31 animals per group. A one-way ANOVA and Dunnett's multiple comparison test were used to determine which treatment groups were significantly different from the control group. *, P < 0.05; **, P < 0.01; ***, P < 0.001.
Figure 5.
The effects of BIII 890 CL on the cerebral infarct volume in rats that had been previously subjected to focal cerebral ischemia by unilateral occlusion of the MCA. BIII 890 CL was administered at doses of 3, 10, and 30 mg/kg at 5 min and 3 h after commencing ischemia. The cerebral infarct volumes were determined 48 h after occlusion of the MCA by standard histological techniques. The results are expressed as the mean ± SEM of 17–22 animals per group. Statistical evaluation was as described for Fig. 4.
Discussion
High Affinity and Specificity of Binding of BIII 890 CL to Na+ Channels.
We determined the ability of a benzomorphan derivative, BIII 890 CL, to block voltage-gated Na+ channels in vitro and in vivo. Previous results showed that it is possible to separate the opioid activity from the NMDA-blocking activity for another benzomorphan structure, namely BIII 277 (17, 18). The present study shows that we can obtain a compound from the same structural class that binds to the Na+ channel without blocking the NMDA receptor or other ion-channel receptor sites. BIII 890 CL displaced [3H]BTX from site 2 of the Na+ channel (IC50 = 49 nM), yet exhibited only low binding affinity for 65 other receptors and ion channels, including site 1 of the Na+ channel. Thus, BIII 890 CL binds to the Na+ channel with both high affinity and specificity and is one of the most potent and specific Na+ channel blockers currently available.
State-Dependent Binding of BIII 890 CL.
Local anesthetics and other drugs that inhibit BTX-b binding block sodium channels in a strongly voltage-dependent manner (34). Thus, voltage-dependent reduction of channel availability by BIII 890 CL is expected from its effects on BTX-b binding (24). The electrophysiological data for the inhibition of inactivated Na+ channels agree closely with the binding data. The IC50 value for functional block of inactivated Na+ channels was 77 nM, and the IC50 for inhibition of BTX-b binding was 49 nM. Thus, the BTX-binding assay is a simple and accurate predictor of the inhibition of Na+ channels in the inactivated state for this series of compounds. The low affinity of BIII 890 CL for resting channels is remarkable, and results in high discrimination between the blockade of resting and inactivated channels (230-fold). We therefore anticipate that BIII 890 CL will preferentially block Na+ channel in ischemic nerve tissue that is depolarized without pronounced effects on healthy neurons with physiological membrane potentials. This contrasts favorably with the results with weaker Na+ channel blockers, such as mexiletine and BW619C89. Mexiletine differentiated 15-fold between resting and inactivated states under comparable experimental conditions (25), and BW619C89 by factor of about 6 (35).
BIII 890 CL Binds to the Local Anesthetic Receptor Site.
Our data provide evidence that BIII 890 CL binds to the local anesthetic site of the Na+ channel. The inhibition of BTX-b binding and the negative shift of inactivation curves resemble the effects of local anesthetics in binding to their receptor site. Moreover, we found that mutations in the local anesthetic receptor site in transmembrane segment IVS6 reduced the affinity for block of Na+ channels by BIII 890 CL substantially. Both voltage-dependent and frequency-dependent block were reduced. Together, these results provide strong evidence for binding to a site that includes F1764 and Y1771 and is similar or identical to the site occupied by local anesthetic drugs. Previous studies (25, 33, 36, 37) have shown that voltage- and frequency-dependent blockade induced by several local anesthetics, antiarrhythmics, and anticonvulsants was reduced by point mutations F1764A and Y1771A. Thus, most Na+ channel-blocking drugs appear to bind to the same receptor site in the channel. BIII 890 CL has the highest affinity among ligands described for this site to date.
Neuroprotection by BIII 890 CL in Vitro.
BIII 890 CL inhibited veratridine-induced glutamate release in rat brain slices from cortex and striatum, and in cultures of cortical neurons with IC50 values of approximately 0.3 μM and 1.2 μM, respectively. Furthermore, BIII 890 CL reduced veratridine-induced neurotoxicity in parallel cultures of cortical neurons with an IC50 of 0.7 μM. These experiments indicate that BIII 890 CL blocks the functional consequences of persistent opening of voltage-gated Na+ channels in vitro and give the first indication that BIII 890 CL is neuroprotective. However, the effective concentrations required to prevent glutamate release and neurotoxicity in brain slices and neuronal cell cultures are approximately 10-fold higher than the IC50 values in BTX-b binding and electrophysiological experiments. This comparison suggests that equilibrium drug binding was not achieved or that block of more than 90% of the Na+ channels is required for half-maximal inhibition of glutamate release and neurotoxicity. We have observed a similar phenomenon with an NMDA antagonist previously (17).
BIII 890 CL Protects Brain Tissue in Vivo.
Our results demonstrate that BIII 890 CL protects brain tissue from ischemia in vivo. Animal models of cerebral ischemia generally fall into two classes: global and focal (38). Global ischemia produces a lesion in a large area of the brain and causes selective neuronal loss in vulnerable brain regions. In contrast, focal ischemia produces infarction in clearly defined regions of the brain, and is probably more relevant to acute ischemic stroke (39). In models of permanent focal ischemia, BIII 890 CL reduced lesion size significantly at the lowest doses tested, and maximum effects were comparable with the effects of the NMDA receptor antagonists, (+)MK-801, BIII 277 CL, and CGP 37849, in similar models (17, 30). Moreover, BIII 890 CL did not disturb motor coordination at these doses as NMDA receptor antagonists have been shown to do (6).
Importantly, BIII 890 CL was neuroprotective in both cortical and subcortical regions of the rat brain. These results show that a Na+ channel blocker can have neuroprotective effects in a region rich in white matter, like the striatum. The white matter of the mammalian brain is also susceptible to ischemic injury (40). However, little is known about the pathophysiology of this process, despite the requirement for neurons to communicate by means of their axons located in the white matter (41). Depriving the white matter of energy causes membrane depolarization and Na+ influx through voltage-gated Na+ channels (42). The resulting rise in intracellular [Na+] causes damaging levels of Ca2+ to enter the axons by reversing the pumping activity of the Na+/Ca2+ exchanger. Neuroprotective agents such as NMDA receptor antagonists have targeted only grey matter because NMDA receptors are not located in axons (43). In contrast, blockers of voltage-dependent Na+ channels, such as TTX and saxitoxin, prevent anoxic damage in mammalian white matter as well (42).
Voltage-dependent Na+ channels have been implicated in excitotoxic neuronal death in both white and grey matter after cerebral ischemia. However, almost all Na+ channel blockers hitherto clinically tested are weak, unspecific, or do not discriminate well between resting and inactivated states of the channel. BIII 890 CL is a benzomorphan derivative that overcomes these disadvantages. Our results demonstrate that BIII 890 CL is a potent, selective, and highly use-dependent Na+ channel blocker that protects brain tissue from the deleterious effects of permanent focal cerebral ischemia in rodents at doses that do not disturb motor coordination. It therefore could be used as a neuroprotective therapy for the treatment of acute thromboembolic stroke. Phase I clinical trials are currently in progress.
Acknowledgments
We thank Rosi Ewen, Sandra Reichert, Hans-Hermann Dechent, Ute Müller, Birgit Christmann, Birgit Brunck, Helmar Schiller, Annette Schwientek, Stephan Kurtze, Holger Werle, Hanfried Baltes, and Elisabeth Weghofer for their expert technical assisitance, as well as Dr. Joachim Theinhardt and Gerhard Weckesser of the Department of Research and Development Coordination for statistically evaluating the data. Research at Boehringer Ingelheim was partly supported by Research Grant 0319520B from the Federal Ministry of Education, Science, Research and Technology (BMBF) (to A.J.C and T.W.), and research at the University of Washington was supported by Research Grant NS15751 from the National Institutes of Health (to W.A.C.).
Abbreviations
- BIII 890 CL
2R-[2α,3(S*),6α]-1,2,3,4,5,6-hexahydro-6,11,11-trimethyl-3-[2-(phenylmethoxy)propyl]-2,6-methano-3-benzazocin-10-ol hydrochloride
- WT
wild type
- BTX-b
batrachotoxinin A-20α-benzoate
- NMDA
N-methyl-d-aspartate
- MCA
middle cerebral artery
- TTX
tetrodotoxin
Footnotes
Article published online before print: Proc. Natl. Acad. Sci. USA, 10.1073/pnas.040577097.
Article and publication date are at www.pnas.org/cgi/doi/10.1073/pnas.040577097
References
- 1.Bonita R. Lancet. 1992;339:342–344. doi: 10.1016/0140-6736(92)91658-u. [DOI] [PubMed] [Google Scholar]
- 2.Lee J-M, Zipfel G J, Choi D W. Nature (London) 1999;399,Suppl.:A7–A14. doi: 10.1038/399a007. [DOI] [PubMed] [Google Scholar]
- 3.Parsons C G, Danysz W, Quack G. Drug News Perspect. 1998;11:523–569. doi: 10.1358/dnp.1998.11.9.863689. [DOI] [PubMed] [Google Scholar]
- 4.Simon R P, Swan J H, Griffiths T, Meldrum B S. Science. 1984;226:850–852. doi: 10.1126/science.6093256. [DOI] [PubMed] [Google Scholar]
- 5.Park C K, Nehls D G, Graham D I, Teasdale G M, McCulloch J. Ann Neurol. 1988;24:543–551. doi: 10.1002/ana.410240411. [DOI] [PubMed] [Google Scholar]
- 6.Carter A J. J Pharmacol Exp Ther. 1994;269:573–580. [PubMed] [Google Scholar]
- 7.Muir K W, Lees K R. Stroke. 1995;26:503–513. doi: 10.1161/01.str.26.3.503. [DOI] [PubMed] [Google Scholar]
- 8.Carter A J. Amino Acids. 1998;14:159–169. doi: 10.1007/BF01345257. [DOI] [PubMed] [Google Scholar]
- 9.Taylor C P, Meldrum B S. Trends Pharmacol Sci. 1995;16:309–316. doi: 10.1016/s0165-6147(00)89060-4. [DOI] [PubMed] [Google Scholar]
- 10.Hille B. J Gen Physiol. 1977;69:497–515. doi: 10.1085/jgp.69.4.497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Catterall W A. Physiol Rev. 1992;72:S15–S48. doi: 10.1152/physrev.1992.72.suppl_4.S15. [DOI] [PubMed] [Google Scholar]
- 12.Squire I B, Lees K R, Pryse-Phillips W, Kertesz A, Bamford J. Cereb Dis. 1996;6:156–160. [Google Scholar]
- 13.Brown N A, Kemp J A, Seabrook G R. Br J Pharmacol. 1994;113:600–606. doi: 10.1111/j.1476-5381.1994.tb17032.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Marrannes R, De Prins E, Clincke G. J Pharmacol Exp Ther. 1998;286:201–214. [PubMed] [Google Scholar]
- 15.Hickenbottom S L, Grotta J. Semin Neurol. 1998;18:485–492. doi: 10.1055/s-2008-1040901. [DOI] [PubMed] [Google Scholar]
- 16.Netzer R, Pflimlin P, Trube G. Eur J Pharmacol. 1993;238:209–216. doi: 10.1016/0014-2999(93)90849-d. [DOI] [PubMed] [Google Scholar]
- 17.Carter A J, Bechtel W D, Grauert M, Harrison P, Merz H, Stransky W. J Pharmacol Exp Ther. 1995;275:1382–1389. [PubMed] [Google Scholar]
- 18.Grauert M, Bechtel W D, Ensinger H A, Merz H, Carter A J. J Med Chem. 1997;40:2922–2930. doi: 10.1021/jm970131j. [DOI] [PubMed] [Google Scholar]
- 19.Catterall W A, Morrow C S, Daly J W, Brown G B. J Biol Chem. 1981;256:8922–8927. [PubMed] [Google Scholar]
- 20.Weiser T, Brenner M, Palluk R, Ceci A, Brambilla A, Ensinger H A, Sagrada A, Wienrich M. J Pharmacol Exp Ther. 1999;289:1343–1349. [PubMed] [Google Scholar]
- 21.Meldrum B S, Swan J H, Leach M J, Millan M H, Gwinn R, Kadota K, Graham S H, Chen J, Simon R P. Brain Res. 1992;593:1–6. doi: 10.1016/0006-8993(92)91254-c. [DOI] [PubMed] [Google Scholar]
- 22.Kehr J. J Chromatogr B Biomed Appl. 1998;708:27–38. doi: 10.1016/s0378-4347(97)00677-4. [DOI] [PubMed] [Google Scholar]
- 23.Bradford M M. Anal Biochem. 1976;72:248–254. doi: 10.1016/0003-2697(76)90527-3. [DOI] [PubMed] [Google Scholar]
- 24.Linford N J, Cantrell A R, Qu Y, Scheuer T, Catterall W A. Proc Natl Acad Sci USA. 1998;95:13947–13952. doi: 10.1073/pnas.95.23.13947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Weiser T, Qu Y, Catterall W A, Scheuer T. Mol Pharmacol. 1999;56:1238–1244. doi: 10.1124/mol.56.6.1238. [DOI] [PubMed] [Google Scholar]
- 26.Stichel C C, Müller H W. Dev Brain Res. 1991;64:145–154. doi: 10.1016/0165-3806(91)90218-8. [DOI] [PubMed] [Google Scholar]
- 27.Brewer G J, Torricelli J R, Evege E K, Price P J. J Neurosci Res. 1993;35:567–576. doi: 10.1002/jnr.490350513. [DOI] [PubMed] [Google Scholar]
- 28.Banker G A, Cowan W M. Brain Res. 1977;126:397–425. doi: 10.1016/0006-8993(77)90594-7. [DOI] [PubMed] [Google Scholar]
- 29.Mosmann T. J Immunol Methods. 1983;65:55–63. doi: 10.1016/0022-1759(83)90303-4. [DOI] [PubMed] [Google Scholar]
- 30.Pschorn U, Carter A J. J Stroke Cerebrovasc Dis. 1996;6:93–99. doi: 10.1016/s1052-3057(96)80010-3. [DOI] [PubMed] [Google Scholar]
- 31.Postma S W, Catterall W A. Mol Pharmacol. 1984;25:219–927. [PubMed] [Google Scholar]
- 32.Ragsdale D S, McPhee J C, Scheuer T, Catterall W A. Science. 1994;265:1724–1728. doi: 10.1126/science.8085162. [DOI] [PubMed] [Google Scholar]
- 33.Ragsdale D S, McPhee J C, Scheuer T, Catterall W A. Proc Natl Acad Sci USA. 1996;93:9270–9275. doi: 10.1073/pnas.93.17.9270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Catterall W A. Trends Pharmacol Sci. 1987;8:57–65. doi: 10.1016/0165-6147(92)90079-l. [DOI] [PubMed] [Google Scholar]
- 35.Xie X M, Garthwaite J. Neuroscience. 1996;73:951–962. doi: 10.1016/0306-4522(96)00092-9. [DOI] [PubMed] [Google Scholar]
- 36.Wright S N, Wang S Y, Wang G K. Mol Pharmacol. 1998;54:733–739. [PubMed] [Google Scholar]
- 37.Li H L, Galue A, Meadows L, Ragsdale D S. Mol Pharmacol. 1999;55:134–141. doi: 10.1124/mol.55.1.134. [DOI] [PubMed] [Google Scholar]
- 38.Ginsberg M D, Busto R. Stroke. 1989;20:1627–1642. doi: 10.1161/01.str.20.12.1627. [DOI] [PubMed] [Google Scholar]
- 39.Macrae I M. Br J Clin Pharmacol. 1992;34:302–308. doi: 10.1111/j.1365-2125.1992.tb05634.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ransom B R, Stys P K, Waxman S G. Stroke. 1990;21:III-52–III-57. [PubMed] [Google Scholar]
- 41.Stys P K. In: Advances in Neurology, Vol. 71; Cellular and Molecular Mechanisms of Ischemic Brain Damage. Siesjö B K, Wieloch T, editors. Philadelphia: Lippincott; 1996. pp. 153–166. [Google Scholar]
- 42.Stys P K, Waxman S G, Ransom B R. J Neurosci. 1992;12:430–439. doi: 10.1523/JNEUROSCI.12-02-00430.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Dewar D, Yam P, McCulloch J. Eur J Pharmacol. 1999;375:41–50. doi: 10.1016/s0014-2999(99)00280-0. [DOI] [PubMed] [Google Scholar]