Abstract
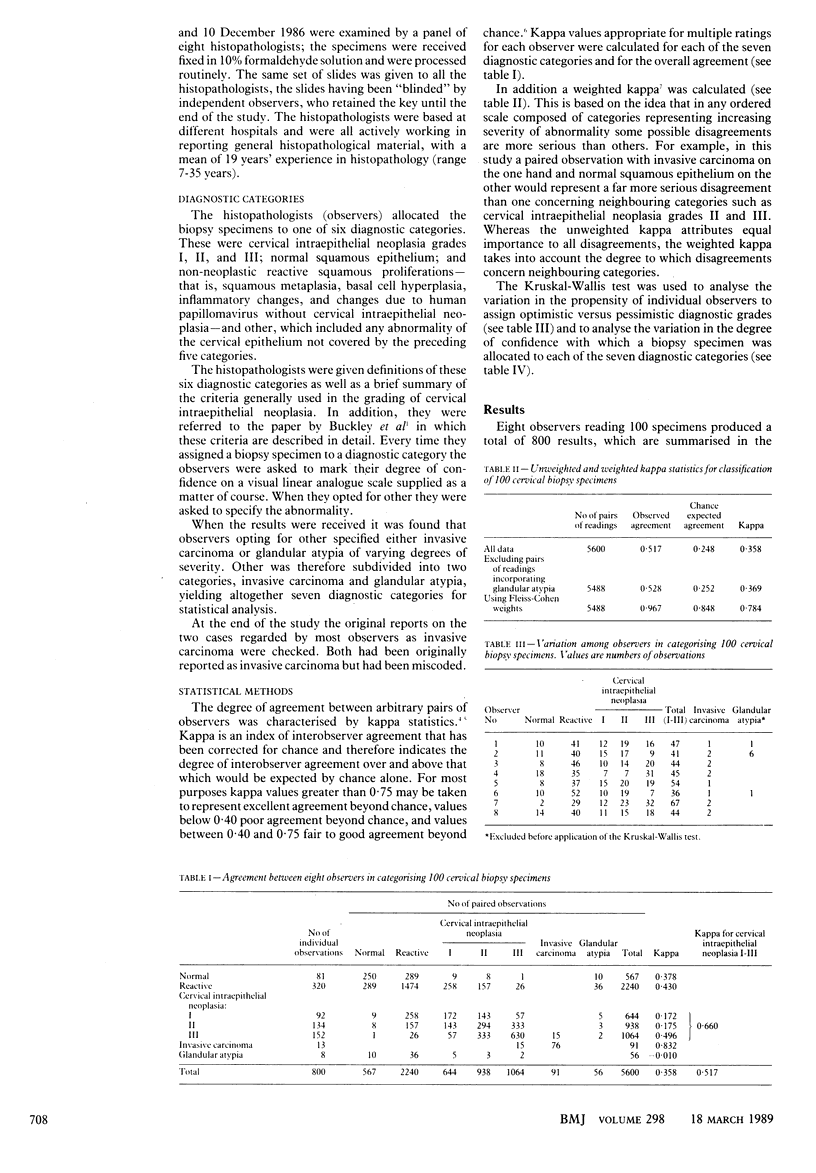
To assess the variability among histopathologists in diagnosing and grading cervical intraepithelial neoplasia eight experienced histopathologists based at different hospitals examined the same set of 100 consecutive colposcopic cervical biopsy specimens and assigned them into one of six diagnostic categories. These were normal squamous epithelium, non-neoplastic squamous proliferations, cervical intraepithelial neoplasia grades I, II, and III, and other. The histopathologists were given currently accepted criteria for diagnosing and grading cervical intraepithelial neoplasia and asked to mark their degree of confidence about their decision on a visual linear analogue scale provided. The degree of agreement between the histopathologists was characterised by kappa statistics, which showed an overall poor agreement (unweighted kappa 0.358). Agreement between observers was excellent for invasive lesions, moderately good for cervical intraepithelial neoplasia grade III, and poor for cervical intraepithelial neoplasia grades I and II (unweighted kappa 0.832, 0.496, 0.172, and 0.175, respectively); the kappa value for all grades of cervical intraepithelial neoplasia taken together was 0.660. The most important source of disagreement lay in the distinction of reactive squamous proliferations from cervical intraepithelial neoplasia grade I. The histopathologists were confident in diagnosing cervical intraepithelial neoplasia grade III and invasive carcinoma (other) but not as confident in diagnosing cervical intraepithelial neoplasia grades I and II and glandular atypia (other). Experienced histopathologists show considerable interobserver variability in grading cervical intraepithelial neoplasia and more importantly in distinguishing between reactive squamous proliferations and cervical intraepithelial neoplasia grade I. It is suggested that the three grade division of cervical intraepithelial neoplasia should be abandoned and a borderline category introduced that entails follow up without treatment.
Full text
PDF


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Barron B. A., Richart R. M. A statistical model of the natural history of cervical carcinoma based on a prospective study of 557 cases. J Natl Cancer Inst. 1968 Dec;41(6):1343–1353. [PubMed] [Google Scholar]
- Beck J. S. Observer variability in reporting of breast lesions. J Clin Pathol. 1985 Dec;38(12):1358–1365. doi: 10.1136/jcp.38.12.1358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckley C. H., Butler E. B., Fox H. Cervical intraepithelial neoplasia. J Clin Pathol. 1982 Jan;35(1):1–13. doi: 10.1136/jcp.35.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christopherson W. M. Concepts of genesis and development in early cervical neoplasia. Obstet Gynecol Surv. 1969 Jul;24(7 Pt 2):842–850. doi: 10.1097/00006254-196907001-00014. [DOI] [PubMed] [Google Scholar]
- Cocker J., Fox H., Langley F. A. Consistency in the histological diagnosis of epithelial abnormalities of the cervix uteri. J Clin Pathol. 1968 Jan;21(1):67–70. doi: 10.1136/jcp.21.1.67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fu Y. S., Reagan J. W., Richart R. M. Definition of precursors. Gynecol Oncol. 1981 Oct;12(2 Pt 2):S220–S231. doi: 10.1016/0090-8258(81)90076-7. [DOI] [PubMed] [Google Scholar]
- Landis J. R., Koch G. G. The measurement of observer agreement for categorical data. Biometrics. 1977 Mar;33(1):159–174. [PubMed] [Google Scholar]
- Nasiell K., Nasiell M., Vaćlavinková V. Behavior of moderate cervical dysplasia during long-term follow-up. Obstet Gynecol. 1983 May;61(5):609–614. [PubMed] [Google Scholar]
- Robertson J. H., Woodend B. E., Crozier E. H., Hutchinson J. Risk of cervical cancer associated with mild dyskaryosis. BMJ. 1988 Jul 2;297(6640):18–21. doi: 10.1136/bmj.297.6640.18. [DOI] [PMC free article] [PubMed] [Google Scholar]


