Abstract
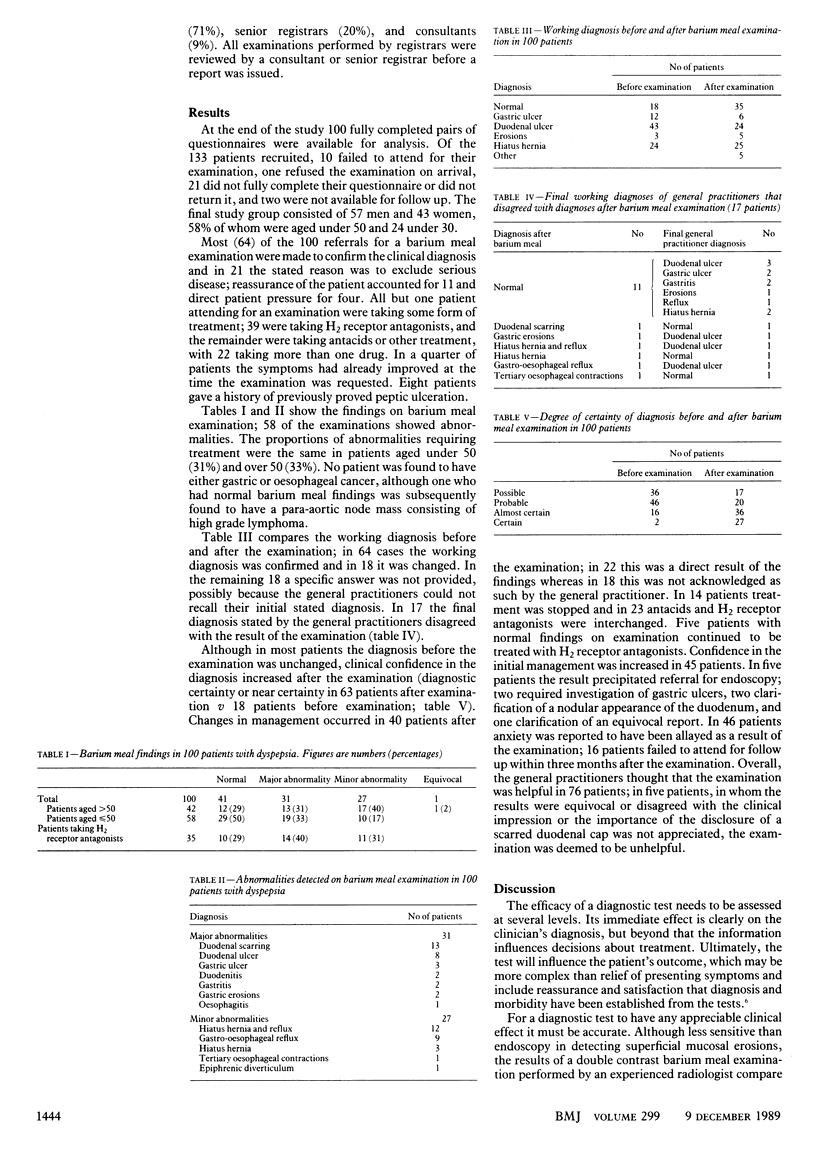
OBJECTIVE--To assess the efficacy of barium meal examinations in managing patients with dyspepsia in general practice. DESIGN--Prospective study by questionnaires completed by general practitioners before and within three to six months after the barium meal examination. Information was requested about the patients' symptoms, current treatment, reason for requesting the examination, and the working diagnosis, including degree of certainty and, after the examination, about any change in diagnosis, diagnostic confidence, or management and to determine whether the examination was judged to be helpful or not. SETTING--Inner city health district. PATIENTS--133 Patients with dyspepsia referred by general practitioners for outpatient barium meal examination, 31 of whom failed to attend for the examination, or refused it on arrival, or did not have fully completed questionnaires. Two patients were not available for follow up. MAIN OUTCOME MEASURES--Prevalence of radiological abnormalities and the influence of the examination result on management, particularly changes in drug treatment. RESULTS--Fully completed pairs of questionnaires were available for 100 patients, 58 of whom were aged below 50. Most of the barium meal reports (64) were to confirm the clinical diagnosis; only 22 were to exclude serious disease. Ninety nine patients were already receiving treatment, with 39 taking an H2 receptor antagonist. Fifty eight barium meal examinations showed abnormalities (31 major abnormalities); there were no cancers and in only 18 patients was the working diagnosis changed as a result of the findings. Although the barium meal result increased management confidence (63 patients) and allayed patients' anxiety (46), changes in management attributed directly to the examination occurred in only 22 patients. Management changes were minor, usually comprising interchange of antacids and H2 receptor antagonists. CONCLUSIONS--Young patients (aged below 50) with dyspepsia are still being overinvestigated. Although barium meal examination improves diagnostic confidence and allays patients' anxiety, fully utilising communication skills at the initial consultation might allay anxiety more economically.
Full text
PDF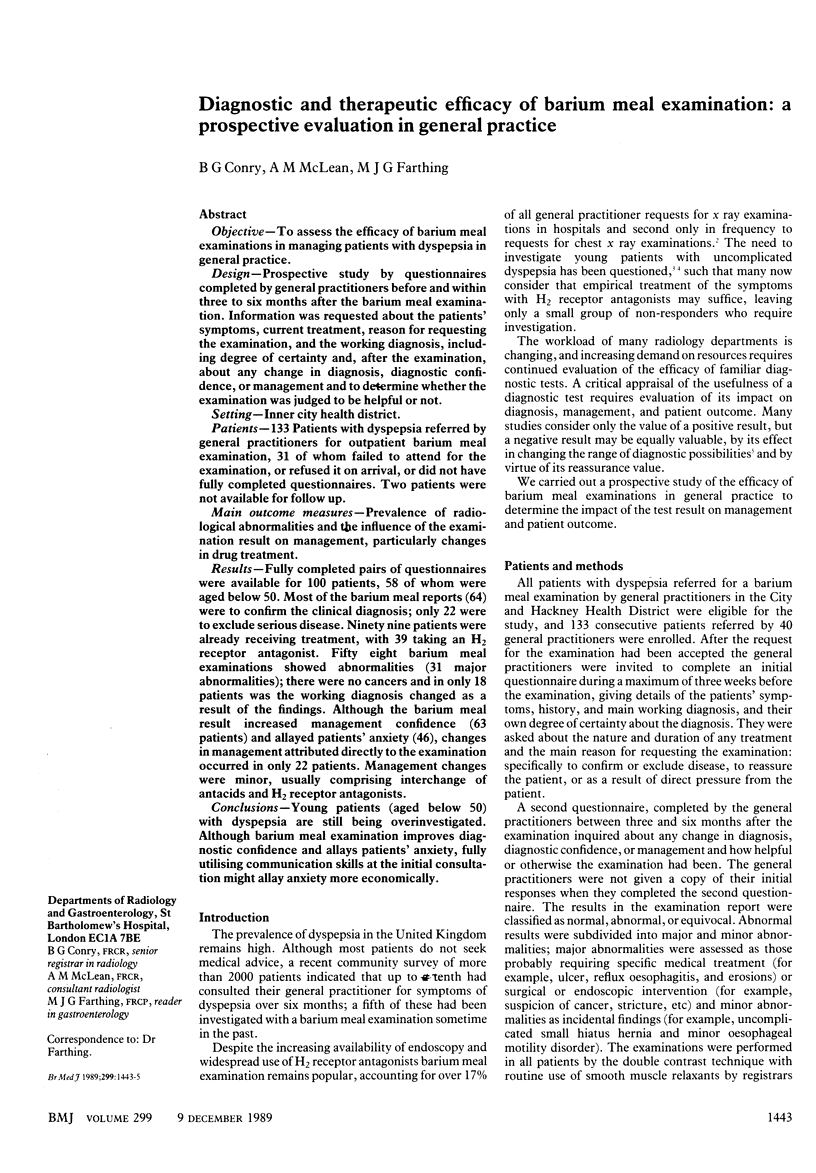

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Barton E., Gallagher S., Flower C. D., Hanka R., King R. H., Sherwood T. Influence on patient management of general practitioner direct access to radiological services. Br J Radiol. 1987 Sep;60(717):893–896. doi: 10.1259/0007-1285-60-717-893. [DOI] [PubMed] [Google Scholar]
- Chen Y. M., Ott D. J., Gelfand D. W., Munitz H. A. Impact of the barium enema on patient management. Gastrointest Radiol. 1988;13(1):81–84. doi: 10.1007/BF01889029. [DOI] [PubMed] [Google Scholar]
- Davenport P. M., Morgan A. G., Darnborough A., De Dombal F. T. Can preliminary screening of dyspeptic patients allow more effective use of investigational techniques? Br Med J (Clin Res Ed) 1985 Jan 19;290(6463):217–220. doi: 10.1136/bmj.290.6463.217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gelfand D. W., Ott D. J., Munitz H. A., Chen Y. M. Radiology and endoscopy: a radiologic viewpoint. Ann Intern Med. 1984 Oct;101(4):550–552. doi: 10.7326/0003-4819-101-4-550. [DOI] [PubMed] [Google Scholar]
- Gorry G. A., Pauker S. G., Schwartz W. B. The diagnostic importance of the normal finding. N Engl J Med. 1978 Mar 2;298(9):486–489. doi: 10.1056/NEJM197803022980904. [DOI] [PubMed] [Google Scholar]
- Guyer P. B., Chalmers A. G. Chest radiography for general practitioners--a low yield investigation. J R Coll Gen Pract. 1983 Aug;33(253):477–479. [PMC free article] [PubMed] [Google Scholar]
- Hayward M. W., Hayward C., Ennis W. P., Roberts C. J. A pilot evaluation of radiography of the acute abdomen. Clin Radiol. 1984 Jul;35(4):289–291. doi: 10.1016/s0009-9260(84)80096-3. [DOI] [PubMed] [Google Scholar]
- Jones R., Lydeard S. Prevalence of symptoms of dyspepsia in the community. BMJ. 1989 Jan 7;298(6665):30–32. doi: 10.1136/bmj.298.6665.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knapp H. R., Reilly I. A., Alessandrini P., FitzGerald G. A. In vivo indexes of platelet and vascular function during fish-oil administration in patients with atherosclerosis. N Engl J Med. 1986 Apr 10;314(15):937–942. doi: 10.1056/NEJM198604103141501. [DOI] [PubMed] [Google Scholar]
- Marton K. I., Sox H. C., Jr, Wasson J., Duisenberg C. E. The clinical value of the upper gastrointestinal tract roentgenogram series. Arch Intern Med. 1980 Feb;140(2):191–195. [PubMed] [Google Scholar]
- Mead G. M., Morris A., Webster G. K., Langman M. J. Uses of barium meal examination in dyspeptic patients under 50. Br Med J. 1977 Jun 4;1(6074):1460–1461. doi: 10.1136/bmj.1.6074.1460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams B., Luckas M., Ellingham J. H., Dain A., Wicks A. C. Do young patients with dyspepsia need investigation? Lancet. 1988 Dec 10;2(8624):1349–1351. doi: 10.1016/s0140-6736(88)90879-3. [DOI] [PubMed] [Google Scholar]


