Abstract
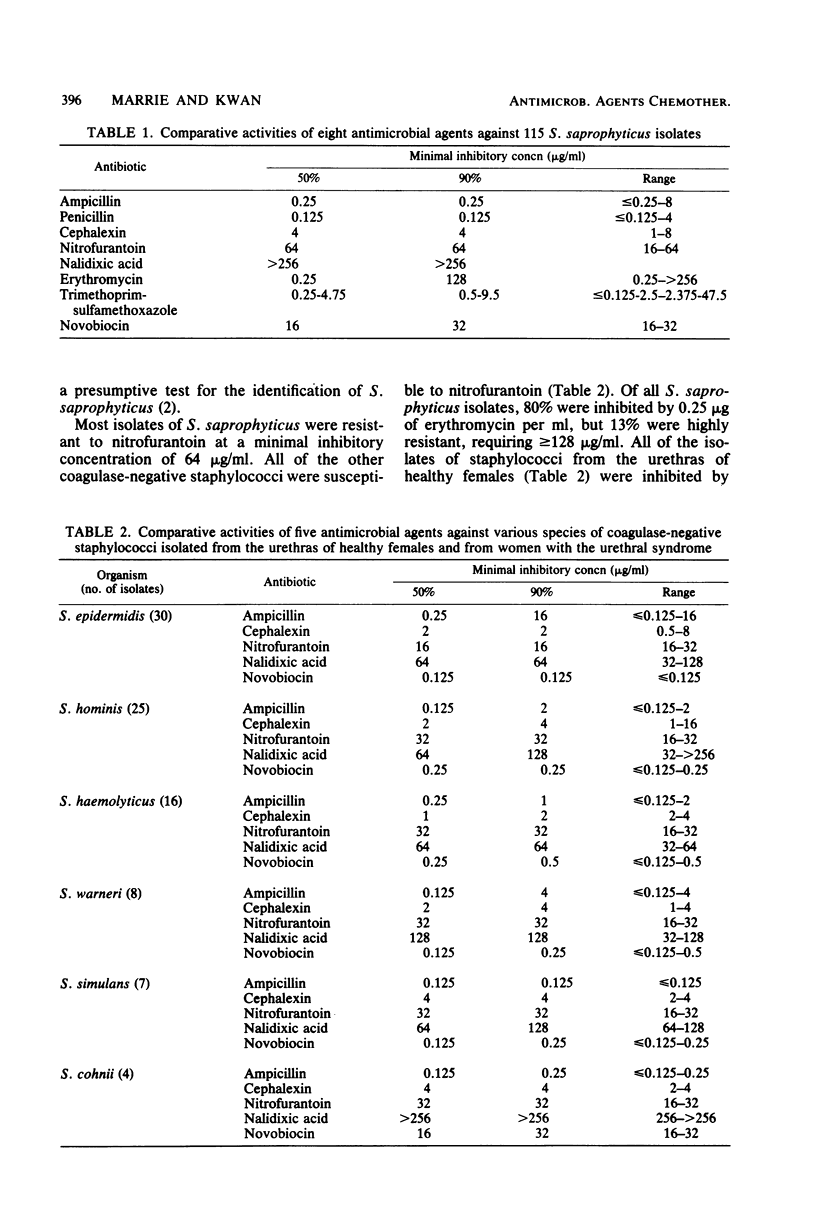
The activity of eight antimicrobial agents was determined against 115 isolates of Staphylococcus saprophyticus. All were susceptible to ampicillin, cephalexin, and trimethoprim-sulfamethoxazole and resistant to nalidixic acid and novobiocin. A bimodal pattern of susceptibility to erythromycin was observed: 80% were inhibited by 0.25 microgram/ml, whereas 13% required greater than or equal to 128 micrograms/ml. The following urethral staphylococci were susceptible to ampicillin, cephalexin, and nitrofurantoin but resistant to nalidixic acid: S. epidermidis, S. hominis, S. haemolyticus, S. warneri, S. simulans, and S. cohnii.
Full text
PDF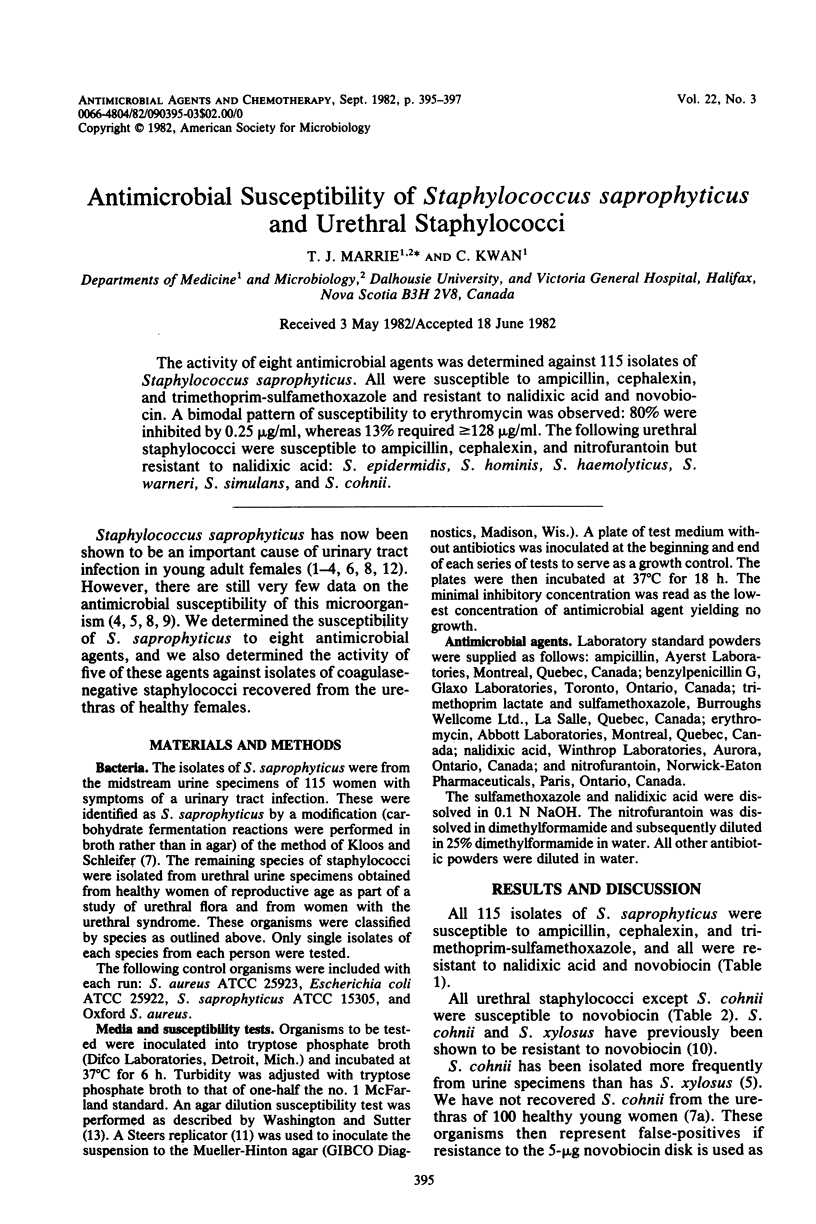
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Anderson J. D., Clarke A. M., Anderson M. E., Isaac-Renton J. L., McLoughlin M. G. Urinary tract infections due to Staphylococcus saprophyticus biotype 3. Can Med Assoc J. 1981 Feb 15;124(4):415–418. [PMC free article] [PubMed] [Google Scholar]
- Digranes A., Oeding P. Characterization of Micrococcaceae from the urinary tract. Acta Pathol Microbiol Scand B. 1975 Aug;83(4):373–381. doi: 10.1111/j.1699-0463.1975.tb00115.x. [DOI] [PubMed] [Google Scholar]
- Hovelius B., Mårdh P. A., Bygren P. Urinary tract infections caused by Staphylococcus saprophyticus: recurrences and complications. J Urol. 1979 Nov;122(5):645–647. doi: 10.1016/s0022-5347(17)56541-6. [DOI] [PubMed] [Google Scholar]
- Hovelius B., Thelin I., Mårdh P. A. Staphylococcus saprophyticus in the aetiology of nongonococcal urethritis. Br J Vener Dis. 1979 Oct;55(5):369–374. doi: 10.1136/sti.55.5.369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- John J. F., Jr, Gramling P. K., O'Dell N. M. Species identification of coagulase-negative staphylococci from urinary tract isolates. J Clin Microbiol. 1978 Oct;8(4):435–437. doi: 10.1128/jcm.8.4.435-437.1978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jordan P. A., Iravani A., Richard G. A., Baer H. Urinary tract infection caused by Staphylococcus saprophyticus. J Infect Dis. 1980 Oct;142(4):510–515. doi: 10.1093/infdis/142.4.510. [DOI] [PubMed] [Google Scholar]
- Kloos W. E., Schleifer K. H. Simplified scheme for routine identification of human Staphylococcus species. J Clin Microbiol. 1975 Jan;1(1):82–88. doi: 10.1128/jcm.1.1.82-88.1975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marrie T. J., Kwan C., Noble M. A., West A., Duffield L. Staphylococcus saprophyticus as a cause of urinary tract infections. J Clin Microbiol. 1982 Sep;16(3):427–431. doi: 10.1128/jcm.16.3.427-431.1982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meers P. D., Whyte W., Sandys G. Coagulase-negative staphylococci and micrococci in urinary tract infections. J Clin Pathol. 1975 Apr;28(4):270–273. doi: 10.1136/jcp.28.4.270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richardson J. F., Marples R. R. Differences in antibiotic susceptibility between Staphylococcus epidermidis and Staphylococcus saprophyticus. J Antimicrob Chemother. 1980 Jul;6(4):499–510. doi: 10.1093/jac/6.4.499. [DOI] [PubMed] [Google Scholar]
- Wallmark G., Arremark I., Telander B. Staphylococcus saprophyticus: a frequent cause of acute urinary tract infection among female outpatients. J Infect Dis. 1978 Dec;138(6):791–797. doi: 10.1093/infdis/138.6.791. [DOI] [PubMed] [Google Scholar]


