Abstract
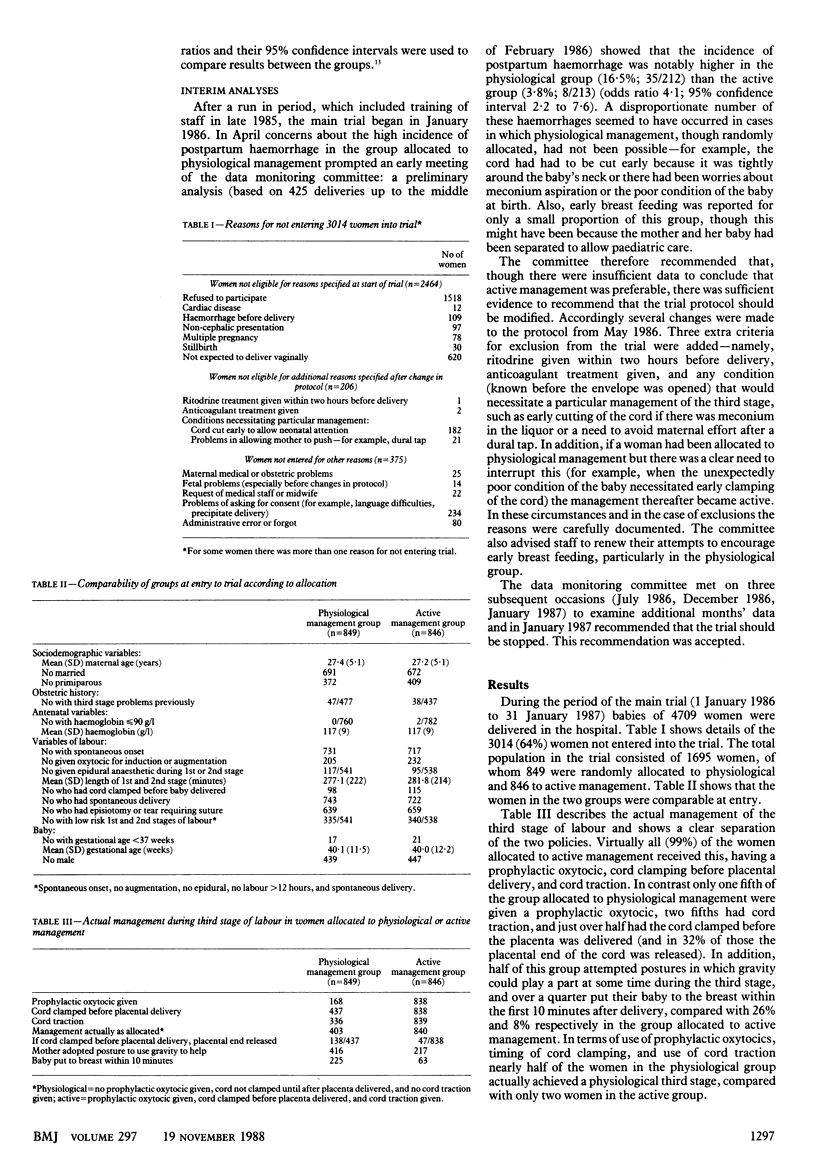
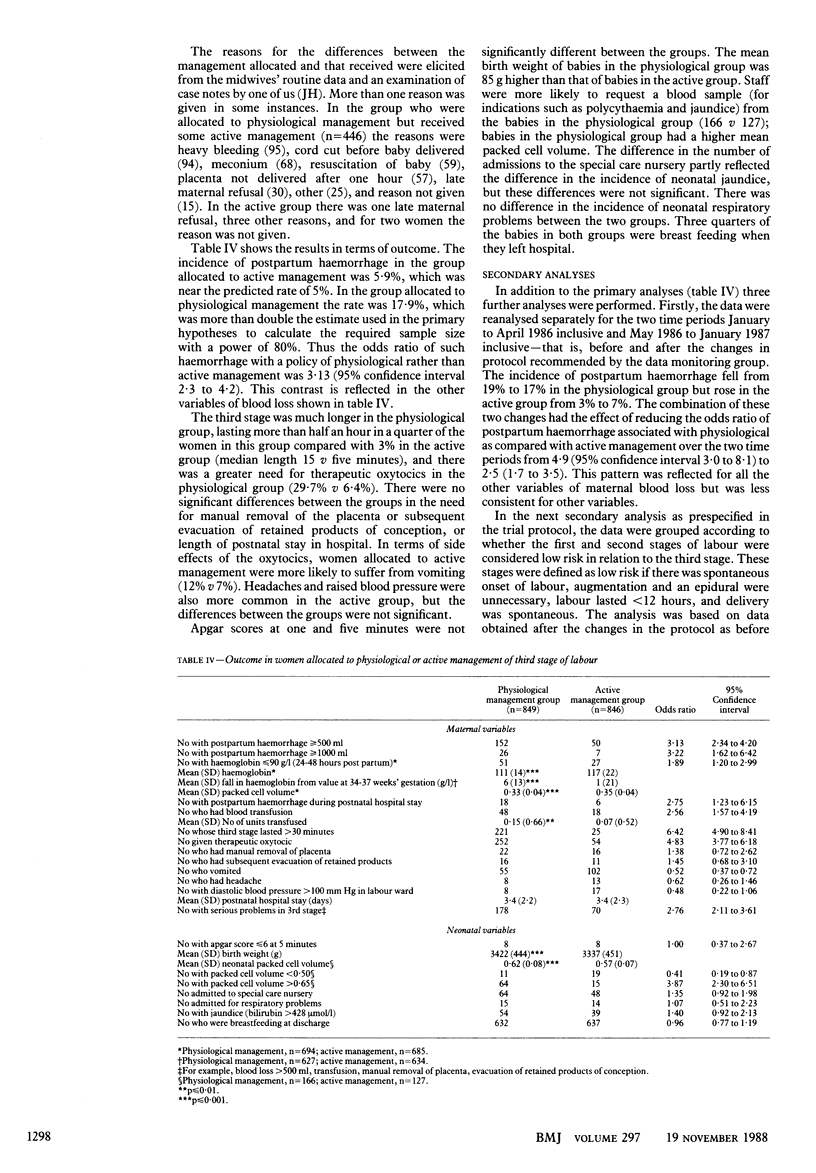
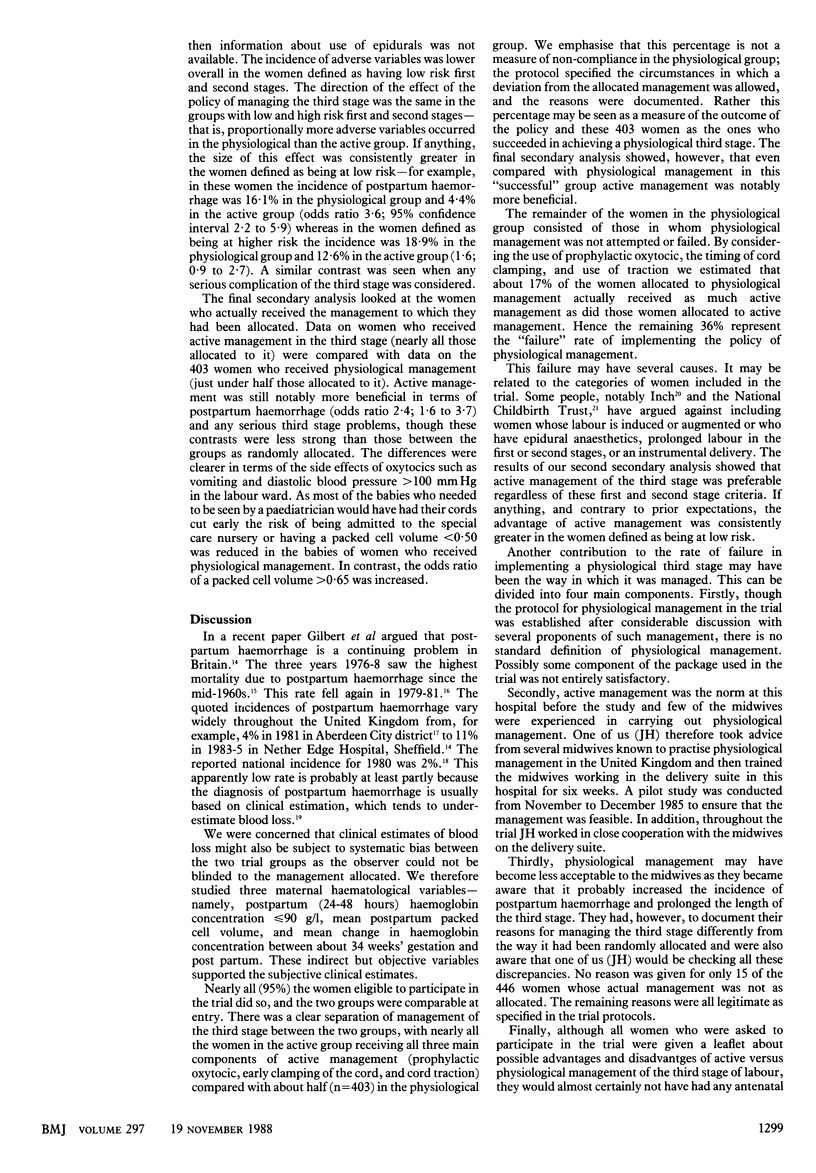
OBJECTIVE--To compare the effects on fetal and maternal morbidity of routine active management of third stage of labour and expectant (physiological) management, in particular to determine whether active management reduced incidence of postpartum haemorrhage. DESIGN--Randomised trial of active versus physiological management. Women entered trial on admission to labour ward with allocation revealed just before vaginal delivery. Five months into trial high rate of postpartum haemorrhage in physiological group (16.5% v 3.8%) prompted modification of protocol to exclude more women and allow those allocated to physiological group who needed some active management to be switched to fully active management. Sample size of 3900 was planned, but even after protocol modification a planned interim analysis after first 1500 deliveries showed continuing high postpartum haemorrhage rate in physiological group and study was stopped. SETTING--Maternity hospital. PARTICIPANTS--Of 4709 women delivered from 1 January 1986 to 31 January 1987, 1695 were admitted to trial and allocated randomly to physiological (849) or active (846) management. Reasons for exclusion were: refusal, antepartum haemorrhage, cardiac disease, breech presentation, multiple pregnancy, intrauterine death, and, after May 1986, ritodrine given two hours before delivery, anticoagulant treatment, and any condition needing a particular management of third stage. INTERVENTIONS--All but six women allocated to active management actually received it, having prophylactic oxytocic, cord clamping before placental delivery, and cord traction; whereas just under half those allocated to physiological management achieved it. A fifth of physiological group received prophylactic oxytocic, two fifths underwent cord traction and just over half clamping of the cord before placental delivery. ENDPOINT--Reduction in incidence of postpartum haemorrhage from 7.5% under physiological management to 5.0% under active management. MEASUREMENTS AND MAIN RESULTS--Incidence of postpartum haemorrhage was 5.9% in active management group and 17.9% in physiological group (odds ratio 3.13; 95% confidence interval 2.3 to 4.2), a contrast reflected in other indices of blood loss. In physiological group third stage was longer (median 15 min v 5 min) and more women needed therapeutic oxytocics (29.7% v 6.4%). Apgar scores at one and five minutes and incidence of neonatal respiratory problems were not significantly different between groups. Babies in physiological group weighed mean of 85 g more than those in active group. When women allocated to and receiving active management (840) were compared with those who actually received physiological management (403) active management still produced lower rate of postpartum haemorrhage (odds ratio 2.4;95% CI1.6 to 3.7). CONCLUSIONS--Policy of active management practised in this trial reduces incidence of postpartum haemorrhage, shortens third stage, and results in reduced neonatal packed cell volume.
Full text
PDF


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Dunn P. M., Fraser I. D., Raper A. B. Influence of early cord ligation on the transplacental passage of foetal cells. J Obstet Gynaecol Br Commonw. 1966 Oct;73(5):757–760. doi: 10.1111/j.1471-0528.1966.tb06079.x. [DOI] [PubMed] [Google Scholar]
- Dunn P. M. Postnatal placental respiration. Dev Med Child Neurol. 1966 Oct;8(5):607–608. doi: 10.1111/j.1469-8749.1966.tb01809.x. [DOI] [PubMed] [Google Scholar]
- Dunn P. M. The placental venous pressure during and after the third stage of labour following early cord ligation. J Obstet Gynaecol Br Commonw. 1966 Oct;73(5):747–756. doi: 10.1111/j.1471-0528.1966.tb06078.x. [DOI] [PubMed] [Google Scholar]
- Elbourne D., Prendiville W., Chalmers I. Choice of oxytocic preparation for routine use in the management of the third stage of labour: an overview of the evidence from controlled trials. Br J Obstet Gynaecol. 1988 Jan;95(1):17–30. doi: 10.1111/j.1471-0528.1988.tb06476.x. [DOI] [PubMed] [Google Scholar]
- Garcia J., Garforth S., Ayers S. The policy and practice in midwifery study: introduction and methods. Midwifery. 1987 Mar;3(1):2–9. doi: 10.1016/s0266-6138(87)80003-7. [DOI] [PubMed] [Google Scholar]
- Gilbert L., Porter W., Brown V. A. Postpartum haemorrhage--a continuing problem. Br J Obstet Gynaecol. 1987 Jan;94(1):67–71. doi: 10.1111/j.1471-0528.1987.tb02255.x. [DOI] [PubMed] [Google Scholar]
- Hall M. H., Halliwell R., Carr-Hill R. Concomitant and repeated happenings of complications of the third stage of labour. Br J Obstet Gynaecol. 1985 Jul;92(7):732–738. doi: 10.1111/j.1471-0528.1985.tb01456.x. [DOI] [PubMed] [Google Scholar]
- Houlton M., Austin J., Jenkins D., Turner G. M., Wilkins D. G. A microcomputer system in the delivery suite. Br J Obstet Gynaecol. 1984 Jun;91(6):555–559. doi: 10.1111/j.1471-0528.1984.tb04802.x. [DOI] [PubMed] [Google Scholar]
- NEWTON M., MOSEY L. M., EGLI G. E., GIFFORD W. B., HULL C. T. Blood loss during and immediately after delivery. Obstet Gynecol. 1961 Jan;17:9–18. [PubMed] [Google Scholar]
- Prendiville W., Elbourne D., Chalmers I. The effects of routine oxytocic administration in the management of the third stage of labour: an overview of the evidence from controlled trials. Br J Obstet Gynaecol. 1988 Jan;95(1):3–16. doi: 10.1111/j.1471-0528.1988.tb06475.x. [DOI] [PubMed] [Google Scholar]
- Yusuf S., Peto R., Lewis J., Collins R., Sleight P. Beta blockade during and after myocardial infarction: an overview of the randomized trials. Prog Cardiovasc Dis. 1985 Mar-Apr;27(5):335–371. doi: 10.1016/s0033-0620(85)80003-7. [DOI] [PubMed] [Google Scholar]


