Wegener's granulomatosis (WG) is a rare form of multisystemic vasculitis. WG most commonly presents as signs and symptoms of upper or lower respiratory tract disease, or both.1 Although clinical manifestations from the gastrointestinal disease have been described,2,3,4,5,6,7,8,9 presentation with extensive intestinal ischaemic perforation without renal or pulmonary disease has not been reported. We report a case of WG presenting with extensive small and large bowel ischaemic perforation without renal or pulmonary disease.
A previously healthy 44 year old female was referred for bronchoscopy with an eight week history of lethargy, polyarthralgia, vasculitic skin rash, and distal sensory and motor polyneuropathy. Laboratory analysis showed normal results on full blood count and urinalysis but an elevated erythrocyte sedimentation rate (79 mm/h; normal <15 mm/h) and positive cytoplasmic antineutrophil cytoplasm antibody (c‐ANCA; titre 1: 89.10). Chest radiograph was normal. A diagnosis of systemic vasculitis secondary to WG was made and intravenous methyl prednisolone was started.
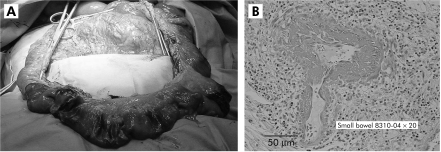
The following day the patient developed severe abdominal pain with signs of peritonitis. Plain film and computed tomography of the abdomen confirmed pneumoperitoneum. At laparotomy, multiple mid‐ileal ischaemic perforations with extensive ischaemic involvement of the left and transverse colon were seen (fig 1A). One metre of small bowel was resected with ileoileal anastomosis and extended left hemicolectomy and a transverse end colostomy. Postoperatively, the patient was continued on intravenous methylprednisolone 1 g for five days followed by dexamethazone 16 mg intravenously daily and cyclophosphamide intravenously 150 mg daily. Histology of the small and large bowel showed extensive vasculitis with fibrinoid necrosis (fig 1B).
Figure 1 (A) Operative view showing multiple areas of ischaemia, necrosis, and perforations. (B) A section of small bowel showing extensive inflammation and vasculitis with fibrinoid necrosis.
On the 32nd day of admission, the patient again developed an acute abdomen and underwent a second laparotomy showing multiple ischaemic perforations at the previous anastomotic site. Further bowel resection, ileostomy, mucous fistula, and re‐fashioning of the colostomy were performed. On day 42 after admission she underwent a third laparotomy due to further ischaemic gangrene of the right colon and ileum; these were excised leaving only 30 cm of jejunum as jejunostomy. Supportive treatment was continued with total parenteral nutrition (TPN). Gradually, cyclophosphamide and steroids were stopped after three and six months, respectively. The vasculitic lesions fully subsided and PR3 ANCA became negative. The patient was discharged on home TPN. Two months later when seen in the outpatients clinic she was well.
WG presents as upper or lower airway symptoms, or both, in 90% of cases.1 Symptomatic gastrointestinal disease in WG is not reported often. There are a few well documented cases which describe only severe forms of the disease affecting part of the bowel, anywhere in the gastrointestinal tract, in the presence of classic lung and renal involvement (table 1). Interestingly, in our patient, almost the whole of the intestine (small and large) was affected without any sign of clinical disease in the lungs or kidneys. The diagnosis of WG in our patient was based on clinical features of systemic vasculitis, high titre of cANCA, and histological evidence of focal necrotising vasculitis in the resected bowel specimen.
Table 1 Gastrointestinal disease in Wegner's granulomatosis.
| Case reports | Age (y) | Sex | GI location | Respiratory/renal involvement | Perforations | Pathology | Surgery | Outcome |
|---|---|---|---|---|---|---|---|---|
| McNabb2 | 50 | M | Distal ileum | Both | Multiple | Ulceration | Yes | Survival |
| Haworth3 | 43 | F | Ileum, caecum, rectum, | Both | None | Ulceration | No | Survival |
| Geraghty4 | 46 | M | Small bowel, colon | Both | Three | Necrosis, ulceration | Yes | Death |
| Tokuda5 | 37 | M | Distal ileum | Both | Single | Necrosis, vasculitis | Yes | Survival |
| Storesund6 Case 1 | 26 | M | Sigmoid, ascending, transverse colon | Both | Single | Ischaemic vasculitis | Yes | Survival |
| Storesund6 Case 2 | 46 | F | Ileum, ascending, transverse, descending, sigmoid colon | Both | None | Inflammation, ischaemic vasculitis | Yes | Survival |
| Skaife7 | 69 | M | Distal jejunum | Both | Multiple | Ischaemic vasculitis | Yes | Death |
| Chow8 | 46 | M | Jejunum | Renal | None | Ulceration, vasculitis | Yes | Survival |
| Pickhardt9 | 26 | M | Ileum, jejunum, colon | Respiratory | None | Necrosis, ischaemic vasculitis | Yes | Survival |
| Our patient | 44 | F | Distal jejunum, ileum, caecum, ascending, transverse, descending, sigmoid colon | None | Multiple | Necrosis, gangrenous, ischaemic vasculitis | Yes | Survival |
Treatment of bowel disease in WG is for the underlying vasculitis, with cyclophosphamide and glucocorticoids. Bowel perforation in our patient occurred a day after initiation of immunotherapy and thus was unlikely to be the cause of the perforation. Older age, renal disease, and high serum creatinine levels have been advocated as predictors of poor outcome.10 The younger age of our patient and no sign of renal involvement with creatinine levels remaining normal throughout disease favoured her survival.
This case highlights the fact that extensive gastrointestinal involvement can occur even in the absence of renal or pulmonary disease in WG.
Acknowledgements
The authors thank Dr James O' Driscoll (Department of Pathology, Mid Western Regional Hospital, Limerick, Republic of Ireland) for selection of slides and interpretation of histological material and Mr Subhasis K Giri for help in the preparation of the manuscript.
Footnotes
Conflict of interest: None declared.
References
- 1.Hoffman G S, Kerr G S, Leavitt R Y.et al Wegener granulomatosis: an analysis of 158 patients. Ann Intern Med 1992116488–498. [DOI] [PubMed] [Google Scholar]
- 2.McNabb W R, Lennox M S, Wedzicha J A. Small intestinal perforation in Wegener's granulomatosis. Postgrad Med J 198258123–125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Haworth S J, Pusey C D. Severe intestinal involvement in Wegener's granulomatosis. Gut 1984251296–1300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Geraghty J, Mackay I R, Smith D C. Intestinal perforation in Wegener's granulomatosis. Gut 198627450–451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tokuda M, Kurata N, Daikuhara H.et al Small intestinal perforation in Wegener's granulomatosis. J Rheumatol 198916547–549. [PubMed] [Google Scholar]
- 6.Storesund B, Gran J T, Koldingsnes W. Severe intestinal involvement in Wegener's granulomatosis: report of two cases and review of the literature. Br J Rheumatol 199837387–390. [DOI] [PubMed] [Google Scholar]
- 7.Skaife P, Lee S, Ramadwar M.et al Intestinal perforation as a presentation of Wegener's granulomatosis. Hosp Med 200061286–287. [DOI] [PubMed] [Google Scholar]
- 8.Chow F Y, Hooke D, Kerr P G. Severe intestinal involvement in Wegener's granulomatosis. J Gastroenterol Hepatol 200318749–750. [DOI] [PubMed] [Google Scholar]
- 9.Pickhardt P J, Curran V W. Fulminant enterocolitis in Wegener's granulomatosis: CT findings with pathologic correlation. AJR Am J Roentgenol 20011771335–1337. [DOI] [PubMed] [Google Scholar]
- 10.Mahr A, Girard T, Agher R.et al Analysis of factors predictive of survival based on 49 patients with systemic Wegener's granulomatosis and prospective follow‐up. Rheumatology (Oxford) 200140492–498. [DOI] [PubMed] [Google Scholar]