Summary
Angiogenesis is a crucial process involved in numerous physiological and pathophysiological settings. During the past three decades, the field of tumour associated angiogenesis has been the focus of a plethora of basic research projects and clinical studies. Tumour associated neovessels satisfying the increased demand of oxygen and nutrients in malignant tumours are now emerging as specific targets for novel antineoplastic agents. This article discusses the present data on antiangiogenic treatment of human gastrointestinal malignancies, including gastric, pancreatic, and colorectal adenocarcinoma, and outlines potential future perspectives, such as development of surrogate markers of angiogenesis.
Process of tumour angiogenesis
Angiogenesis, the formation of new vessels from existing capillary beds, represents a central mechanism involved in many physiological and pathophysiological conditions, including embryonal development, wound healing, and chronic inflammation.1 In malignant tumours, angiogenesis represents a prerequisite for tumour growth, as the high metabolism of tumour cells requires large amounts of oxygen and nutrients. Without angiogenesis, the growth of malignant tumours is limited to 1–2 mm in diameter, which corresponds to the maximum distance oxygen can diffuse.2,3 Tumour vascularisation represents a conditio sine qua non for exponential tumour growth. Studies have indicated that the mitotic index of tumour cells decreases with increasing distance from the supplying microvessel.1,3,4 Primary tumours as well as their metastases are dependent on tumour associated microvessels to establish an independent blood supply.3,5 Enhanced vascularity allows tumours not only to expand in size but also facilitates haematogenous spreading by a higher probability of tumour angioinvasion. Once deposited in a distant organ, tumour metastases are dependent on building their own microvasculature.6 For this reason, disruption of angiogenesis pathways provides a therapeutic perspective in the treatment of primary malignant human tumours as well as their metastases.
The concept that metastases are solely dependent on newly formed blood vessels in order to grow is opposed by observations made by Vermeulen and colleagues.7 According to their findings, approximately one third of hepatic colon cancer metastases studied (n = 28) do not induce new vessels but rather use and preserve the existing abundant vascularisation of the liver parenchyma. This pattern, called “replacement pattern”, differs from the so‐called “desmoplastic” and “pushing”‐type of metastasis. In all three patterns of metastasis, overall vessel density was not significantly different. However, a much lower endothelial cell proliferation was encountered in the replacement‐type of metastasis. These findings suggest that not counting vessels, but rather evaluating endothelial cell (EC) proliferation, might be the appropriate way for assessing angiogenesis, depending on the type of metastasis.8
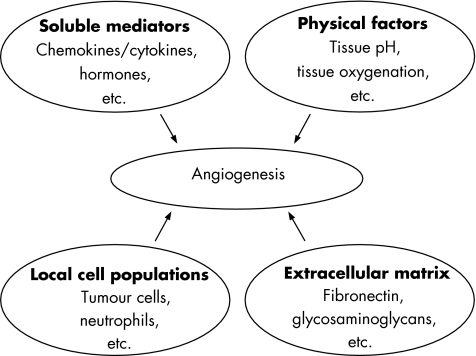
The concept of human tumours being capable of secreting angiogenic factors was first introduced by Dr Judah Folkman in the 1970s, who is widely regarded as a pioneer of angiogenesis research.9 Human microvascular angiogenesis is tightly controlled by a plethora of biochemical variables, including soluble factors (for example, cytokines, growth factors, enzymes modifying the extracellular matrix), as well as hypoxia and acidity (fig 1). Tumour angiogenesis is a mechanism by which the tumour responds to hypoxia and resistance to hypoxia may be attributed to overexpression of enzymes such as haemoxygenase‐1 10 and carbonic anhydrase.11 Angiogenic factors are produced by a multitude of physiological cell populations,12 including smooth muscle cells and pericytes,13 endothelial cells,14,15,16 and tumour cells, as well as epithelial cells from colorectal carcinoma.17
Figure 1 Factors controlling angiogenesis. The formation of new blood vessels from existing capillary beds is dependent on a multitude of physical, chemical, and biological factors. Soluble mediators, including vascular endothelial growth factor and other cytokines, as well as tissue pH and hypoxia, are important determinants regulating angiogenic activity. Likewise, both extracellular matrix and local cell populations have an impact on angiogenesis.
Vascular endothelial growth factor (VEGF) and many other angiogenic factors are endogenous ligands of receptors present on the EC surface, leading to initiation of intracellular signal transduction and gene transcription, eventually resulting in EC proliferation, active locomotion (chemotaxis), and degradation of the extracellular matrix (ECM) by secretion of proteases, including matrix metalloproteinases (MMP).18,19 However, MMP‐2, ‐7, ‐9, and ‐12 were also shown to counteract angiogenesis through generation of potent endogenous angiogenesis inhibitors, including angiostatin, by proteolytic cleavage of plasminogen and specific collagen chains found in the ECM.20
Angiogenesis is a prerequisite for the growth of solid tumours.
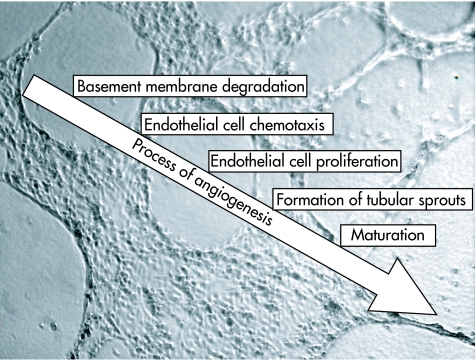
Following rearrangement of the EC, a primary immature vascular network is formed which is subsequently refined by vessel maturation and consolidation by adjacent supporting cells, including smooth muscle cells and pericytes (fig 2).21 Compared with physiological microvessels, tumour associated microvessels are fragile highly disorganised vessels of hetereogeneous diameters, which show less cellular support by scaffolding cells and extracellular matrices.22,23 In addition, tumour microvessels exhibit defect vasomotor functions, often lacking a predilected direction of blood flow.22 All of the above mentioned characteristics of tumour associated microvessels deserve consideration in the design of antiangiogenic strategies as disturbed blood flow and altered permeability potentially hamper effective drug delivery.24,25
Figure 2 Angiogenesis: a multistep sequence. The process of angiogenesis is a sequence of events, some of which occur simultaneously. Proteolysis of the basement membrane is followed by directed locomotion of endothelial cells (chemotaxis). Endothelial cells begin to proliferate, forming initial tube‐like structures (sprouting). The final event in this sequence is maturation of microvessels, which is supported by adjacent cells, including pericytes. Background picture: human intestinal microvascular endothelial cells forming tubular structures in an extracellular matrix (own observations).
Oncogenes and angiogenesis in solid tumours
Angiogenesis driven by solid tumours is believed to be dependent on genetic alterations that also account for features characteristic of malignant transformation, including resistance to apoptosis and deregulated mitogenesis. Genetic alterations responsible for the malignant behaviour of tumour cells include activation of various oncogenes, such as c‐myc and HER‐2, as well as inactivation or loss of tumour suppressor genes, including p53 and p16. Various oncogenes are known to be potent deregulators in the expression of angiogenic and angiostatic effector molecules by tumour cells. For example, activation of specific oncogenes (K‐ras, H‐ras, Her‐2, c‐fos, among others) is associated with enhanced expression of angiogenic mediators (for example, VEGF) by tumour cells. Likewise, these alterations are also involved in downregulation of important antiangiogenic mediators, such as thrombospondin. In addition to VEGF, activated ras oncogenes have also been implicated in the production of further angiogenic factors, including basic fibroblast growth factor (bFGF), transforming growth factor (TGF) family members, platelet derived growth factor (PDGF), insulin‐like growth factor (IGF)‐1, and others.26
Under physiological conditions, p53 gene product is maintained at low often undetectable protein levels owing to an extremely short half life. Under pathophysiological conditions, including DNA damage, activation of oncogenes, and hypoxia, p53 stabilisation occurs, which leads to higher levels of p53 expression.27 Likewise, overexpression of p53 in colorectal carcinoma cells was associated with high microvascular densities in adjacent tissue areas.28 Similar to these observations, a study by Liang et al reported that both K‐ras mutation and mutant p53 overexpression status were significantly correlated with microvascular density in 114 colorectal carcinoma specimens.29 Conflicting results were published in a study by Giatromanolaki et al where no correlation between p53 expression and the degree of tumour vascularity was observed in 106 colorectal cancer specimens.30 These findings were supported by Aotake et al, who were unable to describe an association between p53 activation status and extent of angiogenesis in colorectal carcinoma.31 Similar observations have been published for gastric32 and pancreatic adenocarcinoma (tables 1–3).33
Table 1 Expression of angiogenic factors in colorectal carcinoma: association with clinical features.
| Factor | No of patients | Association | Reference |
|---|---|---|---|
| VEGF | |||
| 52 | +MVD, +metastasis, +proliferation index | Takahashi64 | |
| 100 | +MVD, +Dukes grade | Nakasaki66 | |
| 152 | −Differentiation, +lymphatic metastasis, | ||
| +hepatic metastasis, +advanced stage | Ochiumi94 | ||
| 163 | +MVD, −prognosis, +hepatic metastasis | Kang197 | |
| 136 | +MVD, −prognosis, +TP expression | Amaya198 | |
| 100 | +MVD, −prognosis, +hepatic metastasis | Maeda199 | |
| 121 | +Recurrence rate | Cascinu200 | |
| 259 | +MVD, +liver metastasis, −mean survival | Harada201 | |
| 152 | −Mean survival | Kaio202 | |
| PD‐ECGF | |||
| (thymidine phosphorylase) | 163 | +MVD, +tumour size, +advanced stage, | Takebayashi 203 |
| +lymphatic metastasis, −prognosis | |||
| 86 | −Lymphatic/haematogenous metastasis | Saito204 | |
| 32 | −Mean survival | van Triest205 | |
| 148 | −Prognosis | Matsumura206 | |
| HIF | |||
| 149 | +MVD, +advanced stage, +hepatic metastasis, | ||
| +VEGF expression | Kuwai101 | ||
| 87 | +MVD, −mean survival, +COX‐2 expression | Yoshimura102 |
VEGF, vascular endothelial growth factor; PD‐ECGF, platelet derived endothelial cell growth factor; HIF, hypoxia inducible factor; MVD, microvascular density.
NS, no significant correlation; +, positively correlated; −, inversely correlated.
Table 2 Expression of angiogenic factors in gastric adenocarcinoma: association with clinical features.
| Factor | No of patients | Association | Reference |
|---|---|---|---|
| VEGF | |||
| 163 | +MVD, NS mean survival, +differentiation | Tanigawa207 | |
| 195 | +Disease recurrence | Maeda67 | |
| 102 | +Hepatic metastasis, ‐prognosis | Kimura208 | |
| 91 | (VEGF‐D): −prognosis | Juttner209 | |
| 120 | −Prognosis | Maeda210 | |
| PD‐ECGF | |||
| (thymidine phosphorylase) | 158 | +MVD, +Size, +lymphatic metastasis, −prognosis | Takebayashi211 |
| 120 | +MVD, +hepatic metastasis | Maeda212 | |
| 33 | (Tissue activity): + venous invasion | Nakata213 | |
| 126 | +Response to 5‐FU chemotherapy, +prognosis | Saito214 | |
| 148 | +MVD, −prognosis, +proliferation index | Kikuyama215 | |
| 102 | +Hepatic metastasis, −prognosis | Kimura208 | |
| 116 | −Prognosis, +proliferation index | Konno216 | |
| 116 | +Haematogenous metastasis, +recurrence | Konno217 | |
| Ang‐2 | |||
| 85 | +Advanced disease, −mean survival | Etoh93 | |
| 72 | +VEGF expression, +advanced disease | Sun218 |
VEGF, vascular endothelial growth factor; PD‐ECGF, platelet derived endothelial cell growth factor; Ang‐2, angiopoietin 2; MVD, microvascular density; 5‐FU, 5‐fluorouracil.
NS, no significant correlation; +, positively correlated; −, inversely correlated.
Table 3 Expression of angiogenic factors in pancreatic adenocarcinoma: association with clinical features.
| Factor | No of patients | Association | Reference |
|---|---|---|---|
| VEGF | |||
| 22 | NS MVD, NS mean survival, NS recurrence | Ellis219 | |
| 40 | +MVD, −mean survival, +MVD | Ikeda70 | |
| 70 | +MVD, +recurrence, −mean survival | Niedergethmann220 | |
| 55 | +MVD, −mean survival | Kuwahara79 | |
| 124 | +MVD | Khorana221 | |
| 50 | +MVD, −mean survival | Couvelard105 | |
| FGF | |||
| 55 | NS MVD, −mean survival | Kuwahara79 | |
| 104 | +MVD, +hepatic metastasis, +recurrence | Fujioka222 | |
| 20 | +Proliferation index | Yamazaki223 | |
| PD‐ECGF | |||
| (thymidine phosphorylase) | 104 | +MVD, −mean survival, +recurrence, +hepatic metastasis | Fujioka222 |
| 50 | +MVD, −mean survival | Fujimoto69 | |
| 40 | −Mean survival | Ikeda70 | |
| 55 | NS MVD, NS mean survival | Kuwahara79 | |
| 124 | NS MVD | Khorana221 | |
| HIF | |||
| 49 | +MVD, +tumour size, +advanced stage, +proliferation index | Kitada224 | |
| 55 | +MVD, +metastasis, +VEGF expression, | ||
| −prognosis | Shibaji104 | ||
| 50 | +MVD | Couvelard105 |
VEGF, vascular endothelial growth factor; PD‐ECGF, platelet derived endothelial cell growth factor; HIF, hypoxia inducible factor; MVD, microvascular density.
NS, no significant correlation; +, positively correlated; −, inversely correlated.
Tumour associated angiogenesis depends on a plethora of biochemical and physical determinants, including growth factors, tissue pH, and tissue oxygenation.
Activation of oncogenes or loss of tumour suppressor genes is often associated with expression of angiogenic factors by tumour cells.
A study addressing the question of whether oncogene activation or p53 status could be associated with the clinical response to antiangiogenic therapy was published recently. In a series of 295 patients, the expression status of the oncogenes k‐ras and b‐raf, as well as of the tumour suppressor gene p53 in colorectal cancer specimens did not correlate with the clinical response status to antiangiogenic therapy targeting VEGF (bevacizumab/Avastin).34 Therefore, the relevance of these specific genetic alterations with respect to antiangiogenic therapy in human colorectal carcinoma remains unclear.
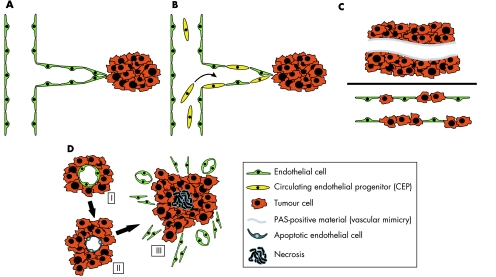
1.2. Angiogenesis independent tumour vascularisation
Alternative mechanisms by which microvascular endothelial cells may support growth of solid tumours include vasculogenesis, vascular co‐option, vessel mosaicism, and vascular mimicry (fig 3).35 The term postnatal vasculogenesis refers to a mechanism by which endothelial precursor cells derived from bone marrow incorporate into and contribute to physiological and pathological angiogenesis.36 Accordingly, in contrast with angiogenesis, blood vessels will be newly formed and not be derived from existing microvessels. It has been hypothesised that solid tumours secreting VEGF, including colorectal carcinoma, might be able to recruit endothelial progenitor cells from bone marrow to initiate vasculogenesis.37
Figure 3 Mechanisms of tumour vascularisation. (A) Classical angiogenesis has widely been described as the formation of new blood vessels from existing capillary beds. Endothelial cells stimulated by angiogenic mediators start to proliferate, forming directed microvessels. (B) Vasculogenesis by recruitment of circulating endothelial progenitor cells (CEP) has been proposed as an additional mechanism of neoangiogenesis. Circulating CEP settle and differentiate into endothelial cells to establish new microvessels. (C) Vascular mimicry (upper panel) describes small perfused channels forming within clusters of tumour cells. Typically, these functional channels are lined with periodic acid‐Schiff (PAS) positive material. The term vessel mosaicism (lower panel) refers to microvessels where the continuous endothelial layer is interrupted by interspersed tumour cells. (D) The term vascular co‐option refers to a mechanism by which tumour cells surround supporting microvessels (I), causing endothelial cell apoptosis. Subsequent hypoxia leads to upregulation of angiogenic mediators by tumour cells, which results in strong angiogenesis, mainly at the tumour periphery (III). Modified from Auguste and colleagues.35
Vascular co‐option, recruitment of pre‐existent vessels by tumours, was first described by Holash and colleagues in 1999.38 This mechanism was initially observed in experimental gliomas, which arise in one of the most densely vascularised organs, the brain. Contrary to the view that angiogenesis is an immediate tissue response required for initial tumour growth, these tumours were shown to initially induce apoptotic vessel regression, resulting in a secondary avascular tumour. In later stages, a robust proangiogenic response at the tumour margin is observed, resulting in tumour rescue.38 Correspondingly, tumours arising in densely vascularised organs will initially be able to grow without the need of an angiogenic switch to take place. Therefore, this initial form of blood supply will not be affected by angiogenesis inhibition.39
Alternative mechanisms of tumour vascularisation include vasculogenesis, vascular mimicry, vessel mosaicism, and vascular co‐option.
In recent years, it has been hypothesised that tumour cells themselves are able to participate in the formation of functional vessel‐like channels. Vascular mosaicism, a mechanism whereby the tumour cells themselves line the vessels, was reported to occur in up to 15% of vessels in a colonic carcinoma implantation model.40
The concept of vasculogenic mimicry was first described for aggressive uveal melanoma described by Maniotis et al. This tumour was shown to contain a network of channels interconnected by loops. Transmission electron microscopy indicated that the channels are lined by a basal lamina‐like layer. Inside the channel lumen, red blood cells are observed. Functional assays have indicated that these channels might contribute to tumour perfusion, as shown by experimental perfusion using fluorescent dyes.41
All of the aforementioned alternative vascularisation models might have important consequences for the development of antiangiogenesis agents in human gastrointestinal tumours, but clinical data are lacking to date.
Recent research has focused mainly on inhibition of single prominent proangiogenic factors and selected pathways. This review reports on a selection of established and well recognised proangiogenic factors, although many more are currently under intensive scientific and clinical investigation.
Angiogenesis research: animal models versus human primary cell culture
Most of what is known about angiogenesis is derived from research on animals (for example, tumour implantation models using immunocompromised SCID mice injected with human colon cancer cells). The large gap between rodent vascular biology and human disease is one major point of criticism in the assessment of clinical antiangiogenesis studies. Many therapeutic strategies obtained from rodent angiogenesis models have proved disappointing in the treatment of human disease.42,43 This is most likely caused by the marked differences in human and rodent vascular biology, as well as by endothelial heterogeneity in human in vitro EC models.44 Consequently, clinical angiogenesis research demands simulation of human intestinal vascular pathology in vitro to obtain results resembling human in vivo vascular characteristics.
In 2000, St Croix and colleagues published a study on specific gene transcription patterns of EC isolated from human colorectal tumours compared with EC from human normal colonic mucosa. Using this approach, 79 genes were differentially expressed, including 46 that were selectively upregulated in tumour associated EC. Some of the detected genes encode ECM proteins but the majority of genes are of unknown function.45
With primary cultures of human intestinal microvascular EC in vitro,46 experiments can be performed resembling the in vivo features of the human intestinal microvasculature as closely as possible.
Multiple experimental approaches to quantify and characterise angiogenesis have been tested and reported. Angiogenesis, a multistep process of interdigitating cellular activities, is composed of cellular locomotion, as assessed by stress fibre assembly and chemotaxis assays, as well as proliferative responses, which can be measured in vitro by cellular uptake of tritiated thymidine (3H‐thymidine, reflecting DNA synthesis) or catalysation of methylthiazolyldiphenyl‐tetrazolium bromide oxidation (reflecting mitochondrial metabolism).47 In addition, a recent investigation has shown evidence for a role of directed apoptosis in the formation of new blood vessels.48 Direct readouts for in vitro angiogenesis are provided using a three dimensional extracellular matrix (Matrigel) enabling cultured EC to form tube‐like structures. In vivo angiogenesis assays are represented mainly by subcutaneous implantation of cast Matrigel plugs and post mortem histological analysis or the chicken chorioallantoic membrane assay.49
Angiogenic factors
Vascular endothelial growth factor (VEGF)
VEGF is regarded as one of the most important angiogenic factors in health as well as in disease. The VEGF family is comprised of six molecules termed VEGF‐A, B, C, D, and E, and placenta growth factor.50 VEGF‐A exists in five isoforms (121, 145, 165, 189, and 205 amino acids),51 the largest two of which are membrane bound. VEGF family members act on EC via VEGF receptors expressed on the EC surface, inducing EC proliferation, synthesis of proteolytic enzymes,52,53 and chemotaxis.54 Further effects of VEGF‐A include antiapoptotic functions, as well as vasodilatation55 and potent escalation of vascular permeability, allowing for plasma proteins to diffuse into the perivascular interstitium to constitute a reticular network along which EC migrate to form premature vessels.56 EC stimulation with VEGF also results in secretion of proteases involved in extracellular matrix degradation, a mechanism required for angiogenesis. VEGF‐A (165) seems to be the most predominant isoform secreted by human tumours.57 Factors modulating VEGF expression were shown to include decreasing tissue pH, hypoxia, and various growth factors, among others.58 Activation of all three characterised VEGF receptors (VEGFR‐1 (flt‐1), ‐2 (kdr/flk‐1), ‐3 (flt‐4)) expressed on the surface of EC and some tumour cell populations results in intracellular tyrosine kinase activity, mediating a potent mitogenic stimulus.59,60 More specifically, VEGFR‐1 was found to communicate EC migration, while stimulation of VEGFR‐2 leads to an increase in vascular permeability and EC proliferation.61
Expression of VEGF‐A is highly upregulated in human colorectal adenocarcinoma,62 and high expression of this cytokine has been linked to poor prognosis and a high propensity of metastatic spreading in these patients.63,64 Additional evidence for a pivotal role of VEGF‐A in angiogenesis of colorectal adenocarcinoma comes from observations indicating increasing expression from non‐neoplastic to malignant colonic mucosa.65 Additionally, microscopic vessel counts were found to tightly correlate with tumour expression of VEGF in colorectal adenocarcinoma.66 Further study results suggest that VEGF expression levels and vessel counts may be used as prognostic markers for recurrence and metastasis in colon cancer patients.64 Similar observations have been made for expression of VEGF‐A in gastric67,68 and pancreatic adenocarcinoma.69,70
Fibroblast growth factors
Fibroblast growth factors (FGFs) constitute a large family with no less than 20 related molecules with a wide spectrum of biological functions, some of them exerting potent induction of angiogenesis in vitro and in in vivo models. Among these, the acidic FGF (aFGF, FGF‐1) and basic FGF (bFGF, FGF‐2) have been investigated most profoundly. As known for VEGF family members, the cellular activities of FGF are mediated by FGF receptor (FGFR1–4) associated intracellular tyrosine kinase activity. In correspondence to what is known about the biological functions of VEGF, FGFs were found to be potent inducers of EC proliferation and migration, as well as EC tubulogenesis.71,72 Numerous additional functions of the FGF family have been associated with tissue repair and tumour progression. Interestingly, FGF‐2 concentrations were found to be elevated in the urine of patients suffering from various malignancies.73,74 In colorectal cancer, bFGF plasma levels were shown to correspond to advanced tumour stages, as well as resistance of tumours to chemotherapy.75,76,77 Only limited data are available regarding expression of FGFs in gastric and pancreatic carcinoma. Initial results obtained by Tanimoto et al have indicated elevated expression of bFGF mRNA in 55% of gastric carcinoma tissues compared with control tissue.78 In pancreatic carcinoma, immunostaining results have shown that FGF‐2 was detectable in 60.9% of tumour specimens. Furthermore, high expression levels of FGF‐2 were significantly associated with shorter survival times in these patients.79
Platelet derived endothelial cell growth factor
Platelet derived endothelial cell growth factor (PD‐ECGF) is a thymidine phosphorylase acting as a powerful chemoattractant on EC,80 which exerts marked angiogenic responses in rodent tumour models.81 In addition to its functions as a secreted growth factor, PD‐ECGF is involved intracellularly in the metabolism of pyrimidine nucleosides and 5‐fluorouracil.82 Expression of PD‐ECGF has been shown in tumour cells, stromal cells, and infiltrating mononuclear cells.83 It has been hypothesised that human colorectal tumours showing low VEGF expression are more dependent on PD‐ECGF as the major proangiogenic factor.83 As for VEGF‐A, expression of PD‐ECGF by tumours has been linked to poor prognosis in pancreatic70 and gastric84 cancer. Recent studies have suggested that tumour PD‐ECGF expression might serve as a prognostic marker for the outcome and response to chemotherapy in patients with colorectal cancer,85,86 especially when assessed at the edge of the invading tumour.87
Angiopoietins
The angiopoietins Ang‐1, ‐2, ‐3, and ‐4 are agonistic ligands of the Tie‐2 tyrosine kinase receptor generally expressed on EC surfaces.88 The Tie‐2 receptor is activated by Ang‐1 and Ang‐4 while Ang‐2 and ‐3 were shown to counteract Ang‐1 induced Tie‐2 activation.88,89 The angiopoietin effects therefore result from the finely tuned balance of Ang‐1 to ‐4 family members. Interestingly, the effects of Ang‐2 seem to be tightly dependent on the concomitant presence of the major angiogenic factor VEGF. In the absence of VEGF, Ang‐2 was shown to induce vessel regression whereas in the presence of VEGF, Ang‐2 is believed to support the angiogenic response of the microvessel.89 Ang‐2 is commonly overexpressed in colorectal adenocarcinoma while Ang‐1 was rarely found to be expressed.90,91 In addition, colon cancer cells stably transfected to overexpress Ang‐2 and implanted into immunocompromised mice displayed markedly enhanced growth kinetics compared with untransfected control cells.92 A high tumour expression of Ang‐2 was correlated with advanced tumour stages and shorter survival in gastric93 and colorectal94,95 cancer patients. In addition, Ang‐2 expression was found to be markedly elevated in pancreatic carcinoma tissue samples,96 but data on its impact on the outcome and prognosis are lacking.
Hypoxia inducible factor 1
Hypoxia inducible factor (HIF) 1 is known to play a central role in tissue responses to hypoxia. HIF‐1 is a heterodimeric protein consisting of two subunits called HIF‐1α and 1β. Under normoxic conditions, HIF‐1α is rapidly degraded in a proteasome dependent pathway. In human tumour cells, HIF‐1α degradation was shown to be tightly dependent on the activation status of the tumour suppressor gene, p53. Anoxic conditions were reported to maximise p53 activation, which leads to an increase in HIF‐1α degradation.27 In hypoxia, however, HIF‐1α degradation is markedly diminished, resulting in the formation of stable HIF‐1 heterodimers and eventually leading to activation of specific genes whose products act to increase the oxygen concentration in the tissue (for example, VEGF and haeme oxygenase, among others).97 Additionally, hypoxia independent upregulation of HIF‐1 was described, occurring as a downstream event of growth factor signalling (for example, epidermal growth factor receptor activation).98
In in vitro models using colorectal carcinoma cells, expression of HIF‐1 was linked to increased tumour vascularisation and higher invasiveness.99 Data from a study using human gastric cancer cells implanted in mice have indicated that inhibition of HIF‐1α leads to a reduction in tumour associated angiogenesis and vessel maturation, accompanied by impairment of tumour growth.100 Overexpression of HIF‐1 in human colorectal adenocarcinoma has been demonstrated to correlate with tumour VEGF expression and advanced tumour stages.101,102 Recent data have shown that tissue expression of HIF‐1 in colorectal cancer specimens appears to be linked to that of lactate dehydrogenase, isoform 5, a response marker for tissue hypoxia and anaerobic glycolysis. Both of the above factors were shown to be associated with an aggressive cancer phenotype in patients with colorectal adenocarcinoma.103 In pancreatic adenocarcinoma, expression of HIF‐1α was shown to correlate with histological markers of angiogenesis and prognosis.104,105
Angiogenic chemokines
Chemokines are small (8–12 kDa) secreted proteins serving a wide array of receptor dependent immune functions.106 Chemokines displaying the ELR (Glu‐Leu‐Arg) amino acid motif (ELR+ chemokines) have been shown to have direct angiogenic effects on human EC in vitro and in vivo, with interleukin 8 (IL‐8) being the most extensively studied angiogenic chemokine.107 IL‐8 (also termed CXCL8) shows constitutive and regulated expression in a broad range of cells, including tumour infiltrating mononuclear cells, several human tumour cell lines, and EC. Proinflammatory regulation of IL‐8 is mediated by the transcription factor nuclear factor κB.108,109,110 IL‐8 exerts its biological activities on effector cells in a paracrine and autocrine fashion. The cellular effects of IL‐8 are mediated by ligation of its cognate receptors, CXCR1 and CXCR2 expressed on target cells, including human EC.111 The chemokine receptor CXCR2 promiscuously binds all known members of the angiogenic ELR+ CXC chemokine family, including IL‐8, the growth regulated oncogene family members (GRO‐α, ‐β, and ‐γ), NAP‐2, GCP‐2, and ENA‐78 with high affinity. In contrast, CXCR1 specifically binds only IL‐8 and GCP‐2. Initially identified as a major proinflammatory cytokine in various inflammatory disorders, there is growing evidence that IL‐8 exerts potent angiogenic effects in human malignant tumours, including colorectal adenocarcinoma. In addition to its direct action on endothelial cells, in vitro angiogenesis induced by exogenous IL‐8 was frequently accompanied by inflammatory bystander cells, pointing towards additional angiogenic mechanisms by IL‐8‐mediated release of secondary angiogenic mediators.112 Malignant colonic epithelial cells derived from colorectal adenocarcinoma are known to secrete IL‐8 in a regulated fashion in vitro.108 Strategies blocking the angiogenic activity of IL‐8 have proven to be effective in inhibiting angiogenesis in human tumours in murine models.113,114 Notably, IL‐8 is highly expressed in hyperplastic mucosa adjacent to colon cancer, supporting an indirect angiogenic effect of colon cancer cells.115 In addition, IL‐8 seems to be involved in the development of distant metastases from colorectal cancer.116 Data from our group have indicated that primary human intestinal microvascular endothelial cells derived from human gut exclusively express CXCR2, whereas CXCR1 does not appear to be expressed.117 For this reason, human intestinal microvascular endothelial cells appear to be responsive to an array of angiogenic chemokines.
In human gastric cancer models, malignant gastric epithelial cells stably transfected to overexpress IL‐8 show increased angiogenesis and tumorigenesis in nude mice.118 Similar experimental observations were made in human pancreatic adenocarcinoma cells orthotopically transplanted into nude mice.119
An additional potential CXC chemokine receptor expressed on colonic microvascular endothelial cells is the Duffy antigen receptor for chemokines (DARC). DARC has been shown to non‐selectively bind various angiogenic ELR+ CXC chemokines, including IL‐8.120 Although DARC is highly expressed on human colonic mucosal microvessels (Heidemann, unpublished data), its signalling properties are unclear as it apparently does not couple to G proteins, and binding of chemokines to DARC does not evoke any intracellular signal in vitro.121,122 It has been suggested that DARC might act as a decoy and scavenger receptor binding excess chemokines, potentially sustaining chemokine action in a buffering fashion.123 To date, expression of DARC in tumour microvessels and its role in chemokine driven angiogenesis remains unclear.
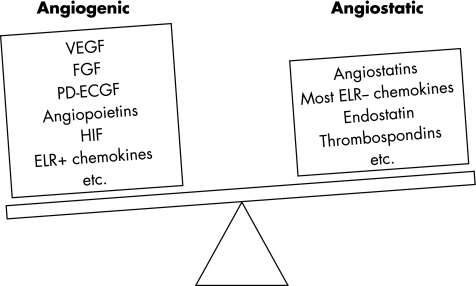
Other angiogenic factors
A multitude of additional secreted mediator molecules have been proven to have an impact on in vitro and in vivo angiogenic EC responses. In many cases, the underlying mechanisms of action are mediated by direct effects on EC, as for interferons α, β, γ, TGF‐α and β, tumour necrosis factor α (TNF‐α), thrombospondin, and many more (fig 4).111 Alternatively, growth factors indirectly act on EC by secondary modulation of VEGF expression, as has been shown for various angiogenic mediators, including hepatocyte growth factor,124 epidermal growth factor,125 IGF‐1,126 IL‐1 family members,127 PDGF, TGF‐β1,128 and prostaglandin E2,129 the production of which is tightly dependent on cyclooxygenase (COX)‐2 activity, a key enzyme in mucosal microvascular homeostasis.130,131
Figure 4 Endogenous factors regulate angiogenesis. The extent of angiogenesis is controlled by the net balance of local endogenous angiogenic and angiostatic factors. An increase in angiogenic factors, as well as a decrease in angiostatic factors, will result in activated angiogenesis. VEGF, vascular endothelial growth factor; FGF, fibroblast growth factor; PD‐ECGF, platelet derived endothelial cell growth factor; HIF, hypoxia inducible factor.
Antiangiogenic therapy
Several antiangiogenic therapy concepts have resulted in preclinical models as well as clinical trials in human colorectal cancer disease. Clinical phase I and II trials of single antiangiogenic agents in human disease have been cancelled due to lack of efficacy. This is in part explainable by the fact that data obtained from rodent angiogenesis models are not translatable into hypotheses on human gastrointestinal angiogenesis without restriction. Compared with human vascular biology, rodent models feature a different set of angiogenic factors fine tuning the balance of microvessel growth and regression. Because of that, only a fraction of clinical trials in human disease can feasibly mimic the effectiveness of preclinical animal experiments. Angiogenesis in both rodents and humans is dependent on a multitude of biological and physical factors, which emphasises that effective antiangiogenic therapy regimens will have to address multiple mechanisms of antiangiogenesis.
The fact that it is quite difficult to determine whether the drug is really hitting the target molecule might be another explanation for the lack of efficacy demonstrated in several antiangiogenesis trials. Therefore, clinical antiangiogenesis trials should be designed in order to verify the direct effects on local endothelial cells (for example, by obtaining sequential biopsies of the tumour). In addition, many studies to date have recruited unselected patient populations. With respect to the above mentioned “replacement pattern” of metastasis, it can be speculated that antiangiogenic compounds will be ineffective owing to the low fraction of proliferating EC in this patient subset. Both of the above problems should be considered in the design of clinical antiangiogenesis trials.
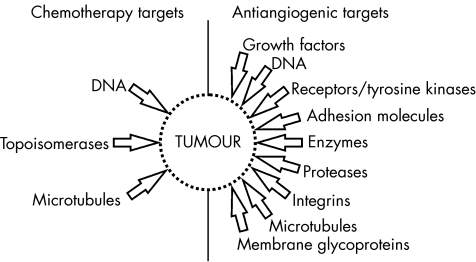
It has been shown that effective antiangiogenic therapy leads to an increase in apoptosis in tumour cells, while tumour cell proliferation itself remains widely unaffected. This balance of proliferative and apoptotic cell fractions is believed to constitute what is clinically referred to as tumour dormancy.132 The multitude of angiogenic effector molecules brings about many potential escape mechanisms. On the other hand, these factors offer an abundance of potential targets for antiangiogenic therapy compared with conventional cytotoxic chemotherapy (fig 5). Therefore, combinations of multiple antiangiogenic agents with established cytotoxic chemotherapy regimens will likely emerge in future antiangiogenesis trials. As VEGF is regarded as the most prominent proangiogenic factor in human colorectal cancer, many of the therapeutic approaches are focusing on interruption of the biological activity of VEGF by means of neutralising circulating VEGF, competitive binding to its receptors, or inhibition of VEGF associated intracellular proangiogenic signalling cascades, including VEGFR associated tyrosine kinases.133
Figure 5 Diversity of targets in conventional chemotherapy and antiangiogenic therapy of human tumours. The multitude of potential antiangiogenic cellular targets permits more diverse mechanisms of action compared with conventional chemotherapy of tumours. Modified from Kerbel and colleagues.196
Neutralisation of VEGF biological activity
Bevacizumab (Avastin; Genentech, South San Francisco, USA) is a neutralising recombinant humanised monoclonal antibody against human VEGF that has completed phase III clinical trials and has obtained FDA approval for firstline treatment in combination with intravenous 5‐fluorouracil (5‐FU) based chemotherapy in February 2004. In a study conducted by Hurwitz et al, a total of 813 naive patients with metastatic colorectal cancer were randomly assigned to conventional intravenous IFL (irinotecan/5‐FU/leucovorin) chemotherapy versus IFL plus bevacizumab. The results were indicative of a significantly prolonged total survival (20.3 v 15.6 months; p<0.001), progression free survival (10.6 v 6.2 months; p<0.001), and higher response rates in the bevacizumab group (44.8% v 34.8%; p = 0.004), respectively.134 Recent data obtained from a phase II study indicate that addition of bevacizumab to chemotherapy regimens containing bolus 5‐FU/leucovorin in patients who did not qualify for irinotecan based chemotherapy results in significant patient benefit, including prolonged progression free survival.135 Consequently, bevacizumab in combination with a 5‐FU based chemotherapy regimen has recently been approved in the USA and several European countries for firstline treatment of metastasised colorectal adenocarcinoma. The predominant side effects of bevacizumab are likely explained by direct effects on vascular homeostasis, including arterial thromboembolic events, gastrointestinal perforations, and impairment of wound healing, along with hypertension, proteinuria, and epistaxis.136 In human rectal cancer, bevacizumab therapy is directly correlated with a decrease in tumour perfusion, microvascular density, and vascular volume, as well as with an increase in the fraction of vessels with pericyte coverage in rectal carcinoma patients, as assessed by pre‐ and post‐treatment tumour tissue analysis.137
Further research projects are currently focusing on VEGF‐Trap, a potent antiangiogenic soluble recombinant decoy protein constructed from VEGFR1 and VEGFR2 binding domains fused to a human immunoglobulin G1 constant region peptide.138 Its biological affinity for VEGF is reported to be significantly higher than that of bevacizumab.139 In preclinical rodent models, VEGF‐Trap was shown to possess potent antiangiogenic efficacy140,141,142 and is currently being studied in phase I clinical trials in patients with advanced stage solid malignancies, including colorectal adenocarcinoma. IMC‐1C11, a chimeric antiVEGFR2/KDR antibody, is a further biological designed to block VEGF induced angiogenesis in human tumours. However, clinical testing of this antibody has not been completed.143
Small molecule compounds: inhibitors of tyrosine kinases and matrix metalloproteinases
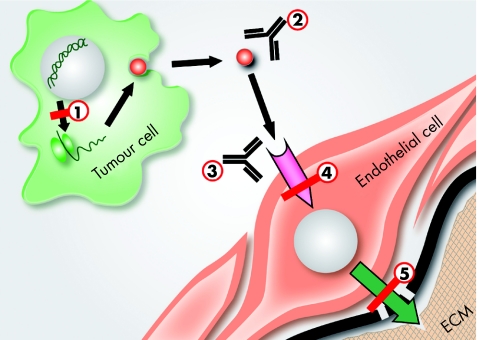
Inhibition of angiogenesis has been the focus of many commercial research groups worldwide. Novel therapeutic agents lacking the severe side effects of conventional cytotoxic chemotherapy represent a welcome addition to established therapy regimens. Many antiangiogenic molecular compounds are currently under intensive investigation, most acting on receptor associated intracellular tyrosine kinase activities as one of the possible molecular targets (fig 6). Novel compounds showing favourable preclinical data were however lacking clinical efficacy in many cases. For example, SU5416 (Semaxanib), a potent and selective inhibitor of VEGFR2 tyrosine kinase activity, has failed to show efficacy in the treatment of human advanced colorectal cancer.144,145 Additional phase III failures were observed for antiangiogenic MMP inhibitors (BB2516 (Marimastat), AG3340, Bay‐12‐9566)146 in the treatment of various human solid tumours, including pancreatic adenocarcinoma. Another potent angiogenesis inhibitor, SU6668, a chemical compound acting on a variety of tyrosine kinase activities associated with VEGF, PD‐ECGF, and FGF receptor activation, has undergone preclinical assessment and early clinical studies. Due to dose related toxicity, SU6668 had to be withdrawn from further testing.147
Figure 6 Subcellular localisation of antiangiogenic target molecules. The process of tumour associated angiogenesis can potentially be interrupted at various stages in the multistep sequence of tumour associated microvascular angiogenesis. (1) Some tumour cells show enhanced transcription of angiogenic mediators (red dot) (for example, vascular endothelial growth factor (VEGF)). Chemically stabilised phosphorothioate antisense oligonucleotides can be used to interfere with the transcription of angiogenic mediators. (2) Angiogenic mediators can be biologically bound by immunoreactive antibodies (for example, neutralising anti‐VEGF antibodies) or other neutralising peptides (for example, VEGF‐Trap). (3) Similarly, endothelial cell associated receptors specific for the angiogenic mediator (for example, VEGFR2) can be blocked by specifically designed antibodies eliciting competitive binding. (4) Receptor associated angiogenic signalling is often mediated by tyrosine kinases coupled to the angiogenic receptor (for example, VEGFR2 associated tyrosine kinases). Chemical compounds engineered to interfere with the enzymatic activity of these kinases (for example, Vatalanib) can specifically inhibit cytokine mediated endothelial activation. (5) Activated endothelial cells secrete proteases that potently disintegrate the endothelium associated basal lamina (black bold line) and the underlying extracellular matrix (ECM). Chemical compounds designed to block these enzymatic activities (for example, matrix metalloproteinase inhibitors) inhibit this last step in the sequence of tumour associated microvascular angiogenesis.
Further tyrosine kinase inhibitors include PTK787/ZK222584 (Vatalanib) and PKI 166, both of which have been shown to be effective in preclinical angiogenesis models in gastrointestinal tumours. PTK787/ZK222584 is currently being evaluated in phase II clinical trials in the treatment of gastrointestinal tumours, showing favourable data towards a biological response in tumour patients, along with a low occurrence rate of side effects.148,149
Additional VEGF‐tyrosine kinase inhibiting small molecules are under clinical investigation as potential antiangiogenic compounds in various human solid tumours, including ZD6474 and AZD2171.150 Other agents potentially effective in the antiangiogenic treatment of human colorectal cancer include BAY 43‐9006 (Sorafenib),151 a novel signal transduction inhibitor designed to disrupt angiogenesis through inhibition of the Raf/MEK/ERK pathway, and VEGFR2 associated tyrosine kinase activities, as well as SU‐11248 (Sunitinib), an orally active inhibitor of multiple angiogenic tyrosine kinase signalling pathways.152 All of the latter have undergone early clinical studies in the treatment of gastrointestinal cancer. Current studies actively recruiting gastrointestinal cancer patients are shown in table 4.
Table 4 Antiangiogenic small molecule compounds in gastrointestinal solid tumours: active studies.
| Compound/trial characteristics | Trial identifier |
|---|---|
| PTK787/ZK222584 (Vatalanib)/multiple receptor associated tyrosine kinases | |
| Phase II, advanced pancreatic cancer, open label | NCT00226005 |
| Phase II, metastatic solid tumours, open label | NCT00171587 |
| AG‐013736/multiple receptor associated tyrosine kinases | |
| Phase II, advanced pancreatic cancer, versus gemcitabine monotherapy | NCT00219557 |
| AZD2171/VEGFR‐2 associated tyrosine kinases | |
| Phase I, stage IV colorectal cancer, versus conv. chemotherapy | NCT00107250 |
| Phase II, colorectal cancer, versus conv. chemotherapy + bevacizumab | NCT00278889 |
| BAY 43‐9006 (Sorafenib)/raf protein kinases | |
| Phase II, stage III and IV colorectal cancer, versus cetuximab/irinotecan | NCT00134069 |
| XL999/multiple receptor associated tyrosine kinases | |
| Phase II, metastatic colorectal cancer, open label | NCT00277303 |
Bevacizumab, in adjunct with conventional chemotherapy, has proven to be effective in the first‐line treatment of metastasized colorectal carcinoma.
Other antiangiogenic treatment strategies
Future antiangiogenic approaches potentially include the use of stable nuclease resistant phosphorothioate antisense oligonucleotides aiming to reduce expression levels of tumour associated proangiogenic targets, including VEGFR‐mRNA. Inhibition of VEGFR‐mRNA was effective in reducing the peritoneal dissemination of experimental gastric cancer models in nude mice.153 Other studies have indicated that chemically stabilised ribozymes designed to specifically cleave VEGFR coding mRNA could be effective in the inhibition of tumour growth and metastatic activity in rodent xenograft models of metastatic human colorectal cancer.154,155 In addition, preclinical data have hinted at the effectiveness of small antagonistic peptides in antiangiogenic therapy, including integrin α5β1 inhibitory peptides,156 which were reported to be active in the reduction of hepatic metastasis, resulting in improved survival in a rodent colorectal cancer model.157,158
Inhibition of COX‐2 activity has been shown to be effective in a wide variety of preclinical models of solid human tumours, including colorectal carcinoma.131 COX‐2 inhibition was shown to have antiangiogenic effects by downregulation of prostaglandin E2, which in turn is known to potently enhance expression of the angiogenic mediators VEGF and bFGF in an array of target cells, including endothelial cells and colorectal carcinoma epithelial cells.159 Expression of COX‐2 in colorectal cancer specimens was tightly linked to higher microvessel densities and increased VEGF gene expression.160 Clinical studies justifying the use of such agents are lacking so far. As colorectal cancer patients are at increased risk of thrombotic events and COX‐2 inhibitors have been linked to increased risk of thrombosis, the potential for an additive risk has to be considered.161
Thalidomide, a hypnotic drug, possesses anti‐inflammatory and antiangiogenic properties, potentially by downregulation of TNF‐α expression. Thalidomide has been used in combination with palliative chemotherapy regimens using irinotecan (CPT‐11) in colorectal cancer patients. Apart from its ability to ameliorate irinotecan induced side effects, especially nausea and diarrhoea,162 thalidomide is undergoing clinical testing163,164 due to its antiangiogenic effects on colorectal carcinoma in preclinical models.165
Angiogenesis is tightly dependent on the viability of involved endothelial cells. Few studies have investigated the use of antiangiogenic compounds in combination with irradiation therapy. Preliminary evidence supports the concept that irradiation combined with the orally bioavailable VEGF tyrosine kinase inhibitor PTK787/ZK222584 exerts synergistic antiangiogenic effects on VEGF induced endothelial cell proliferation in vitro and a xenograft tumour model of human colorectal carcinoma.166 Similar observations have been made for a variety of human solid tumour implantation models in combination with neutralising anti‐VEGF monoclonal antibodies.167 Advanced clinical studies are urgently needed to clarify the potential synergistic effects of irradiation therapy in combination with such agents in patients with metastatic gastrointestinal cancer.
Surrogate markers of antiangiogenesis in gastrointestinal oncology
With new antiangiogenic treatment strategies emerging and novel compounds being tested in advanced clinical studies, it is now apparent that novel surrogate markers reflecting the biological activity of the tested agents are important for their successful development. Several attempts have been undertaken to define the biological effects obtained by administration of antiangiogenic therapy. However, it has to be emphasised that no adequate surrogate markers of any antiangiogenic treatment strategy have been identified to date and therefore circulating marker levels do not necessarily reflect intratumoral ongoing angiogenesis.
Multiple assays to assess the effects of antiangiogenic effects of novel compounds in clinical trials have been proposed (for example, measuring levels of angiogenic factors in body fluids, including serum, plasma, and urine). It has to be kept in mind however that circulating growth factor levels in serum are not necessarily in total derived from the primary tumour. For example, particulate blood elements, including platelets and neutrophils, represent important compartments for circulating VEGF.168 Therefore, specimen handling is of crucial importance in order to reflect actual serum concentrations of the marker tested.
Further approaches include histological analysis of tumour biopsies (such as laser scanning cytometry), and biological and radiological imaging of tumour associated angiogenic activity (including three dimensional ultrasound, magnetic resonance imaging, computed tomography, and positron emission tomography using 15O‐H2O and 18FDG as tracer substances) also appear to represent markers for evaluation of antiangiogenic therapy.169 Recent studies have suggested that ex vivo analysis of circulating endothelial progenitor cells (CEP) and circulating endothelial cells might be useful in determining the angiogenic activity of human tumours in treated patients. Evidence for this hypothesis comes from a study showing that patients with progressive cancers display significantly higher levels of CEPs compared with healthy controls.170 In humans, levels of CEPs appear to be dependent on expression of VEGF.171 Several attempts have been made to identify surrogate markers in clinical trials using antiangiogenic agents in treated colorectal cancer patients, including monitoring of microarray based gene expression profiles of patient peripheral blood mononuclear cells.172 A multitude of serum markers reflecting tumour associated angiogenesis in colorectal cancer patients with extensive and metastatic disease have been reported. In colorectal cancer patients, serum MMP‐2 and ‐9 levels were associated with metastasis and tumour invasion and were therefore proposed as potential surrogate markers in antiangiogenic therapy.173 As for VEGF, serum levels of bFGF were reported to be elevated in colorectal cancer patients with extensive or metastatic disease.174
Assessment of circulating VEGF levels in colorectal cancer patients
Several studies have reported on the assessment of serum VEGF levels in colorectal cancer patients, showing ambiguous results regarding the correlation of peripheral cytokine levels with clinical angiogenic activity.175 Although correlations were observed for tumour size and volume, with higher circulating VEGF levels, its exclusive use as a diagnostic tumour marker is limited mainly due to low sensitivity.176 Other investigators have reported that T2–T4 tumour stages of colorectal cancer can be detected by elevated VEGF serum levels.177,178 Similarly, serum VEGF levels were reported to be associated with tumour stage, the presence of lymphogenic and distant metastasis, and depth of tumour invasion.179,180 In these patients, serum VEGF levels were shown to decrease after curative, but not palliative, resection.179 In patients having undergone curative surgery for colorectal cancer, the combination of high VEGF and high carcinoembryonic antigen (CEA) levels six months after resection was strongly associated with a poor prognosis and disease recurrence.181 On the other hand, treatment strategies employing monoclonal antibodies against VEGF receptor 2 (KDR) were shown to elevate circulating VEGF levels in treated tumour bearing mice, possibly by competitive antagonism.169 Similarly, the use of bevacizumab in patients with metastatic renal cancer was associated with a significant increase in plasma VEGF levels.182 Elevated VEGF levels might therefore serve as a surrogate marker for determining the optimal biological dose of antibody administration in these patients.183 Recent studies have indicated that elevated circulating VEGF levels in colorectal cancer patients might in fact be derived from cellular compartments other than tumour cells (that is, leucocytes and activated platelets). Evidence for this hypothesis stems from studies showing that extracellular VEGF might accumulate in corpusculate fractions of peripheral blood from patients and subsequently be liberated into the supernatant depending on sample storage conditions.184 In a recent study, Ranieri et al have reported that activated platelet rich plasma anticoagulated with sodium citrate/adenosine/dipyridamole (P‐APRCTAD) represents the peripheral blood fraction most suitable to distinguish healthy controls from colorectal cancer patients by peripheral VEGF levels.185 Further studies will be needed to precisely define the role of VEGF levels in monitoring disease activity and efficacy of antiangiogenic treatment.
To date, there are no validated surrogate markers to monitor antiangiogenic therapy.
Other potential angiogenesis markers in colorectal cancer patients
Further attempts have been made to identify molecules involved in angiogenesis as surrogate markers. Elevated plasma levels of matrix metalloproteinases ‐2 and ‐9, key enzymes involved in the degradation of the basement membrane and the extracellular matrix in tumour invasion and angiogenesis, were reported to be associated with advanced tumour stage in colorectal cancer patients, both decreasing to levels within the normal range following curative surgery.173 Angiogenin, an angiogenic peptide initially identified in culture supernatants of a colorectal cancer cell line, was found to be elevated in the serum of colorectal cancer patients and correlated with disease stage.186 Soluble FLT1 (sFLT), a natural antagonist of circulating VEGF, is detectable in the sera of colorectal cancer patients, but not healthy controls. Interestingly, sFLT levels did not show any significant correlation with serum VEGF levels.187 Similarly, levels of soluble E‐selectin, an endothelial cell adhesion molecule involved in angiogenesis, displayed higher serum levels in metastatic colorectal cancer patients compared with normal controls. In these patient groups, elevated levels of soluble E‐selectin were not correlated with circulating serum markers of systemic inflammation, including C reactive protein, TNF‐α, and fibrinogen.188
Other groups have suggested that molecular imaging of tumour microvasculature using dynamic contrast enhanced magnetic resonance tomography might serve as a potential non‐invasive technique to monitor antiangiogenic therapy in colorectal cancer patients.189
Recent investigation has indicated that the process of angiogenesis is dependent on the equilibrium of fibrinolysis and fibrin polymerisation.190,191 As a prerequisite for neovascularisation, the breakdown of ECM proteins, including cross linked fibrin, appears to be a fundamental step in the growth of tumour associated microvessels. Crosslinked fibrin contained in the ECM represents a stable framework for the migration of endothelial cells during angiogenesis and for tumour cells during invasion. D‐dimers are fibrin degradation fragments which occur in the serum of patients when both intravascular and extravascular crosslinked fibrin is degraded by plasmin.192 As a routinely assessable serum marker, D‐dimers are clinically used to screen for thromboembolic events such as pulmonary embolism and deep venous thrombosis. In patients suffering from solid tumours, including lung, prostate, cervical, and colorectal carcinoma, elevated plasma D‐dimer levels have been shown to be directly correlated with levels of established tumour markers such as CA 125 and CEA. Moreover, in colorectal cancer patients, serum D‐dimer levels were found to correlate with depth of tumour invasion and lymph node involvement.192,193,194
Similar observations have been made by our group in the antiangiogenic treatment of benign intra‐abdominal desmoid lesions using interferon beta and the selective oestrogen receptor modulating agent toremifene. In two patients suffering from extensive intra‐abdominal desmoid disease, treatment with these two agents was associated with an immediate and sustained drop in circulating D‐dimer levels which was accompanied by marked tumour regression and decreasing microvessel density, as assessed in post treatment desmoid tissue.195
Conclusions
Angiogenesis associated with gastrointestinal tumours is a multistep sequence dependent on a plethora of biological and physical factors, including cytokines, chemokines, hypoxia, and tissue pH. Even though blockade of single angiogenic factors has yielded amazing results in a wide variety of rodent preclinical models of gastrointestinal cancers, most of the substances tested have shown disappointing efficacy in the setting of clinical phase II and III studies in the treatment of human gastrointestinal cancer. This is in part due to the fact that rodent vascular biology is different to human physiology in many aspects. On the other hand, fast growing malignant human tumours possess the ability to develop resistance towards blockade of single angiogenesis pathways while utilising the next weakest link in the chain of angiogenic events. Given the multitude of possibilities which tumours use to satisfy their excessive demands of oxygen and nutrients, successful angiogenic therapy will likely consist of a combination of established cytotoxic chemotherapeutic and biological agents. Recent advances in the treatment of colorectal carcinoma using 5‐FU based chemotherapy regimens in conjunction with strategies based on the blockade of circulating VEGF support this hypothesis. The use of adjuvant strategies to enhance the efficacy of modern antiangiogenic therapy will have to be assessed in clinical studies. Those will potentially include selective COX‐2 inhibitors, thalidomide, and radiotherapy.
Footnotes
Conflict of interest: None declared.
References
- 1.Folkman J. Angiogenesis in cancer, vascular, rheumatoid and other disease. Nat Med 1995127–31. [DOI] [PubMed] [Google Scholar]
- 2.Fidler I J, Ellis L M. The implications of angiogenesis for the biology and therapy of cancer metastasis. Cell 199479185–188. [DOI] [PubMed] [Google Scholar]
- 3.Folkman J. What is the evidence that tumors are angiogenesis dependent? J Natl Cancer Inst 1990824–6. [DOI] [PubMed] [Google Scholar]
- 4.Folkman J. How is blood vessel growth regulated in normal and neoplastic tissue? G.H.A. Clowes memorial award lecture. Cancer Res 198646467–473. [PubMed] [Google Scholar]
- 5.Weidner N, Semple J P, Welch W R.et al Tumor angiogenesis and metastasis—correlation in invasive breast carcinoma. N Engl J Med 19913241–8. [DOI] [PubMed] [Google Scholar]
- 6.Garcea G, Lloyd T D, Gescher A.et al Angiogenesis of gastrointestinal tumours and their metastases—a target for intervention? Eur J Cancer 2004401302–1313. [DOI] [PubMed] [Google Scholar]
- 7.Vermeulen P B, Colpaert C, Salgado R.et al Liver metastases from colorectal adenocarcinomas grow in three patterns with different angiogenesis and desmoplasia. J Pathol 2001195336–342. [DOI] [PubMed] [Google Scholar]
- 8.Stessels F, Van den Eynden G, Van der Auwera I.et al Breast adenocarcinoma liver metastases, in contrast to colorectal cancer liver metastases, display a non‐angiogenic growth pattern that preserves the stroma and lacks hypoxia. Br J Cancer 2004901429–1436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Folkman J. Tumor angiogenesis: therapeutic implications. N Engl J Med 19712851182–1186. [DOI] [PubMed] [Google Scholar]
- 10.Deramaudt B M, Braunstein S, Remy P.et al Gene transfer of human heme oxygenase into coronary endothelial cells potentially promotes angiogenesis. J Cell Biochem 199868121–127. [DOI] [PubMed] [Google Scholar]
- 11.Beasley N J, Wykoff C C, Watson P H.et al Carbonic anhydrase IX, an endogenous hypoxia marker, expression in head and neck squamous cell carcinoma and its relationship to hypoxia, necrosis, and microvessel density. Cancer Res 2001615262–5267. [PubMed] [Google Scholar]
- 12.Armulik A, Abramsson A, Betsholtz C. Endothelial/pericyte interactions. Circ Res 200597512–523. [DOI] [PubMed] [Google Scholar]
- 13.Moscatelli D, Presta M, Joseph‐Silverstein J.et al Both normal and tumor cells produce basic fibroblast growth factor. J Cell Physiol 1986129273–276. [DOI] [PubMed] [Google Scholar]
- 14.Weich H A, Iberg N, Klagsbrun M.et al Transcriptional regulation of basic fibroblast growth factor gene expression in capillary endothelial cells. J Cell Biochem 199147158–164. [DOI] [PubMed] [Google Scholar]
- 15.Wang D, Lehman R E, Donner D B.et al Expression and endocytosis of VEGF and its receptors in human colonic vascular endothelial cells. Am J Physiol Gastrointest Liver Physiol 2002282G1088–G1096. [DOI] [PubMed] [Google Scholar]
- 16.Imaizumi T, Itaya H, Nasu S.et al Expression of vascular endothelial growth factor in human umbilical vein endothelial cells stimulated with interleukin‐1alpha—an autocrine regulation of angiogenesis and inflammatory reactions. Thromb Haemost 200083949–955. [PubMed] [Google Scholar]
- 17.Rak J, Mitsuhashi Y, Sheehan C.et al Oncogenes and tumor angiogenesis: differential modes of vascular endothelial growth factor up‐regulation in ras‐transformed epithelial cells and fibroblasts. Cancer Res. 20005 60490–498. [PubMed] [Google Scholar]
- 18.Salcedo R, Resau J H, Halverson D.et al Differential expression and responsiveness of chemokine receptors (CXCR1–3) by human microvascular endothelial cells and umbilical vein endothelial cells. FASEB J 2000142055–2064. [DOI] [PubMed] [Google Scholar]
- 19.Zucker S, Mirza H, Conner C E.et al Vascular endothelial growth factor induces tissue factor and matrix metalloproteinase production in endothelial cells: conversion of prothrombin to thrombin results in progelatinase A activation and cell proliferation. Int J Cancer 199875780–786. [DOI] [PubMed] [Google Scholar]
- 20.Rundhaug J E. Matrix metalloproteinases and angiogenesis. J Cell Mol Med 20059267–285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Uutela M, Wirzenius M, Paavonen K.et al PDGF‐D induces macrophage recruitment, increased interstitial pressure, and blood vessel maturation during angiogenesis. Blood 20041043198–3204. [DOI] [PubMed] [Google Scholar]
- 22.Raghunand N, Gatenby R A, Gillies R J. Microenvironmental and cellular consequences of altered blood flow in tumours. Br J Radiol 200376S11–S22. [DOI] [PubMed] [Google Scholar]
- 23.Jain R K. Tumor angiogenesis and accessibility: role of vascular endothelial growth factor. Semin Oncol 200229(6 suppl 16)3–9. [DOI] [PubMed] [Google Scholar]
- 24.Liotta L A, Kohn E C. The microenvironment of the tumour‐host interface. Nature 2001411375–379. [DOI] [PubMed] [Google Scholar]
- 25.Munn L L. Aberrant vascular architecture in tumors and its importance in drug‐based therapies. Drug Discov Today 20038396–403. [DOI] [PubMed] [Google Scholar]
- 26.Rak J, Yu J L, Klement G.et al Oncogenes and angiogenesis: signaling three‐dimensional tumor growth. J Investig Dermatol Symp Proc 2000524–33. [DOI] [PubMed] [Google Scholar]
- 27.Schmid T, Zhou J, Brune B. HIF‐1 and p53: communication of transcription factors under hypoxia. J Cell Mol Med 20048423–431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Vermeulen P B, Van den Eynden G G, Huget P.et al Prospective study of intratumoral microvessel density, p53 expression and survival in colorectal cancer. Br J Cancer 199979316–322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Liang J T, Huang K C, Jeng Y M.et al Microvessel density, cyclo‐oxygenase 2 expression, K‐ras mutation and p53 overexpression in colonic cancer. Br J Surg 200491355–361. [DOI] [PubMed] [Google Scholar]
- 30.Giatromanolaki A, Stathopoulos G P, Tsiobanou E.et al Combined role of tumor angiogenesis, bcl‐2, and p53 expression in the prognosis of patients with colorectal carcinoma. Cancer 1999861421–1430. [DOI] [PubMed] [Google Scholar]
- 31.Aotake T, Lu C D, Chiba Y.et al Changes of angiogenesis and tumor cell apoptosis during colorectal carcinogenesis. Clin Cancer Res 19995135–142. [PubMed] [Google Scholar]
- 32.Sanz‐Ortega J, Steinberg S M, Moro E.et al Comparative study of tumor angiogenesis and immunohistochemistry for p53, c‐ErbB2, c‐myc and EGFr as prognostic factors in gastric cancer. Histol Histopathol 200015455–462. [DOI] [PubMed] [Google Scholar]
- 33.Ozer E, Ozkal S, Karademir S.et al Angiogenesis and p53 and H‐ras mutations in pancreatic ductal adenocarcinoma. Anal Quant Cytol Histol 199921473–476. [PubMed] [Google Scholar]
- 34.Ince W L, Jubb A M, Holden S N.et al Association of k‐ras, b‐raf, and p53 status with the treatment effect of bevacizumab. J Natl Cancer Inst 200597981–989. [DOI] [PubMed] [Google Scholar]
- 35.Auguste P, Lemiere S, Larrieu‐Lahargue F.et al Molecular mechanisms of tumor vascularization. Crit Rev Oncol Hematol 20055453–61. [DOI] [PubMed] [Google Scholar]
- 36.Asahara T, Masuda H, Takahashi T.et al Bone marrow origin of endothelial progenitor cells responsible for postnatal vasculogenesis in physiological and pathological neovascularization. Circ Res 199985221–228. [DOI] [PubMed] [Google Scholar]
- 37.Hicklin D J, Ellis L M. Role of the vascular endothelial growth factor pathway in tumor growth and angiogenesis. J Clin Oncol 2005231011–1027. [DOI] [PubMed] [Google Scholar]
- 38.Holash J, Maisonpierre P C, Compton D.et al Vessel cooption, regression, and growth in tumors mediated by angiopoietins and VEGF. Science 19992841994–1998. [DOI] [PubMed] [Google Scholar]
- 39.Leenders W P, Kusters B, de Waal R M. Vessel co‐option: how tumors obtain blood supply in the absence of sprouting angiogenesis. Endothelium 2002983–87. [DOI] [PubMed] [Google Scholar]
- 40.Chang Y S, di Tomaso E, McDonald D M.et al Mosaic blood vessels in tumors: frequency of cancer cells in contact with flowing blood. Proc Natl Acad Sci U S A 20009714608–14613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Maniotis A J, Folberg R, Hess A.et al Vascular channel formation by human melanoma cells in vivo and in vitro:vasculogenic mimicry. Am J Pathol 1999155739–752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Zucker S, Cao J, Chen W T. Critical appraisal of the use of matrix metalloproteinase inhibitors in cancer treatment. Oncogene 2000196642–6650. [DOI] [PubMed] [Google Scholar]
- 43.Tuma R S. Success of bevacizumab trials raises questions for future studies. J Natl Cancer Inst 200597950–951. [DOI] [PubMed] [Google Scholar]
- 44.Cao Y. Antiangiogenic cancer therapy. Semin Cancer Biol 200414139–145. [DOI] [PubMed] [Google Scholar]
- 45.St Croix B, Rago C, Velculescu V.et al Genes expressed in human tumor endothelium. Science 20002891197–1202. [DOI] [PubMed] [Google Scholar]
- 46.Binion D G, West G A, Ina K.et al Enhanced leukocyte binding by intestinal microvascular endothelial cells in inflammatory bowel disease. Gastroenterology 19971121895–1907. [DOI] [PubMed] [Google Scholar]
- 47.Arenberg D A, Polverini P J, Kunkel S L.et al In vitro and in vivo systems to assess role of C‐X‐C chemokines in regulation of angiogenesis. Methods Enzymol 1997288190–220. [DOI] [PubMed] [Google Scholar]
- 48.Sakamaki K. Regulation of endothelial cell death and its role in angiogenesis and vascular regression. Curr Neurovasc Res 20041305–315. [DOI] [PubMed] [Google Scholar]
- 49.Salcedo R, Zhang X, Young H A.et al Angiogenic effects of prostaglandin E2 are mediated by up‐regulation of CXCR4 on human microvascular endothelial cells. Blood 20031021966–1977. [DOI] [PubMed] [Google Scholar]
- 50.Tischer E, Mitchell R, Hartman T.et al The human gene for vascular endothelial growth factor. Multiple protein forms are encoded through alternative exon splicing. J Biol Chem 199126611947–11954. [PubMed] [Google Scholar]
- 51.Korc M. Pathways for aberrant angiogenesis in pancreatic cancer. Mol Cancer 200328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Leung D W, Cachianes G, Kuang W J.et al Vascular endothelial growth factor is a secreted angiogenic mitogen. Science 19892461306–1309. [DOI] [PubMed] [Google Scholar]
- 53.Drake C J, Little C D. Exogenous vascular endothelial growth factor induces malformed and hyperfused vessels during embryonic neovascularization. Proc Natl Acad Sci U S A 1995927657–7661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Marconcini L, Marchio S, Morbidelli L.et al c‐fos‐induced growth factor/vascular endothelial growth factor D induces angiogenesis in vivo and in vitro. Proc Natl Acad Sci U S A 1999969671–9676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ku D D, Zaleski J K, Liu S.et al Vascular endothelial growth factor induces EDRF‐dependent relaxation in coronary arteries. Am J Physiol 1993265H586–H592. [DOI] [PubMed] [Google Scholar]
- 56.Hicklin D J, Ellis L M. Role of the vascular endothelial growth factor pathway in tumor growth and angiogenesis. J Clin Oncol 2005231011–1027. [DOI] [PubMed] [Google Scholar]
- 57.Reinmuth N, Parikh A A, Ahmad S A.et al Biology of angiogenesis in tumors of the gastrointestinal tract. Microsc Res Tech 200360199–207. [DOI] [PubMed] [Google Scholar]
- 58.Brogi E, Wu T, Namiki A.et al Indirect angiogenic cytokines upregulate VEGF and bFGF gene expression in vascular smooth muscle cells, whereas hypoxia upregulates VEGF expression only. Circulation 199490649–652. [DOI] [PubMed] [Google Scholar]
- 59.Ellis L M, Liu W, Ahmad S A.et al Overview of angiogenesis: Biologic implications for antiangiogenic therapy. Semin Oncol 200128(suppl 16)94–104. [DOI] [PubMed] [Google Scholar]
- 60.Shaheen R M, Tseng W W, Davis D W.et al Tyrosine kinase inhibition of multiple angiogenic growth factor receptors improves survival in mice bearing colon cancer liver metastases by inhibition of endothelial cell survival mechanisms. Cancer Res 2001611464–1468. [PubMed] [Google Scholar]
- 61.Ellis L M, Takahashi Y, Liu W.et al Vascular endothelial growth factor in human colon cancer: biology and therapeutic implications. Oncologist 20005(suppl 1)11–15. [DOI] [PubMed] [Google Scholar]
- 62.Wong M P, Cheung N, Yuen S T.et al Vascular endothelial growth factor is up‐regulated in the early pre‐malignant stage of colorectal tumour progression. Int J Cancer 199981845–850. [DOI] [PubMed] [Google Scholar]
- 63.Lee J C, Chow N H, Wang S T.et al Prognostic value of vascular endothelial growth factor expression in colorectal cancer patients. Eur J Cancer 200036748–753. [DOI] [PubMed] [Google Scholar]
- 64.Takahashi Y, Kitadai Y, Bucana C D.et al Expression of vascular endothelial growth factor and its receptor, KDR, correlates with vascularity, metastasis, and proliferation of human colon cancer. Cancer Res 1995553964–3968. [PubMed] [Google Scholar]
- 65.Kuniyasu H, Yasui W, Shinohara H.et al Induction of angiogenesis by hyperplastic colonic mucosa adjacent to colon cancer. Am J Pathol 20001571523–1535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Nakasaki T, Wada H, Shigemori C.et al Expression of tissue factor and vascular endothelial growth factor is associated with angiogenesis in colorectal cancer. Am J Hematol 200269247–254. [DOI] [PubMed] [Google Scholar]
- 67.Maeda K, Kang S M, Onoda N.et al Vascular endothelial growth factor expression in preoperative biopsy specimens correlates with disease recurrence in patients with early gastric carcinoma. Cancer 199986566–571. [DOI] [PubMed] [Google Scholar]
- 68.Takahashi Y, Cleary K R, Mai M.et al Significance of vessel count and vascular endothelial growth factor and its receptor (KDR) in intestinal‐type gastric cancer. Clin Cancer Res 199621679–1684. [PubMed] [Google Scholar]
- 69.Fujimoto K, Hosotani R, Wada M.et al Expression of two angiogenic factors, vascular endothelial growth factor and platelet‐derived endothelial cell growth factor in human pancreatic cancer, and its relationship to angiogenesis. Eur J Cancer 1998341439–1447. [DOI] [PubMed] [Google Scholar]
- 70.Ikeda N, Adachi M, Taki T.et al Prognostic significance of angiogenesis in human pancreatic cancer. Br J Cancer 1999791553–1563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Javerzat S, Auguste P, Bikfalvi A. The role of fibroblast growth factors in vascular development. Trends Mol Med 20028483–489. [DOI] [PubMed] [Google Scholar]
- 72.Montesano R, Vassalli J D, Baird A.et al Basic fibroblast growth factor induces angiogenesis in vitro. Proc Natl Acad Sci U S A 1986837297–7301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Fujimoto K, Ichimori Y, Kakizoe T.et al Increased serum levels of basic fibroblast growth factor in patients with renal cell carcinoma. Biochem Biophys Res Commun 1991180386–392. [DOI] [PubMed] [Google Scholar]
- 74.Chodak G W, Hospelhorn V, Judge S M.et al Increased levels of fibroblast growth factor‐like activity in urine from patients with bladder or kidney cancer. Cancer Res 1988482083–2088. [PubMed] [Google Scholar]
- 75.Akbulut H, Altuntas F, Akbulut K G.et al Prognostic role of serum vascular endothelial growth factor, basic fibroblast growth factor and nitric oxide in patients with colorectal carcinoma. Cytokine 200220184–190. [DOI] [PubMed] [Google Scholar]
- 76.George M L, Tutton M G, Abulafi A M.et al Plasma basic fibroblast growth factor levels in colorectal cancer: a clinically useful assay? Clin Exp Metastasis 200219735–738. [DOI] [PubMed] [Google Scholar]
- 77.Landriscina M, Cassano A, Ratto C.et al Quantitative analysis of basic fibroblast growth factor and vascular endothelial growth factor in human colorectal cancer. Br J Cancer 199878765–770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Tanimoto H, Yoshida K, Yokozaki H.et al Expression of basic fibroblast growth factor in human gastric carcinomas. Virchows Arch B Cell Pathol Incl Mol Pathol 199161263–267. [DOI] [PubMed] [Google Scholar]
- 79.Kuwahara K, Sasaki T, Kuwada Y.et al Expressions of angiogenic factors in pancreatic ductal carcinoma: a correlative study with clinicopathologic parameters and patient survival. Pancreas 200326344–349. [DOI] [PubMed] [Google Scholar]
- 80.Ishikawa F, Miyazono K, Hellman U.et al Identification of angiogenic activity and the cloning and expression of platelet‐derived endothelial cell growth factor. Nature 1989338557–562. [DOI] [PubMed] [Google Scholar]
- 81.Moghaddam A, Zhang H T, Fan T P.et al Thymidine phosphorylase is angiogenic and promotes tumor growth. Proc Natl Acad Sci U S A 199592998–1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Seeliger H, Guba M, Koehl G E.et al Blockage of 2‐deoxy‐D‐ribose‐induced angiogenesis with rapamycin counteracts a thymidine phosphorylase‐based escape mechanism available for colon cancer under 5‐fluorouracil therapy. Clin Cancer Res 2004101843–1852. [DOI] [PubMed] [Google Scholar]
- 83.Takahashi Y, Bucana C D, Liu W.et al Platelet‐derived endothelial cell growth factor in human colon cancer angiogenesis: role of infiltrating cells. J Natl Cancer Inst 1996881146–1151. [DOI] [PubMed] [Google Scholar]
- 84.Takahashi Y, Bucana C D, Akagi Y.et al Significance of platelet‐derived endothelial cell growth factor in the angiogenesis of human gastric cancer. Clin Cancer Res 19984429–434. [PubMed] [Google Scholar]
- 85.Hasegawa S, Seike K, Koda K.et al Thymidine phosphorylase expression and efficacy of adjuvant doxifluridine in advanced colorectal cancer patients. Oncol Rep 200513621–626. [PubMed] [Google Scholar]
- 86.Yasuno M, Mori T, Koike M.et al Importance of thymidine phosphorylase expression in tumor stroma as a prognostic factor in patients with advanced colorectal carcinoma. Oncol Rep 200513405–412. [PubMed] [Google Scholar]
- 87.Ogawa M, Ikeuchi K, Takao Y.et al The activities of thymidine phosphorylase and dihydropyrimidine dehydrogenase in colorectal cancer depend on where the sample is taken. Oncol Rep 200514331–335. [PubMed] [Google Scholar]
- 88.Tsigkos S, Koutsilieris M, Papapetropoulos A. Angiopoietins in angiogenesis and beyond. Expert Opin Investig Drugs 200312933–941. [DOI] [PubMed] [Google Scholar]
- 89.Maisonpierre P C, Suri C, Jones P F.et al Angiopoietin‐2, a natural antagonist for Tie2 that disrupts in vivo angiogenesis. Science 199727755–60. [DOI] [PubMed] [Google Scholar]
- 90.Yoshida Y, Oshika Y, Fukushima Y.et al Expression of angiostatic factors in colorectal cancer. Int J Oncol 1999151221–1225. [DOI] [PubMed] [Google Scholar]
- 91.Ahmad S A, Liu W, Jung Y D.et al Differential expression of angiopoietin‐1 and angiopoietin‐2 in colon carcinoma. A possible mechanism for the initiation of angiogenesis. Cancer 2001921138–1143. [DOI] [PubMed] [Google Scholar]
- 92.Ahmad S A, Liu W, Jung Y D.et al The effects of angiopoietin‐1 and ‐2 on tumor growth and angiogenesis in human colon cancer. Cancer Res 2001611255–1259. [PubMed] [Google Scholar]
- 93.Etoh T, Inoue H, Tanaka S.et al Angiopoietin‐2 is related to tumor angiogenesis in gastric carcinoma: possible in vivo regulation via induction of proteases. Cancer Res 2001612145–2153. [PubMed] [Google Scholar]
- 94.Ochiumi T, Tanaka S, Oka S.et al Clinical significance of angiopoietin‐2 expression at the deepest invasive tumor site of advanced colorectal carcinoma. Int J Oncol 200424539–547. [PubMed] [Google Scholar]
- 95.Nakayama T, Hatachi G, Wen C Y.et al Expression and significance of Tie‐1 and Tie‐2 receptors, and angiopoietins‐1, 2 and 4 in colorectal adenocarcinoma: Immunohistochemical analysis and correlation with clinicopathological factors. World J Gastroenterol 200511964–969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Durkin A J, Bloomston M, Yeatman T J.et al Differential expression of the Tie‐2 receptor and its ligands in human pancreatic tumors. J Am Coll Surg 2004199724–731. [DOI] [PubMed] [Google Scholar]
- 97.Semenza G L. Targeting HIF‐1 for cancer therapy. Nat Rev Cancer 20033721–732. [DOI] [PubMed] [Google Scholar]
- 98.Phillips R J, Mestas J, Gharaee‐Kermani M.et al Epidermal growth factor and hypoxia‐induced expression of CXC chemokine receptor 4 on non‐small cell lung cancer cells is regulated by the phosphatidylinositol 3‐kinase/PTEN/AKT/mammalian target of rapamycin signaling pathway and activation of hypoxia inducible factor‐1alpha. J Biol Chem 200528022473–22481. [DOI] [PubMed] [Google Scholar]
- 99.Krishnamachary B, Berg‐Dixon S, Kelly B.et al Regulation of colon carcinoma cell invasion by hypoxia‐inducible factor 1. Cancer Res 2003631138–1143. [PubMed] [Google Scholar]
- 100.Stoeltzing O, McCarty M F, Wey J S.et al Role of hypoxia‐inducible factor 1alpha in gastric cancer cell growth, angiogenesis, and vessel maturation. J Natl Cancer Inst 200496946–956. [DOI] [PubMed] [Google Scholar]
- 101.Kuwai T, Kitadai Y, Tanaka S.et al Expression of hypoxia‐inducible factor‐1alpha is associated with tumor vascularization in human colorectal carcinoma. Int J Cancer 2003105176–181. [DOI] [PubMed] [Google Scholar]
- 102.Yoshimura H, Dhar D K, Kohno H.et al Prognostic impact of hypoxia‐inducible factors 1alpha and 2alpha in colorectal cancer patients: correlation with tumor angiogenesis and cyclooxygenase‐2 expression. Clin Cancer Res 2004108554–8560. [DOI] [PubMed] [Google Scholar]
- 103.Koukourakis M I, Giatromanolaki A, Simopoulos C.et al Lactate dehydrogenase 5 (LDH5) relates to up‐regulated hypoxia inducible factor pathway and metastasis in colorectal cancer. Clin Exp Metastasis 20052225–30. [DOI] [PubMed] [Google Scholar]
- 104.Shibaji T, Nagao M, Ikeda N.et al Prognostic significance of HIF‐1 alpha overexpression in human pancreatic cancer. Anticancer Res 2003234721–4727. [PubMed] [Google Scholar]
- 105.Couvelard A, O'Toole D, Leek R.et al Expression of hypoxia‐inducible factors is correlated with the presence of a fibrotic focus and angiogenesis in pancreatic ductal adenocarcinomas. Histopathology 200546668–676. [DOI] [PubMed] [Google Scholar]
- 106.Rossi D, Zlotnik A. The biology of chemokines and their receptors. Annu Rev Immunol 200018217–242. [DOI] [PubMed] [Google Scholar]
- 107.Strieter R M, Burdick M D, Gomperts B N.et al CXC chemokines in angiogenesis. Cytokine Growth Factor Rev 2005161916–1927. [DOI] [PubMed] [Google Scholar]
- 108.Eckmann L, Jung H C, Schurer‐Maly C.et al Differential cytokine expression by human intestinal epithelial cell lines: regulated expression of interleukin 8. Gastroenterology 19931051689–1697. [DOI] [PubMed] [Google Scholar]
- 109.Yoshida S, Ono M, Shono T.et al Involvement of interleukin‐8, vascular endothelial growth factor, and basic fibroblast growth factor in tumor necrosis factor alpha‐dependent angiogenesis. Mol Cell Biol 1997174015–4023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Takeda A, Stoeltzing O, Ahmad S A.et al Role of angiogenesis in the development and growth of liver metastasis. Ann Surg Oncol 20029610–616. [DOI] [PubMed] [Google Scholar]
- 111.Salcedo R, Resau J H, Halverson D.et al Differential expression and responsiveness of chemokine receptors (CXCR1–3) by human microvascular endothelial cells and umbilical vein endothelial cells. FASEB J 2000142055–2064. [DOI] [PubMed] [Google Scholar]
- 112.Hu D E, Hori Y, Fan T P. Interleukin‐8 stimulates angiogenesis in rats. Inflammation 199317135–143. [DOI] [PubMed] [Google Scholar]
- 113.Fujisawa N, Sakao Y, Hayashi S.et al alpha‐Chemokine growth factors for adenocarcinomas; a synthetic peptide inhibitor for alpha‐chemokines inhibits the growth of adenocarcinoma cell lines. J Cancer Res Clin Oncol 200012619–26. [DOI] [PubMed] [Google Scholar]
- 114.Kim S J, Uehara H, Karashima T.et al Expression of interleukin‐8 correlates with angiogenesis, tumorigenicity, and metastasis of human prostate cancer cells implanted orthotopically in nude mice. Neoplasia 2001333–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Kuniyasu H, Yasui W, Shinohara H.et al Induction of angiogenesis by hyperplastic colonic mucosa adjacent to colon cancer. Am J Pathol 20001571523–1535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Haraguchi M, Komuta K, Akashi A.et al Elevated IL‐8 levels in the drainage vein of resectable Dukes' C colorectal cancer indicate high risk for developing hepatic metastasis. Oncol Rep 20029159–165. [PubMed] [Google Scholar]
- 117.Heidemann J, Ogawa H, Dwinell M B.et al Angiogenic effects of interleukin 8 (CXCL8) in human intestinal microvascular endothelial cells are mediated by CXCR2. J Biol Chem 20032788508–8515. [DOI] [PubMed] [Google Scholar]
- 118.Kitadai Y, Takahashi Y, Haruma K.et al Transfection of interleukin‐8 increases angiogenesis and tumorigenesis of human gastric carcinoma cells in nude mice. Br J Cancer 199981647–653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Shi Q, Abbruzzese J L, Huang S.et al Constitutive and inducible interleukin 8 expression by hypoxia and acidosis renders human pancreatic cancer cells more tumorigenic and metastatic. Clin Cancer Res 199953711–3721. [PubMed] [Google Scholar]
- 120.Peiper S C, Wang Z X, Neote K.et al The Duffy antigen/receptor for chemokines (DARC) is expressed in endothelial cells of Duffy negative individuals who lack the erythrocyte receptor. J Exp Med 19951811311–1317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Chaudhuri A, Polyakova J, Zbrzezna V.et al Cloning of glycoprotein D cDNA, which encodes the major subunit of the Duffy blood group system and the receptor for the Plasmodium vivax malaria parasite. Proc Natl Acad Sci U S A 19939010793–10797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Neote K, Mak J Y, Kolakowski L F., Jret al Functional and biochemical analysis of the cloned Duffy antigen: identity with the red blood cell chemokine receptor. Blood 19948444–52. [PubMed] [Google Scholar]
- 123.Locati M, Torre Y M, Galliera E.et al Silent chemoattractant receptors: D6 as a decoy and scavenger receptor for inflammatory CC chemokines. Cytokine Growth Factor Rev 200516679–686. [DOI] [PubMed] [Google Scholar]
- 124.Zhang Y W, Su Y, Volpert O V.et al Hepatocyte growth factor/scatter factor mediates angiogenesis through positive VEGF and negative thrombospondin 1 regulation. Proc Natl Acad Sci U S A 200310012718–12723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Bancroft C C, Chen Z, Yeh J.et al Effects of pharmacologic antagonists of epidermal growth factor receptor, PI3K and MEK signal kinases on NF‐kappaB and AP‐1 activation and IL‐8 and VEGF expression in human head and neck squamous cell carcinoma lines. Int J Cancer 200299538–548. [DOI] [PubMed] [Google Scholar]
- 126.Warren R S, Yuan H, Matli M R.et al Induction of vascular endothelial growth factor by insulin‐like growth factor 1 in colorectal carcinoma. J Biol Chem 199627129483–29488. [DOI] [PubMed] [Google Scholar]
- 127.Li J, Perrella M A, Tsai J C.et al Induction of vascular endothelial growth factor gene expression by interleukin‐1 beta in rat aortic smooth muscle cells. J Biol Chem 1995270308–312. [DOI] [PubMed] [Google Scholar]
- 128.Brogi E, Wu T, Namiki A.et al Indirect angiogenic cytokines upregulate VEGF and bFGF gene expression in vascular smooth muscle cells, whereas hypoxia upregulates VEGF expression only. Circulation 199490649–652. [DOI] [PubMed] [Google Scholar]
- 129.Ben‐Av P, Crofford L J, Wilder R L.et al Induction of vascular endothelial growth factor expression in synovial fibroblasts by prostaglandin E and interleukin‐1: a potential mechanism for inflammatory angiogenesis. FEBS Lett 199537283–87. [DOI] [PubMed] [Google Scholar]
- 130.Tamura M, Sebastian S, Gurates B.et al Vascular endothelial growth factor up‐regulates cyclooxygenase‐2 expression in human endothelial cells. J Clin Endocrinol Metab 2002873504–3507. [DOI] [PubMed] [Google Scholar]
- 131.Masferrer J L, Leahy K M, Koki A T.et al Antiangiogenic and antitumor activities of cyclooxygenase‐2 inhibitors. Cancer Res 2000601306–1311. [PubMed] [Google Scholar]
- 132.Holmgren L, O'Reilly M S, Folkman J. Dormancy of micrometastases: balanced proliferation and apoptosis in the presence of angiogenesis suppression. Nat Med 19951149–153. [DOI] [PubMed] [Google Scholar]
- 133.Wey J S, Stoeltzing O, Ellis L M. Vascular endothelial growth factor receptors: expression and function in solid tumors. Clin Adv Hematol Oncol 2005337–45. [PubMed] [Google Scholar]
- 134.Hurwitz H, Fehrenbacher L, Novotny W.et al Bevacizumab plus irinotecan, fluorouracil, and leucovorin for metastatic colorectal cancer. N Engl J Med 20043502335–2342. [DOI] [PubMed] [Google Scholar]
- 135.Kabbinavar F F, Hambleton J, Mass R D.et al Combined analysis of efficacy: the addition of bevacizumab to fluorouracil/leucovorin improves survival for patients with metastatic colorectal cancer. J Clin Oncol 2005233706–3712. [DOI] [PubMed] [Google Scholar]
- 136.Kabbinavar F F, Schulz J, McCleod M.et al Addition of bevacizumab to bolus fluorouracil and leucovorin in first‐line metastatic colorectal cancer: results of a randomized phase II trial. J Clin Oncol 2005233697–3705. [DOI] [PubMed] [Google Scholar]
- 137.Willett C G, Boucher Y, di Tomaso E.et al Direct evidence that the VEGF‐specific antibody bevacizumab has antivascular effects in human rectal cancer. Nat Med 200410145–147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Holash J, Davis S, Papadopoulos N.et al VEGF‐Trap: a VEGF blocker with potent antitumor effects. Proc Natl Acad Sci U S A 20029911393–11398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Konner J, Dupont J. Use of soluble recombinant decoy receptor vascular endothelial growth factor trap (VEGF Trap) to inhibit vascular endothelial growth factor activity. Clin Colorectal Cancer 20044(suppl 2)S81–S85. [DOI] [PubMed] [Google Scholar]
- 140.Hu L, Hofmann J, Holash J.et al Vascular endothelial growth factor trap combined with Paclitaxel strikingly inhibits tumor and ascites, prolonging survival in a human ovarian cancer model. Clin Cancer Res 2005116966–6971. [DOI] [PubMed] [Google Scholar]
- 141.Frischer J S, Huang J, Serur A.et al Effects of potent VEGF blockade on experimental Wilms tumor and its persisting vasculature. Int J Oncol 200425549–553. [PubMed] [Google Scholar]
- 142.Fukasawa M, Korc M. Vascular endothelial growth factor‐trap suppresses tumorigenicity of multiple pancreatic cancer cell lines. Clin Cancer Res 2004103327–3332. [DOI] [PubMed] [Google Scholar]
- 143.Posey J A, Ng T C, Yang B.et al A phase I study of anti‐kinase insert domain‐containing receptor antibody, IMC‐1C11, in patients with liver metastases from colorectal carcinoma. Clin Cancer Res 200391323–1332. [PubMed] [Google Scholar]
- 144.Eskens F A. Angiogenesis inhibitors in clinical development; where are we now and where are we going? Br J Cancer 2004901–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Kuenen B C, Levi M, Meijers J C.et al Potential role of platelets in endothelial damage observed during treatment with cisplatin, gemcitabine, and the angiogenesis inhibitor SU5416. J Clin Oncol 2003212192–2198. [DOI] [PubMed] [Google Scholar]
- 146.Sparano J A, Gray R, Giantonio B.et al Eastern Cooperative Oncology Group Portfolio of Clinical Trials. Evaluating antiangiogenesis agents in the clinic: the Eastern Cooperative Oncology Group Portfolio of Clinical Trials, Clin Cancer Res 2004101206–1211. [DOI] [PubMed] [Google Scholar]
- 147.Eichhorn M E, Strieth S, Dellian M. Anti‐vascular tumor therapy: recent advances, pitfalls and clinical perspectives. Drug Resist Updat 20047125–138. [DOI] [PubMed] [Google Scholar]
- 148.Tyagi P. Vatalanib (PTK787/ZK 222584) in combination with FOLFOX4 versus FOLFOX4 alone as first‐line treatment for colorectal cancer: preliminary results from the CONFIRM‐1 trial. Clin Colorectal Cancer 2005524–26. [DOI] [PubMed] [Google Scholar]
- 149.Drevs J, Zirrgiebel U, Schmidt‐Gersbach C I.et al Soluble markers for the assessment of biological activity with PTK787/ZK 222584 (PTK/ZK), a vascular endothelial growth factor receptor (VEGFR) tyrosine kinase inhibitor in patients with advanced colorectal cancer from two phase I trials. Ann Oncol 200516558–565. [DOI] [PubMed] [Google Scholar]
- 150.Caponigro F, Basile M, de Rosa V.et al New drugs in cancer therapy, National Tumor Institute, Naples, 17–18 June 2004. Anticancer Drugs 200516211–221. [DOI] [PubMed] [Google Scholar]
- 151.Kupsch P, Henning B F, Passarge K.et al Results of a phase I trial of sorafenib (BAY 43–9006) in combination with oxaliplatin in patients with refractory solid tumors, including colorectal cancer. Clin Colorectal Cancer 20055188–196. [DOI] [PubMed] [Google Scholar]
- 152.Sakamoto K M. Su‐11248 Sugen. Curr Opin Investig Drugs 200451329–1339. [PubMed] [Google Scholar]
- 153.Kamiyama M, Ichikawa Y, Ishikawa T.et al VEGF receptor antisense therapy inhibits angiogenesis and peritoneal dissemination of human gastric cancer in nude mice. Cancer Gene Ther 20029197–201. [DOI] [PubMed] [Google Scholar]
- 154.Pavco P A, Bouhana K S, Gallegos A M.et al Antitumor and antimetastatic activity of ribozymes targeting the messenger RNA of vascular endothelial growth factor receptors. Clin Cancer Res 200062094–2103. [PubMed] [Google Scholar]
- 155.Parry T J, Cushman C, Gallegos A M.et al Bioactivity of anti‐angiogenic ribozymes targeting Flt‐1 and KDR mRNA. Nucleic Acids Res 1999272569–2577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Yeh C H, Peng H C, Huang T F. Accutin, a new disintegrin, inhibits angiogenesis in vitro and in vivo by acting as integrin alphavbeta3 antagonist and inducing apoptosis. Blood 1998923268–3276. [PubMed] [Google Scholar]
- 157.Stoeltzing O, Liu W, Reinmuth N.et al Inhibition of integrin alpha5beta1 function with a small peptide (ATN‐161) plus continuous 5‐FU infusion reduces colorectal liver metastases and improves survival in mice. Int J Cancer 2003104496–503. [DOI] [PubMed] [Google Scholar]
- 158.Reinmuth N, Liu W, Ahmad S A.et al Alphavbeta3 integrin antagonist S247 decreases colon cancer metastasis and angiogenesis and improves survival in mice. Cancer Res 2003632079–2087. [PubMed] [Google Scholar]
- 159.Cianchi F, Cortesini C, Fantappie O.et al Cyclooxygenase‐2 activation mediates the proangiogenic effect of nitric oxide in colorectal cancer. Clin Cancer Res 2004102694–2704. [DOI] [PubMed] [Google Scholar]
- 160.Cianchi F, Cortesini C, Bechi P.et al Up‐regulation of cyclooxygenase 2 gene expression correlates with tumor angiogenesis in human colorectal cancer. Gastroenterology 20011211339–1347. [DOI] [PubMed] [Google Scholar]
- 161.Wang D, Dubois R N. Prostaglandins and cancer. Gut 200655115–122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Govindarajan R, Heaton K M, Broadwater R.et al Effect of thalidomide on gastrointestinal toxic effects of irinotecan. Lancet 2000356566–567. [DOI] [PubMed] [Google Scholar]
- 163.Dal Lago L, Richter M F, Cancela A I.et al Phase II trial and pharmacokinetic study of thalidomide in patients with metastatic colorectal cancer. Invest New Drugs 200321359–366. [DOI] [PubMed] [Google Scholar]
- 164.Sparano J A, Gray R, Giantonio B.et al Eastern Cooperative Oncology Group Portfolio of Clinical Trials. Evaluating antiangiogenesis agents in the clinic: the Eastern Cooperative Oncology Group Portfolio of Clinical Trials, Clin Cancer Res 2004101206–1211. [DOI] [PubMed] [Google Scholar]
- 165.Fujii T, Tachibana M, Dhar D K.et al Combination therapy with paclitaxel and thalidomide inhibits angiogenesis and growth of human colon cancer xenograft in mice. Anticancer Res 2003232405–2411. [PubMed] [Google Scholar]
- 166.Hess C, Vuong V, Hegyi I.et al Effect of VEGF receptor inhibitor PTK787/ZK222584 combined with ionizing radiation on endothelial cells and tumour growth. Br J Cancer 2001852010–2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Lee C G, Heijn M, di Tomaso E.et al Anti‐Vascular endothelial growth factor treatment augments tumor radiation response under normoxic or hypoxic conditions. Cancer Res 2000605565–5570. [PubMed] [Google Scholar]
- 168.Kusumanto Y H, Dam W A, Hospers G A.et al Platelets and granulocytes, in particular the neutrophils, form important compartments for circulating vascular endothelial growth factor. Angiogenesis 20036283–287. [DOI] [PubMed] [Google Scholar]
- 169.Davis D W, McConkey D J, Abbruzzese J L.et al Surrogate markers in antiangiogenesis clinical trials. Br J Cancer 2003898–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Beerepoot L V, Mehra N, Vermaat J S.et al Increased levels of viable circulating endothelial cells are an indicator of progressive disease in cancer patients. Ann Oncol 200415139–145. [DOI] [PubMed] [Google Scholar]
- 171.Kalka C, Masuda H, Takahashi T.et al Vascular endothelial growth factor(165) gene transfer augments circulating endothelial progenitor cells in human subjects. Circ Res 2000861198–1202. [DOI] [PubMed] [Google Scholar]
- 172.DePrimo S E, Wong L M, Khatry D B.et al Expression profiling of blood samples from an SU5416 Phase III metastatic colorectal cancer clinical trial: a novel strategy for biomarker identification. BMC Cancer 200333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Tutton M G, George M L, Eccles S A.et al Use of plasma MMP‐2 and MMP‐9 levels as a surrogate for tumour expression in colorectal cancer patients. Int J Cancer 2003107541–550. [DOI] [PubMed] [Google Scholar]
- 174.Dirix L Y, Vermeulen P B, Pawinski A.et al Elevated levels of the angiogenic cytokines basic fibroblast growth factor and vascular endothelial growth factor in sera of cancer patients. Br J Cancer 199776238–243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Berglund A, Molin D, Larsson A.et al Tumour markers as early predictors of response to chemotherapy in advanced colorectal carcinoma. Ann Oncol 2002131430–1437. [DOI] [PubMed] [Google Scholar]
- 176.Broll R, Erdmann H, Duchrow M.et al Vascular endothelial growth factor (VEGF)—a valuable serum tumour marker in patients with colorectal cancer? Eur J Surg Oncol 20012737–42. [DOI] [PubMed] [Google Scholar]
- 177.Kumar H, Heer K, Duthie G S.et al Kinetics of postoperative serum vascular endothelial growth factor (VEGF)—can it be used to predict curative resections in colorectal cancer? Anticancer Res 2002223717–3722. [PubMed] [Google Scholar]
- 178.Kumar H, Heer K, Lee P W.et al Preoperative serum vascular endothelial growth factor can predict stage in colorectal cancer. Clin Cancer Res 199841279–1285. [PubMed] [Google Scholar]
- 179.Karayiannakis A J, Syrigos K N, Zbar A.et al Clinical significance of preoperative serum vascular endothelial growth factor levels in patients with colorectal cancer and the effect of tumor surgery. Surgery 2002131548–555. [DOI] [PubMed] [Google Scholar]
- 180.Nakayama Y, Sako T, Shibao K.et al Prognostic value of plasma vascular endothelial growth factor in patients with colorectal cancer. Anticancer Res 2002222437–2442. [PubMed] [Google Scholar]
- 181.Werther K, Christensen I J, Nielsen H J. Danish RANX05 Colorectal Cancer Study Group. The association between preoperative concentration of soluble vascular endothelial growth factor, perioperative blood transfusion, and survival in patients with primary colorectal cancer. Eur J Surg 2001167287–292. [DOI] [PubMed] [Google Scholar]
- 182.Yang J C, Haworth L, Sherry R M.et al A randomized trial of bevacizumab, an anti‐vascular endothelial growth factor antibody, for metastatic renal cancer. N Engl J Med 2003349427–434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Bocci G, Man S, Green S K.et al Increased plasma vascular endothelial growth factor (VEGF) as a surrogate marker for optimal therapeutic dosing of VEGF receptor‐2 monoclonal antibodies. Cancer Res 2004646616–6625. [DOI] [PubMed] [Google Scholar]
- 184.Nielsen H J, Werther K, Mynster T.et al Soluble vascular endothelial growth factor in various blood transfusion components. Transfusion 1999391078–1083. [DOI] [PubMed] [Google Scholar]
- 185.Ranieri G, Coviello M, Patruno R.et al Vascular endothelial growth factor concentrations in the plasma‐activated platelets rich (P‐APR) of healthy controls and colorectal cancer patients. Oncol Rep 200412817–820. [PubMed] [Google Scholar]
- 186.Shimoyama S, Yamasaki K, Kawahara M.et al Increased serum angiogenin concentration in colorectal cancer is correlated with cancer progression. Clin Cancer Res 199951125–1130. [PubMed] [Google Scholar]
- 187.Kumar H, Heer K, Greenman J.et al Soluble FLT‐1 is detectable in the sera of colorectal and breast cancer patients. Anticancer Res 2002221877–1880. [PubMed] [Google Scholar]
- 188.Wittig B M, Kaulen H, Thees R.et al Elevated serum E‐selectin in patients with liver metastases of colorectal cancer. Eur J Cancer 199632A1215–1218. [DOI] [PubMed] [Google Scholar]
- 189.Rehman S, Jayson G C. Molecular imaging of antiangiogenic agents. Oncologist 20051092–103. [DOI] [PubMed] [Google Scholar]
- 190.Dupuy E, Habib A, Lebret M.et al Thrombin induces angiogenesis and vascular endothelial growth factor expression in human endothelial cells: possible relevance to HIF‐1alpha. J Thromb Haemost 200311096–1102. [DOI] [PubMed] [Google Scholar]
- 191.Pirie‐Shepherd S R. Regulation of angiogenesis by the hemostatic system. Front Biosci 20038d286–d293. [DOI] [PubMed] [Google Scholar]
- 192.Blackwell K, Hurwitz H, Lieberman G.et al Circulating D‐dimer levels are better predictors of overall survival and disease progression than carcinoembryonic antigen levels in patients with metastatic colorectal carcinoma. Cancer 200410177–82. [DOI] [PubMed] [Google Scholar]
- 193.Oya M, Akiyama Y, Okuyama T.et al High preoperative plasma D‐dimer level is associated with advanced tumor stage and short survival after curative resection in patients with colorectal cancer. Jpn J Clin Oncol 200131388–394. [DOI] [PubMed] [Google Scholar]
- 194.Edwards C M, Warren J, Armstrong L.et al D‐dimer: a useful marker of disease stage in surgery for colorectal cancer. Br J Surg 1993801404–1405. [DOI] [PubMed] [Google Scholar]
- 195.Heidemann J, Ogawa H, Otterson M F.et al Antiangiogenic treatment of mesenteric desmoid tumors with toremifene and interferon alfa‐2b: report of two cases. Dis Colon Rectum 200447118–122. [DOI] [PubMed] [Google Scholar]
- 196.Kerbel R S, Yu J, Tran J.et al Possible mechanisms of acquired resistance to anti‐angiogenic drugs: implications for the use of combination therapy approaches. Cancer Metastasis Rev 20012079–86. [DOI] [PubMed] [Google Scholar]
- 197.Kang S M, Maeda K, Onoda N.et al Combined analysis of p53 and vascular endothelial growth factor expression in colorectal carcinoma for determination of tumor vascularity and liver metastasis. Int J Cancer 199774502–507. [DOI] [PubMed] [Google Scholar]
- 198.Amaya H, Tanigawa N, Lu C.et al Association of vascular endothelial growth factor expression with tumor angiogenesis, survival and thymidine phosphorylase/platelet‐derived endothelial cell growth factor expression in human colorectal cancer. Cancer Lett 1997119227–235. [DOI] [PubMed] [Google Scholar]
- 199.Maeda K, Nishiguchi Y, Yashiro M.et al Expression of vascular endothelial growth factor and thrombospondin‐1 in colorectal carcinoma. Int J Mol Med 20005373–378. [DOI] [PubMed] [Google Scholar]
- 200.Cascinu S, Staccioli M P, Gasparini G.et al Expression of vascular endothelial growth factor can predict event‐free survival in stage II colon cancer. Clin Cancer Res 200062803–2807. [PubMed] [Google Scholar]
- 201.Harada Y, Ogata Y, Shirouzu K. Expression of vascular endothelial growth factor and its receptor KDR (kinase domain containing receptor)/Flk‐1 (fetal liver kinase‐1) as prognostic factors in human colorectal cancer. Int J Clin Oncol 20016221–228. [DOI] [PubMed] [Google Scholar]
- 202.Kaio E, Tanaka S, Oka S.et al Clinical significance of thrombospondin‐1 expression in relation to vascular endothelial growth factor and interleukin‐10 expression at the deepest invasive tumor site of advanced colorectal carcinoma. Int J Oncol 200323901–911. [PubMed] [Google Scholar]
- 203.Takebayashi Y, Akiyama S, Akiba S.et al Clinicopathologic and prognostic significance of an angiogenic factor, thymidine phosphorylase, in human colorectal carcinoma. J Natl Cancer Inst 1996881110–1117. [DOI] [PubMed] [Google Scholar]
- 204.Saito S, Tsuno N, Nagawa H.et al Expression of platelet‐derived endothelial cell growth factor correlates with good prognosis in patients with colorectal carcinoma. Cancer 20008842–49. [PubMed] [Google Scholar]
- 205.van Triest B, Pinedo H M, Blaauwgeers J L.et al Prognostic role of thymidylate synthase, thymidine phosphorylase/platelet‐derived endothelial cell growth factor, and proliferation markers in colorectal cancer. Clin Cancer Res 200061063–1072. [PubMed] [Google Scholar]
- 206.Matsumura M, Chiba Y, Lu C.et al Platelet‐derived endothelial cell growth factor/thymidine phosphorylase expression correlated with tumor angiogenesis and macrophage infiltration in colorectal cancer. Cancer Lett 199812855–63. [DOI] [PubMed] [Google Scholar]
- 207.Tanigawa N, Amaya H, Matsumura M.et al Correlation between expression of vascular endothelial growth factor and tumor vascularity, and patient outcome in human gastric carcinoma. J Clin Oncol 199715826–832. [DOI] [PubMed] [Google Scholar]
- 208.Kimura H, Konishi K, Nukui T.et al Prognostic significance of expression of thymidine phosphorylase and vascular endothelial growth factor in human gastric carcinoma. J Surg Oncol 20017631–36. [DOI] [PubMed] [Google Scholar]
- 209.Juttner S, Wissmann C, Jons T.et al Vascular endothelial growth factor‐D and its receptor VEGFR‐3: two novel independent prognostic markers in gastric adenocarcinoma. J Clin Oncol 200624228–240. [DOI] [PubMed] [Google Scholar]
- 210.Maeda K, Kang S M, Onoda N.et al Expression of p53 and vascular endothelial growth factor associated with tumor angiogenesis and prognosis in gastric cancer. Oncology 199855594–599. [DOI] [PubMed] [Google Scholar]
- 211.Takebayashi Y, Miyadera K, Akiyama S.et al Expression of thymidine phosphorylase in human gastric carcinoma. Jpn J Cancer Res 199687288–295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Maeda K, Kang S M, Ogawa M.et al Combined analysis of vascular endothelial growth factor and platelet‐derived endothelial cell growth factor expression in gastric carcinoma. Int J Cancer 199774545–550. [DOI] [PubMed] [Google Scholar]
- 213.Nakata B, Hirakawa‐YS, Chung K.et al Thymidine phosphorylase activity in tumor correlates with venous invasion. Int J Mol Med 19982461–464. [DOI] [PubMed] [Google Scholar]
- 214.Saito H, Tsujitani S, Oka S.et al The expression of thymidine phosphorylase correlates with angiogenesis and the efficacy of chemotherapy using fluorouracil derivatives in advanced gastric carcinoma. Br J Cancer 199981484–489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Kikuyama S, Inada T, Shimizu K.et al Thymidine phosphorylase expression in gastric cancer in association with proliferative activity and angiogenesis. Anticancer Res 2000202081–2086. [PubMed] [Google Scholar]
- 216.Konno S, Takebayashi Y, Aiba M.et al Clinicopathological and prognostic significance of thymidine phosphorylase and proliferating cell nuclear antigen in gastric carcinoma. Cancer Lett 2001166103–111. [DOI] [PubMed] [Google Scholar]
- 217.Konno S, Takebayashi Y, Higashimoto M.et al Thymidine phosphorylase expression in gastric carcinoma as a marker for metastasis. Anticancer Res 2003235011–5014. [PubMed] [Google Scholar]
- 218.Sun X D, Liu X E, Wu J M.et al Expression and significance of angiopoietin‐2 in gastric cancer. World J Gastroenterol 2004101382–1385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Ellis L M, Takahashi Y, Fenoglio C J.et al Vessel counts and vascular endothelial growth factor expression in pancreatic adenocarcinoma. Eur J Cancer 199834337–340. [DOI] [PubMed] [Google Scholar]
- 220.Niedergethmann M, Hildenbrand R, Wostbrock B.et al High expression of vascular endothelial growth factor predicts early recurrence and poor prognosis after curative resection for ductal adenocarcinoma of the pancreas. Pancreas 200225122–129. [DOI] [PubMed] [Google Scholar]
- 221.Khorana A A, Hu Y C, Ryan C K.et al Vascular endothelial growth factor and DPC4 predict adjuvant therapy outcomes in resected pancreatic cancer. J Gastrointest Surg 20059903–911. [DOI] [PubMed] [Google Scholar]
- 222.Fujioka S, Yoshida K, Yanagisawa S.et al Angiogenesis in pancreatic carcinoma: thymidine phosphorylase expression in stromal cells and intratumoral microvessel density as independent predictors of overall and relapse‐free survival. Cancer 2001921788–1797. [DOI] [PubMed] [Google Scholar]
- 223.Yamazaki K, Nagao T, Yamaguchi T.et al Expression of basic fibroblast growth factor (FGF‐2)‐associated with tumour proliferation in human pancreatic carcinoma. Virchows Arch 199743195–101. [DOI] [PubMed] [Google Scholar]
- 224.Kitada T, Seki S, Sakaguchi H.et al Clinicopathological significance of hypoxia‐inducible factor‐1alpha expression in human pancreatic carcinoma. Histopathology 200343550–555. [DOI] [PubMed] [Google Scholar]