Abstract
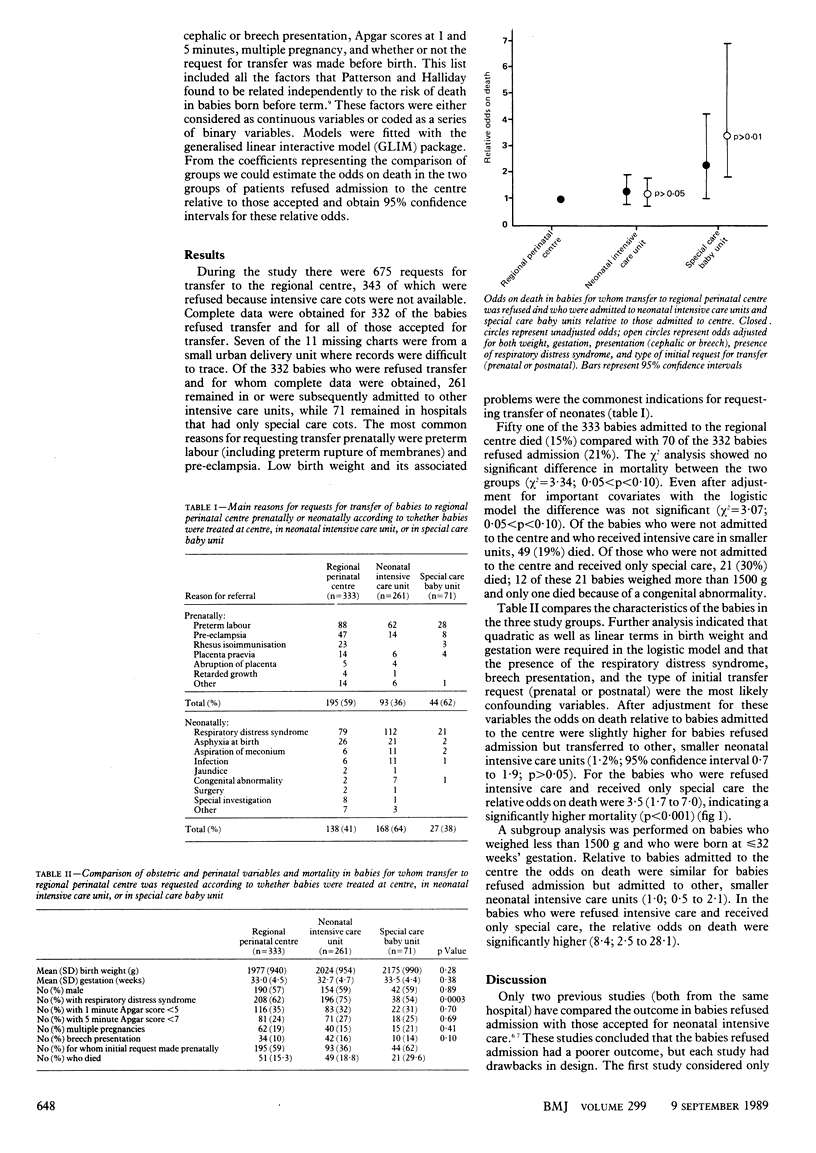
OBJECTIVE--To compare the mortality in babies refused admission to a regional perinatal centre with that in babies accepted for intensive care in the centre. DESIGN--Retrospective study with group comparison. SETTING--Based at the Royal Maternity Hospital, Belfast, with follow up of patients in all obstetric units in Northern Ireland. PATIENTS--Requests for transfer of 675 babies to the regional perinatal centre (prenatally and postnatally) were made from hospitals in Northern Ireland between January 1984 and December 1986. In all, 343 babies were refused admission to the centre, and complete data were available for 332 of them. These babies were either admitted to other neonatal intensive care units (261 babies) or remained in hospitals with only special care cots (71 babies). MAIN OUTCOME MEASURE--Short term mortality. RESULTS--Seventy of the 332 babies refused admission to the centre died compared with 51 of the 333 who were admitted. Multivariate analysis based on a logistic model showed a non-significant increase in mortality among babies treated in other intensive care units compared with babies treated in the centre (relative odds 1.2; 95% confidence interval 0.7 to 1.9). The increase in mortality in babies who remained in a special care baby unit, however, was significant (3.5; 1.7 to 7.0). This increase was particularly significant in babies born at less than or equal to 32 weeks' gestation and who weighed less than 1500 g (8.4; 2.5 to 28.1). CONCLUSIONS--The results of the study confirm the benefits of neonatal intensive care and its particular value in improving survival in babies of low birth weight. As the babies were refused admission to the regional perinatal centre because intensive care cots were not available this deficiency should be corrected.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Blake A. M., Pollitzer M. J., Reynolds E. O. Referral of mothers and infants for intensive care. Br Med J. 1979 Aug 18;2(6187):414–416. doi: 10.1136/bmj.2.6187.414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooke R. Where should low birthweight babies be born? Br Med J (Clin Res Ed) 1986 Oct 18;293(6553):974–975. doi: 10.1136/bmj.293.6553.974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lobb M. O., Morgan M. E., Bond A. P., Cooke R. W. Transfer before delivery on Merseyside: an analysis of the first 140 patients. Br J Obstet Gynaecol. 1983 Apr;90(4):338–341. doi: 10.1111/j.1471-0528.1983.tb08920.x. [DOI] [PubMed] [Google Scholar]
- Patterson C. C., Halliday H. L. Prediction of outcome shortly after delivery for the very low birthweight (less than or equal to 1500 g) infant. Paediatr Perinat Epidemiol. 1988 Jul;2(3):221–228. doi: 10.1111/j.1365-3016.1988.tb00211.x. [DOI] [PubMed] [Google Scholar]
- Powell T. G., Pharoah P. O. Regional neonatal intensive care: bias and benefit. Br Med J (Clin Res Ed) 1987 Sep 19;295(6600):690–692. doi: 10.1136/bmj.295.6600.690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roper H. P., Chiswick M. L., Sims D. G. Referrals to a regional neonatal intensive care unit. Arch Dis Child. 1988 Apr;63(4):403–407. doi: 10.1136/adc.63.4.403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sims D. G., Wynn J., Chiswick M. L. Outcome for newborn babies declined admission to a regional neonatal intensive care unit. Arch Dis Child. 1982 May;57(5):334–337. doi: 10.1136/adc.57.5.334. [DOI] [PMC free article] [PubMed] [Google Scholar]


