A blackout, or transient loss of consciousness (T‐LOC) occurs because there is: a disorder of the circulation—syncope; a disorder of the brain—epilepsy (or other rare neurological condition); a disorder of the psyche—psychogenic seizures.
CAUSES OF BLACKOUTS: EPILEPSY OR SYNCOPE?
It is clear from referral patterns and current care pathways that many doctors assume that T‐LOC is usually caused by epilepsy, but in fact syncope is more likely1,2,3 (table 1). The majority are cases of reflex syncope, with up to 50% of people suffering reflex syncope during their lives. In most patients this presents as simple fainting, and many sufferers never come to neurological evaluation. However, a very significant number of patients with syncope may be misdiagnosed with epilepsy. This is a common mistake, it damages patients lives, may result in failure to respond to treatment, and may be very dangerous. For example, in the UK only about 4% of patients attending neurological clinics have an ECG recorded (http://www.nice.org.uk/pdf/CG020fullguideline.pdf). Cases of T‐LOC caused by transient polymorphic ventricular tachycardia (VT) in the congenital long QT syndrome have been misdiagnosed as epilepsy. This has previously led to cardiac arrest and hypoxic brain damage in young people, after wrong treatment with antiepilepsy drugs (author's experience). The STARS Medical Advisory Committee (STARS MAC, www.stars.org.uk), with European and North American multidisciplinary membership comprising cardiologists, paediatric and adult neurologists and general physicians, agree that this is a worldwide problem. Furthermore, close collaboration between neurologists and cardiologists is now advocated by the National Institute for Health and Clinical Excellence (NICE) guidelines (http://www.nice.org.uk/pdf/CG020fullguideline.pdf), although generally such collaboration still seems to be unusual.
Table 1 Causes of blackout presenting to primary care or emergency departments.
| Kapoor1 1990 | Eagle2 1985 | Day3 1982 | Total (%) | ||
|---|---|---|---|---|---|
| Cardiovascular volume/tone | Vasovagal (reflex) | 35 | 64 | 57 | 15 6(19) |
| Other | 89 | 16 | 9 | 114 (14) | |
| Cardiac (structural heart disease/ arrhythmia) | 110 | 15 | 17 | 142 (18) | |
| Neurological | Epilepsy | 7 | 2 | 58 | 67 (8) |
| Other | 8 | 3 | 5 | 16 (2) | |
| Metabolic/other | 5 | 7 | 27 | 39 (4) | |
| Unknown | 179 | 69 | 25 | 273 (34) | |
| Total | 433 | 176 | 198 | 807 (100) | |
Current understanding puts the prevalence of epilepsy at 0.5–1%.4 Syncope is thought to be more common than epilepsy, affecting 15% of children under the age of 18 years and a similar percentage of middle aged men and women.5 The prevalence rises significantly in the elderly population, with approximately a quarter of all patients over 70 years of age experiencing an attack, of which one third will have a recurrent blackout in the next two years.5 A number of studies, including our own,6 have shown that between 20–30% of patients diagnosed as suffering from epilepsy do not actually have this disorder.7w1 w2 Others put misdiagnosis rates as high as 40%, in children.w3
Zaidi and colleagues6 investigated 74 patients (mean (SD) age of 38.9 (18) years, range 18–77 years) diagnosed with epilepsy, half of them continuing to have seizures despite medication, by means of a head up tilt test and carotid sinus massage during continuous electrocardiographic, electroencephalographic, and blood pressure monitoring. In addition, 10 patients also underwent long term ECG monitoring with an implantable loop recorder. An alternative diagnosis was found in 31 (41.9%) patients including 13 (36.1%) of those taking an anticonvulsant. Eleven of 13 patients (84.6%) who were taking medication could successfully stop this because of an alternative diagnosis being established.
Blackouts or T‐LOC are common—some patients clearly have fainting episodes or syncope caused by an evident arrhythmia, and some patients clearly have epilepsy. However, the common experience of a misdiagnosis of epilepsy indicates that many doctors equate blackouts/T‐LOC with epilepsy and should give syncope much greater consideration, and also indicates that there are a great many patients in whom the cause of T‐LOC is far from clear. These patients are in a “grey area” diagnostically between clear fainting and clear epilepsy. This article aims to explore the reasons why this is so, and examine the value of clinical skills and objective testing in T‐LOC, as well as looking at therapeutic options when a diagnosis is made.
TERMINOLOGY OF BLACKOUTS
One important reason why T‐LOC is misdiagnosed is the misunderstanding caused by the use of confusing terminology. Fortunately, the European Federation of Neurological Societies is establishing a taskforce to clarify this matter (Gert van Dijk, taskforce chairman, personal communication). Meanwhile, there is much confusion. Recent prestigious publications on syncope clearly include patients with epilepsy and other disorders that are not syncope,8,9 adding to this confusion. Table 2 gives suggested terminology that may help relieve confusion.
Table 2 Definitions.
| • Collapse | Abrupt loss of postural tone (with or without T‐LOC) |
| • T‐LOC | Transient loss of consciousness |
| • Syncope | T‐LOC, cause by global impairment of cerebral perfusion causing collapse |
| • Epilepsy | Spontaneous inappropriate discharge of cortical neurones leading to a clinical event |
| • Psychogenic seizure | Transient neurological disturbance without organic cause |
Unfortunately, confusion is caused by reference to causes of T‐LOC that are not the result of transient global impairment of cerebral perfusion as “syncope”. Terms such as “neurologic syncope”8,9 are simply confusing and have no place in the classification of T‐LOC.
A popular colloquialism in acute medicine in the UK is “collapse‐?‐cause”. This term is used extensively in emergency medicine, and this is an important setting for the triage of patients with T‐LOC towards the appropriate care pathway. However, if the terminology used is confused and misunderstood, it is more likely that the clinical evaluation will go wrong and patients will see the wrong doctors. They may then get “trapped” with the wrong diagnosis in the wrong care pathways.
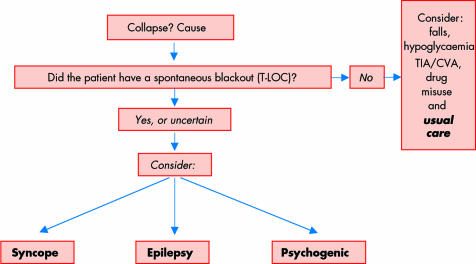
Patients with collapse may not have had T‐LOC. For example, a cerebrovascular accident (CVA) may cause collapse because of unilateral loss of postural tone. However, a patient might remain fully conscious throughout the evolution of a CVA. Patients with T‐LOC may not have collapsed. Some forms of epilepsy disturb awareness, but without abrupt loss of postural tone, as in the “absences” experienced in complex partial seizures. Patients may remain sitting, for example, but become unaware. Where there is collapse and T‐LOC, the differential diagnosis is of syncope, epilepsy, or psychogenic seizures. Figure 1 shows the algorithm that should be followed.
Figure 1 Algorithm for triage of patients with collapse‐?‐cause. CVA, cerebrovascular accident; T‐LOC, transient loss of consciousness; TIA, transient ischaemic attack.
SYNCOPE
Definition
Syncope has been defined by the European Society of Cardiology taskforce on syncope as “a symptom with transient, self limited loss of consciousness usually leading to collapse. The onset of syncope is relatively rapid, and the recovery is spontaneous, complete, and usually prompt. The underlying mechanism is transient global cerebral hypoperfusion”.w4 One of the most common clinical errors is to consider a transient cerebral ischaemic episode (TIA) as a cause of T‐LOC. In fact T‐LOC excludes TIA as a cause of the episode, by accepted definitions: “T‐LOC is a transient loss of consciousness without neurological deficit, and a TIA is a transient neurological deficit, (< 24 hours duration), without T‐LOC.”
Many patients are unnecessarily investigated for carotid disease after an episode of T‐LOC, and some may have had unnecessary operations for incidental carotid stenoses.
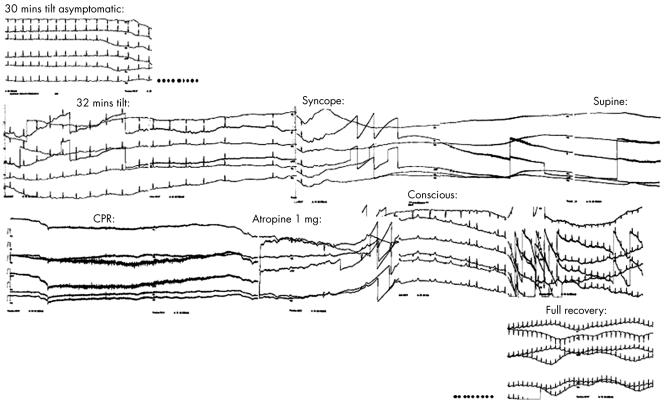
Reflex syncope (also referred to as vasovagal syncope, neurocardiogenic syncope, vasodepressor syncope, neurally mediated hypotension and bradycardia syndrome, emotional fainting, pallid breath holding spells, pallid infantile syncope, reflex anoxic seizure, reflex asystolic syncope, malignant vasovagal syncope, etc) is probably by far the most common cause of syncope. Reflex syncope has an unknown trigger, but the afferent arc synapses with the brain stem cardioinhibitory and vasodepressor centres to cause T‐LOC by vasodepressive hypotension and a variable degree of bradycardia or asystole (fig 2). At one time it was thought that the origin of reflex syncope was the result of inappropriate activation of left ventricular stretch receptors (“low pressure” baroreceptors), by approximation of left ventricular walls in a state of left ventricular underfilling.10 However, such reflexes can be elicited in patients after heart transplantation,11 and this is not now credible as the afferent mechanism.
Figure 2 Asystole induced at 30 minutes of 60° head‐up tilt in a 23 year old woman.
The initial event in reflex syncope remains obscure. Higher cerebral centres have a causative effect in some patients where fear is the trigger—for example, fainting at the sight of blood—which indicates that the cerebral cortex is the origin. Experimental evidence supports this, because direct stimulation of the cerebral cortex in animals can cause hypotension and cardiac asystole.w5
Speculation surrounds the reflex underlying reflex syncope, and its role in evolution. Some have suggested that it represents a “play dead” response to a threat from a predator, whereby the prey might escape death by collapsing and appearing dead. Abrupt collapse and facial pallor in humans might support this, and account for an evolutionary advantage which might have favoured animals who gave this response.
Prevalence
The reported prevalence of syncope varies widely with approximately 15% of children below 18 years of age and middle aged men and women experiencing an episode.5 Falls are also common in this age group, with about 30% of blackouts in the > 65 years age group presenting as falls as there is amnesia to the event.12 Further hampering management, around 70% of blackouts in this age group are unwitnessed, and achieving the appropriate management in this age group can be very challenging. For those patients who are hospitalised, the average length of stay varies from 5–17 days and accounts for most of the cost involved in caring for these patients,13 with falls costing the National Health Service £1 billion per annum.w6 An ageing population means these costs will rise.
Evaluation of a patient with syncope
The aims in evaluating the patient with syncope are to identify any underlying structural heart disease, identify the reason or mechanism of syncope, define any risk of sudden cardiac death, and identify any treatment options.
Patients presenting with T‐LOC or suspected syncope should have a detailed history, a physical examination (including lying and standing blood pressure) and an ECG. Where the ECG is abnormal an echocardiogram must be done. Syncope implies that there has been collapse with T‐LOC. Important features include precipitating factors and warning symptoms, appearance and behaviour during T‐LOC, and the features of the recovery period. Any injuries sustained and specific situations in which syncope occurs—for example, micturition, cough, swallowing, etc—are important. A description from any witness to the episode is essential, where possible. T‐LOC is a story, with a beginning, middle, and end. The history should focus on any premonitory symptoms, the features during unconsciousness, and symptoms during recovery.
Syncope may occur in the setting of structural heart disease, may be associated with palpitations and presyncope, and there may be a history of sudden cardiac death in the family. Consequently, a family history of sudden cardiac death should be sought in all patients, and may be helpful in suspected Brugada syndrome, long QT syndrome or an inherited cardiomyopathy—for example, hypertrophic cardiomyopathy, familial dilated cardiomyopathy, or arrhythmogenic right ventricular dysplasia. In contrast, reflex syncope usually occurs in the absence of cardiac disease, is associated with “autonomic” symptoms like nausea, vomiting and sweating, the patient turns pale during the episodes, and there is often quick recovery of consciousness. Frequently there are precipitating causes like emotional stress as can be experienced at the time of a phlebotomy, reduced plasma volume during prolonged standing or dehydration, low blood pressure caused by low salt intake, and raised intrathoracic pressure impeding venous return in cough syncope and carotid sinus pressure or after exercise. A careful history is important. Syncope after exercise is a manifestation of reflex syncope. Syncope during exercise is much more sinister, and suggestive of cardiomyopathy or primary electrical disease such as Wolff‐Parkinson‐White syndrome or right ventricular dysplasia.
Studies have shown that syncope occurring in the setting of structural heart disease is associated with a poorer prognosis,13 and investigations should be aimed at demonstrating or excluding structural heart disease. Every T‐LOC patient should have at least one 12 lead ECG, especially where syncope seems likely, and especially where there has been sudden cardiac death in a relative under 40 years of age.
Infrastructure for evaluation
The European Society of Cardiology recommends a cohesive, structured care pathway either delivered within a single syncope facility or as a more multifaceted service for the assessment of the patient with syncope. Many models exist. The important principles are speed of access, and a multidisciplinary approach, so that patients cannot get “stuck” in one care pathway, and can easily get access to other disciplines if a particular diagnostic or treatment pathway appears unhelpful. As well as expert opinion, which is by far the most important resource, access to echocardiography, stress testing, electroencephalograms (EEGs), magnetic resonance imaging (MRI)/computed tomographic (CT) scans, and electrophysiology studies is needed. Appendix 1 gives algorithms for point‐of‐care‐pathways for presentation to ambulance crews, emergency departments, and general practice (to view Appendix 1 visit the Heart website—http://www.heartjnl.com/supplemental). These care pathways were developed by the Department of Health Heart Team Expert Reference Group for the National Service Framework for arrhythmias and sudden cardiac death,w7 a multidisciplinary group containing electrophysiologists, cardiologists, neurologists, nurses, technicians, patient advocates, and Heart Team members. A model for referral to secondary care gives a structure for providing a nurse‐led rapid access blackouts clinic, supported by an NCCG (non‐consultant career grade) doctor. Pilot data from such a clinic (run by author PC), in the north west of England suggests that this is an efficient and safe method of evaluating patients, and leads to changes in referral patterns over time, indicating an educational impact.
EPILEPSY
Definition
Epilepsy is a spontaneous, inappropriate discharge of cortical neurones leading to a clinical event.
Diagnosis
A suspicion of epilepsy in blackouts is a common reason for referral to a hospital clinic, but as explained above, most such patients do not have epilepsy. Neurological clinics therefore take many referrals for patients with syncope. It is important that a correct diagnosis is established quickly. The misdiagnosis of epilepsy has unnecessary negative psychosocial and socioeconomic consequences, and other causes of T‐LOC require different investigation and treatment. If epilepsy is confirmed, patients should have a complete diagnosis (detailing the specific epilepsy syndrome), appropriate treatment and counselling, and a continuing care plan. Details are given in the NICE guidelines for epilepsy, published in 2004 (http://www.nice.org.uk/page.aspx?o = 227586). These state that a diagnosis of epilepsy should be made by an appropriate specialist with specific training in the diagnosis and management of epilepsy, and management should involve multidisciplinary and multi‐sector cooperation over a prolonged period, with a team including general practitioners, nurses, and hospital neurological specialists, social workers, and voluntary agency workers. In particular, a diagnosis of epilepsy should no longer be made by a general practitioner, accident and emergency doctor, or general physician, and patients suspected of having epilepsy must be referred to a neurologist. However, given workforce constraints, many patients continue to be seen in busy general neurology or general medical clinics. Others may be diagnosed with epilepsy and treated with anticonvulsants in primary care, given waiting times for expert opinion. This is now contrary to specific national guidelines and misdiagnosis may now have serious medico‐legal implications.
A diagnosis in blackouts depends largely on clinical evaluation, and some patients with epilepsy who are thought to have syncope may be referred to a cardiologist. The detailed classification of epileptic syndromes is complex, but initially patients with epilepsy can usually be divided on clinical and EEG grounds into one of three groups:
Generalised onset epilepsies—The idiopathic generalised epilepsies commence in childhood/adolescence/early adulthood. They are genetically determined conditions associated with generalised spike and wave on the EEG. The brain is structurally normal and cerebral imaging is not required. Patients thought to have idiopathic generalised epilepsy should have an EEG but do not need cerebral imaging (MRI).
Unclassified epilepsy in patients under 30 years of age—These patients could have either idiopathic generalised or partial onset epilepsy caused by structural pathology. Both EEG and MR imaging are required. Patients with unclassified epilepsy beginning before age 30 should have an MR scan and an EEG.
Partial onset epilepsy, or unclassified epilepsy in patients over 30 years of age—All these patients will have a partial onset epilepsy and structural pathology should be excluded by MR in the first instance. An EEG is not required at this stage. Patients with partial seizures or with unclassified seizures after age 30 should have an MR scan but do not need an EEG at this stage.
The diagnosis of epilepsy in elderly people can be more difficult because of the broader differential diagnosis and the possible presence of more than one pathology. Elderly patients with unequivocal seizures are usually managed in a similar way to younger patients. If the diagnosis is uncertain, if the seizures prove to be refractory, or medication is not tolerated they should be seen by a geriatrician experienced in the issues, ideally part of the epilepsy service, and if the diagnosis is called into question, by a cardiologist, in keeping with the NICE guidelines (http://www.nice.org.uk/page.aspx?o = 227586).
There are two further important principles:
For the non‐neurologist clinician dealing with patients with blackouts/T‐LOC, the most important principle is that epilepsy is a clinical diagnosis, it is not diagnosed by an EEG. An EEG is not mandatory in all patients suspected of having epilepsy, and is used to define the epilepsy syndrome, not diagnose epilepsy itself.
We believe that all patients with blackouts/T‐LOC should have at least one 12 lead ECG, with appropriate report. This includes patients with suspected epilepsy, as detailed in the National Service Framework for arrhythmias and sudden cardiac death.w7
Treatment
The aim of treatment is to reduce both the frequency of seizures and any disability or handicap resulting from the diagnosis of epilepsy. Individuals are only able to decide which course of action to take when they understand issues such as the effect on driving, employment, reproductive health, and side effects of treatment. Information, counselling, and support are all important parts of the management alongside the use of appropriate anticonvulsant or antiepileptic drugs. Clinicians can only make informed decisions about drug choices if they are aware of the syndromic diagnosis. All patients with epilepsy should be given full information about their epilepsy, including the type of epilepsy, likely cause, and prognosis, together with the options for medication, and the implications of the drug chosen, so that they can make informed decisions about their treatment and lifestyle.
PSYCHOGENIC SEIZURES
A detailed discussion of this condition is inappropriate here. Patients are usually children or young adults (< 50 years) and have very frequent episodes, often occurring many times a day. Tilt table testing has an important role in these patients. If simultaneous ECG, phasic non‐invasive blood pressure and EEG are monitored, it has been shown that T‐LOC occurs without any change in heart rhythm, blood pressure or electroencephalic recordings.14 These patients are more prone to be female, commonly have a history of self harm or self poisoning, often have a history of childhood abuse, or come from a dysfunctional family background. Proving that T‐LOC during tilt is neither syncopal nor epileptic can be very valuable in reassuring patients and their family, withdrawing treatment when it is not needed, offering continued follow up, and bringing well informed psychological or psychiatric opinion to bear. Other techniques used in the demonstration of a psychogenic basis to T‐LOC include intravenous injection of saline after convincing a patient that this will precipitate T‐LOC.15 Ethical objections to deliberate deception of patients in this way have previously been raised. Using tilt table testing with simultaneous ECG, EEG and phasic blood pressure, which is accepted in the evaluation of T‐LOC and syncope, removes all such concerns.
DIAGNOSTIC TESTS USED BY CARDIOLOGISTS
In patients with T‐LOC, there is no substitute for a thorough history, backed up by eye witness accounts of the beginning, middle, and end of an episode of T‐LOC. However, it is usual for this to be incomplete or imperfect. One important learning point is that there is commonly convulsion in syncope, with abnormal limb movements (often asynchronous—that is, myoclonic), and incontinence is not unusual. The history may not clinch a diagnosis even when it is well taken and well given. A thorough clinical examination is needed in all cases. Naturally, we then turn to investigations in the hope that these will discriminate between causes of T‐LOC—that is, syncope, epilepsy, and psychogenic seizures.
Investigations for syncope
The overwhelming majority of syncope that is diagnosed successfully and quickly is diagnosed by simple clinical evaluation and simple inexpensive tests.13 When patients are admitted through emergency departments, the majority of diagnoses are made by such simple, inexpensive methods. A small number are diagnosed during hospital admission lasting about nine days on average, at approximately 10 times the average cost, but consistently a large minority, up to 50%, remain undiagnosed.13 Where the diagnosis is clear, structural heart disease may be evident, and such patients have a high mortality if the diagnosis is missed, at around 30% per annum.13 Patients discharged without a diagnosis tend to have a good prognosis.13
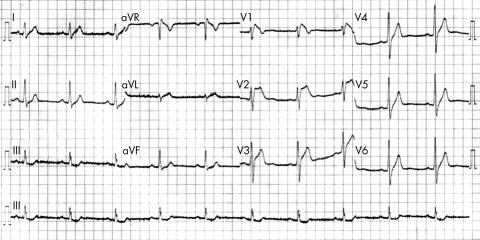
The 12 lead ECG
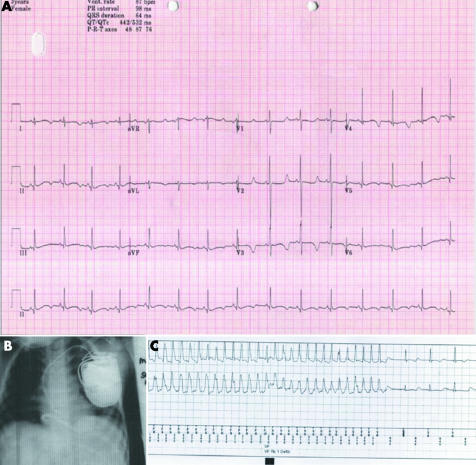
This is mandatory for any patient with collapse, and multiple ECGs will increase the certainty of normality (figs 3 and 4). Some patients may have fluctuant ECG changes—for example, patients with Brugada syndrome (fig 3).
Figure 3 ECG in a 35 year old man admitted with a history of two blackouts, but no chest pain. He received thrombolysis and was referred for urgent coronary angiography when the ECG remained unchanged. The coronary angiogram was normal. He was referred to a neurologist, then eventually to a cardiologist. The ECG changes were those of the Brugada syndrome.
Figure 4 ECG in a 3 year old girl with recurrent blackouts (panel A). She was treated for epilepsy but had continuing symptoms. Eventually an ECG was done which showed evidence of long QT syndrome. β Blockers failed to control symptoms, and she received an implantable cardioverter‐defibrillator (panel B). Three months later interrogation of the device memory shower that further symptoms had been caused by self‐terminating polymorphic ventricular tachycardia (panel C).
Echocardiography
Echocardiography should be done in any patient whose ECGs are not completely normal, and for any usual indication, such as elucidation and characterisation of valve disease when murmurs are heard on clinical examination, and where there is a history of sudden cardiac death in a relative under 40.
ECG monitoring
Twenty four hour ECGs have a negligible yield in syncope.16 ECG event monitoring is little better.17 Long term skin electrodes are impractical. Patients may suffer skin reactions to the adhesive, or fail to be connected during infrequent recurrences of T‐LOC. Devices which are applied intermittently to the chest for a recording are very useful for palpitations, when consciousness is preserved, but are not useful when consciousness is lost in T‐LOC.17
Tilt table testing
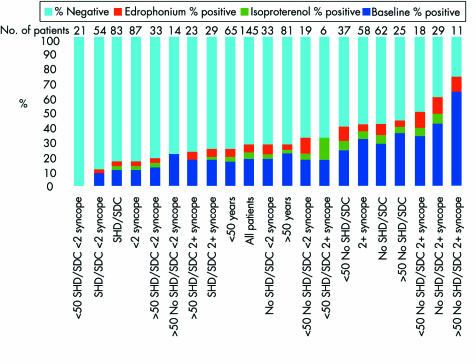
Tilt table testing has been thoroughly investigated over the last 20 years. There are many variations in technique, including angle of tilt,w8 duration of tilt, and the use of adjuvant drug provocation.10,18 One factor of concern is the type of patient enrolled in studies where the yield of tilt testing can vary from 20–70%. With confusion over terminology, and doubts about the cause of T‐LOC, it is likely that populations enrolled in these studies vary significantly. What is crucial in tilt testing is the value of the test in differentiating the cause of T‐LOC, and little evidence exists about the usefulness of tilting in “all‐comers” with T‐LOC. One study looked at clinical features in patients with T‐LOC referred for tilting using baseline 60° tilt for 45 minutes, also evaluating the additive yield of subsequent randomised drug provocation with intravenous isoprenaline and edrophonium.18 The results clearly showed that the pre‐test clinical characteristics of patients in different groups determined their responses to tilting. Young patients with structural heart disease, few episodes before evaluation and aged under 50 years had no positive responses (fig 5, left side of graph). Older patients (> 50 years, multiple T‐LOC episodes, no structural heart disease, right side of graph in fig 5), had a very high yield, approaching 70%.18 Clearly, the yield of tilting is very dependent upon the pre‐test likelihood of a positive or negative yield, and as such is no different from any other provocative test. It is likely that differences in the type of T‐LOC patient enrolled in tilt testing studies in the past may have contributed significantly to the wide variation in yield. Figure 5 also shows that the additive yield of drug provocation after the baseline period of 45 minutes tilt is consistently quite small at about 10–15%.18 Because drug provocation increases the sensitivity of tilt testing (by increasing the number of positive tests), it also inevitably reduces the specificity, by increasing the number of false‐positive tests.
Figure 5 The effect of clinical features in T‐LOC on yield of tilt testing at baseline 45 minute tilt and subsequent randomised provocation with isoprenaline (isoproterenol) or edrophonium injection. Young patients with few T‐LOC episodes, and structural heart disease (SHD) (far left) had no positive tests. Older patients with multiple T‐LOC and no structural heart disease had a high yield of 70%. After baseline tilt, intravenous drug provocation added a small additional yield to baseline tilt, which would have included some inevitable false positive results.18 SDC, presence of another non‐cardiovascular, potential cause of sudden diminished consciousness.
Optimum diagnostic technology for T‐LOC
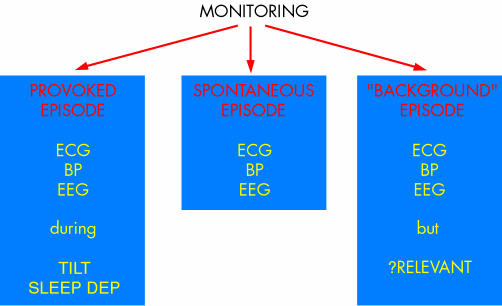
Tests in T‐LOC are of three types. Background information is obtained when an abnormality is documented in a patient with T‐LOC, but without simultaneous symptoms. These data may be helpful, but there are real risks that incidental findings may be over interpreted. For example, in Holter ECG monitoring, the relationships are shown in fig 6.
Figure 6 Methods of obtaining objective physiological monitoring data in patients with T‐LOC. Background data in the absence of symptoms might help, but negative findings could lead to false negative conclusions. BP, blood pressure; ECG, electrocardiogram; EEG, electroencephalogram; SLEEP DEP, sleep deprived EEG recording attempting to provoke epilepsy; TILT, tilt table testing.
A perfect diagnostic technology for T‐LOC would be able to discriminate reliably between syncope, epilepsy, and psychogenic seizures. This would require long term ambulatory monitoring of heart rhythm, blood pressure, and EEG. The nearest available technology is video‐telemetry, which is often used for preoperative work‐up in patients with definite epilepsy awaiting epilepsy surgery.w9 However, video‐telemetry does not monitor blood pressure, may require hospitalisation for many weeks, and is very restrictive, confining patients to a small area in front of a video camera and thus precluding normal life.
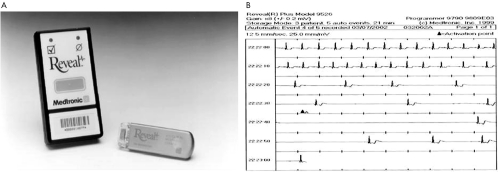
The next nearest current technology is the Reveal implantable ECG loop recorder (ILR) (fig 7), which is implanted subcutaneously on the anterior chest, usually in a short day‐case procedure. It has a useful life of up to 18 months monitoring a high quality single channel ECG only. Recordings to memory can be made automatically over and below certain pre‐set rate limits (based on R wave sensing), but patient activation after an episode of T‐LOC is far more reliable. The yield of ILR testing is far greater than conventional ECG monitoring, and randomised studies have shown that while tilt table testing results do not predict recurrences, positive and negative tilt responders have similar useful yield from ILR recordings.19 The ILR is limited in providing only ECG data during spontaneous T‐LOC, but this is of far greater value and far higher diagnostic yield than any other technology. Further developments need to concentrate on long term monitoring of ECG, EEG, and blood pressure, or physiological surrogates, so that T‐LOC can be differentiated into syncope, epilepsy, or psychogenic seizures with less reliance on clinical skills, and a consequent reduction in misdiagnosis rates.
Figure 7 Reveal loop recorder with external activator. Panel A shows the implantable device and the hand held activator, which is placed on the external skin over the device and used to acquire up to 42 minutes of retrospective and two minutes of prospective ECG. Panel B shows an example of a downloaded recording in a 46 year old man with “epilepsy” diagnosed, investigated, and treated over 15 years. He had also had two driving accidents and lost his driving licence. The episode shown occurred within two months of implantation, and resulted in permanent pacing with complete resolution of symptoms over a seven year follow‐up.
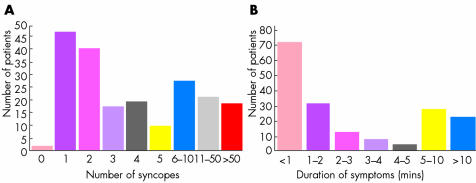
Prolonged ECG monitoring is far more effective than conventional ECG monitoring. In unpublished work in preparation for submission, we compared the yield and diagnostic cost effectiveness of conventional Holter ECG monitoring (fig 8), with long term implanted ECG monitoring in syncope patients with similar clinical profiles (fig 9). Although not completely similar groups, and unrandomised and retrospective, the groups were broadly very similar. One noticeable difference was that patients receiving ILRs had suffered syncope for much longer than the conventional group, probably reflecting a reluctance to refer for an ILR until it was clear that syncope was set to continue.
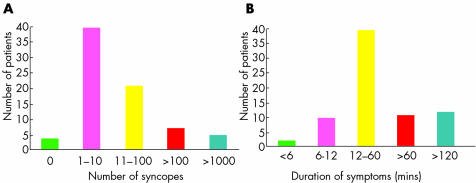
Figure 8 Number of syncopes (A) and duration of symptoms (B) in 345 patients (50% male, mean (SD) age 57 (19) years) with T‐LOC, believed to be syncope, undergoing a mean of 44 hours' continuous external ECG monitoring. Results were that three patients had recurrent spontaneous symptoms during monitoring (symptom/ECG correlation (SECGC) 0.9%), and none showed any concurrent arrhythmias.
Figure 9 Number of syncopes (A) and duration of symptoms (B) in 346 patients (53% male, mean age 56 (20) years), believed to have syncope undergoing long term ECG monitoring with an implanted loop recorder (ILR). In the ILR group 251 (72.6%) of patients achieved SECGC during typical symptoms. Time to first recording was 68 (79) days (range 1–276 days). Forty eight (14%) patients had severe bradycardia or asystole and received permanent pacemakers; five (1.5%) patients had tachyarrhythmias and the findings guided further investigations; and 104 (30%) patients had milder bradycardia and were believed to have reflex syncope. The remainder (55%) had no arrhythmias recorded during typical symptoms, and the diagnosis remains obscure.
In this comparison of similar (though not randomised) groups, the unit cost of Holter monitoring for an average of 44 hours was very low, at £75 per 24 hour tape (cost of tape, cost of technical analysis and share of recorder costs, not including medical reporting time and costs), while the unit cost for IRL implantation was much higher (£2000 per ILR), since the device had to be purchased and implanted, and episodes downloaded. However, almost no patient had a recurrent symptom ECG correlation (SECGC) in the Holter group (which corroborates findings of very low yield of SECGC, and therefore diagnostic yield, in other Holter studies in syncope16). Despite the high unit cost of the Reveal ILR for long term ECG monitoring of spontaneous symptoms, our data suggest that it is far more cost effective than conventional ambulatory ECG monitoring, making SECGC about 4–5 times more expensive using conventional ambulatory ECG monitoring than using the ILR.
MANAGEMENT
Management of T‐LOC consists of getting the diagnosis right, and applying appropriate treatment. In epilepsy, this will usually be antiepilepsy drugs (AEDs), in appropriate dosage and sometimes in combination. In syncope, where the diagnosis is clear early on—for example, in syncope caused by the onset of established complete heart block (classic Stokes‐Adams attack20), manifested on clinical examination and confirmed by ECG—treatment by pacing has no alternatives. In psychogenic seizures, once recognised beyond reasonable doubt, psychological evaluation may uncover suppression of terrors that can respond to treatment.21
Treating reflex syncope remains a major challenge. Studies of permanent pacing for those with pronounced bradycardia or asystole have typically been guided by tilt table responses, which can be unreliable, and lack reproducibility.22 These studies generally give little credit to pacing for alleviating symptoms of syncope.w10–12 However, the RAST study19 showed that patients had similar yield from long term ECG monitoring with an ILR irrespective of whether their tilt table test had previously been positive or negative. This suggests that tilt table responses may not be the best way to select patients for pacing. Recording of spontaneous asystole or severe bradycardia with an ILR seems much more appropriate, and patients such as the one shown in fig 7B have done well with pacing.
Medical treatment may be helpful, although many studies have been non‐randomised, unblinded and without placebo control, greatly limiting the available objective information.23w13 On the basis that left ventricular stretch receptors triggered reflex syncope, and did so in a hyperdynamic state reproduced by isoprenaline infusion during tilt table testing, β blockers were long advocated.10 However, in randomised, blinded, placebo controlled trials they faired no better than placebo.24,25 Midodrine, a α‐adrenoceptor agonist widely available in Europe and the USA, has become a staple treatment, following good evidence that it is effective in the elderly.26 Prescribed in two or three divided doses of 5–30 mg/day, it seems to be very effective in all age groups, without significantly raising blood pressure. Unfortunately, it is only available on a “named patient basis” in the UK, and is not licensed.
Diagnosis and management of patients with blackouts: key points
Blackout/transient loss of consciousness (T‐LOC) is a common and costly problem
Patients with collapse‐?‐cause may or may not have had T‐LOC. The first principle of evaluation is to establish this
Patients with T‐LOC should be approached looking for evidence of syncope, epilepsy, or psychogenic seizures
The correct basis of diagnosis of these conditions with current technology is clinical evaluation
Simple bedside and laboratory tests, done well, have the highest yield in diagnosis
ST elevation is not always caused by an acute coronary syndrome; it occurs in the Brugada syndrome
Many commonly done tests, such as Holter ECG, event ECG monitoring, EEG, and brain imaging have a low yield, because they do not capture physiological data during recurrence of typical presenting symptoms
By far the most valuable test is one which captures physiological data during recurrence of typical presenting symptoms—for example, video‐telemetry or long term ECG monitoring with an implantable loop recorder (ILR)
Holter monitoring in syncope has a very low yield, and ILR monitoring has a very high yield of symptom/ECG correlation (SECGC). This makes Holter monitoring very cost ineffective compared to ILR monitoring. Holter ECG in syncope may cost up to four times the cost of an ILR to achieve SECGC, which is the gold standard in investigation
In reflex syncope, midodrine is a very effective treatment, but it has not been possible to get it licensed in the UK, and it remains available only on a named patient basis
An ideal technology for investigation of T‐LOC would reliably monitor ECG, blood pressure, and EEG over long periods and be able to record all these during an episode of typical symptoms, later making these data available for review
Additional references appear on the Heart website—http://www.heartjnl.com/supplemental
To view Appendix 1 and the additional references, visit the Heart website—http://www.heartjnl.com/supplemental
Supplementary Material
Footnotes
In compliance with EBAC/EACCME guidelines, all authors participating in Education in Heart have disclosed potential conflicts of interest that might cause a bias in the article
To view Appendix 1 and the additional references, visit the Heart website—http://www.heartjnl.com/supplemental
References
- 1.Kapoor W N. Evaluation and outcome of patients with syncope. Medicine 199069160–175. [DOI] [PubMed] [Google Scholar]
- 2.Eagle K A, Black H R, Cook E F.et al Evaluation of prognostic classification for patients with syncope Am J Med 198579455–460. [DOI] [PubMed] [Google Scholar]
- 3.Day S C, Cook E F, Funkenstein H.et al Evaluation and outcome of emergency room patients with transient loss of consciousness. Am J Med 19827315–23. [DOI] [PubMed] [Google Scholar]
- 4.Sander J W A S, Shorvon S D. Epidemiology of the epilepsies. J Neurol Neurosurg Psychiatry 199661433–443.A concise reference article for classification of the epilepsy syndromes. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Smith D, Defalla B A, Chadwick D W. The misdiagnosis of epilepsy and the management of refractory epilepsy in a specialist clinic. Q J M 19999215–23.Beacon UK publication highlighting the problem of the misdiagnosis of epilepsy in neurology clinics. [DOI] [PubMed] [Google Scholar]
- 6.Zaidi A, Clough P, Cooper P.et al Misdiagnosis of epilepsy: many seizure like attacks have a cardiovascular cause. J Am Coll Cardiol 200036181–184.Landmark paper showing that many patients misdiagnosed with epilepsy in fact have syncope. [DOI] [PubMed] [Google Scholar]
- 7.Smith D, Defalla B A, Chadwick D W. The misdiagnosis of epilepsy and the management of refractory epilepsy in a specialist clinic. Q J M 19999215–23. [DOI] [PubMed] [Google Scholar]
- 8.Soteriades E S, Evans J C, Larson M G.et al Incidence and prognosis of syncope. N Engl J Med 2002347878–885.This paper from the USA, and reference 9, confuses T‐LOC with syncope. Syncope is a cause of T‐LOC, as is epilepsy. [DOI] [PubMed] [Google Scholar]
- 9.Chen‐Scarabelli C, Scarabelli T M. Neurocardiogenic syncope. BMJ 2004329336–341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Almquist A, Goldenberg I F, Milstein S.et al Provocation of bradycardia and hypotension by isoproterenol and upright posture in patients with unexplained syncope. N Engl J Med 1989321346–351.Early landmark study showing the effect of head‐up tilt in reproducing symptoms in unexplained syncope. [DOI] [PubMed] [Google Scholar]
- 11.Fitzpatrick A P, Banner N, Cheng A.et al Vasovagal reactions before and after re‐innervation in patients with orthotopic cardiac transplantation. J Am Coll Cardiol 1993211132–1137.Report of studies of tilt table testing in heart transplant recipients, showing that reflex syncope could be produced in spite of cardiac denervation. [DOI] [PubMed] [Google Scholar]
- 12.Parry S W, Steen I N, Baptist M.et al Amnesia for loss of consciousness in carotid sinus syndrome: implications for presentation with falls. J Am Coll Cardiol 2005451840–1843.Important work showing that many elderly patients with falls have had a blackout precipitating the fall, and that they later cannot recall the initial blackout. [DOI] [PubMed] [Google Scholar]
- 13.Kapoor W N, Karpf M, Weant S.et al A prospective evaluation and follow‐up of patients with syncope. N Engl J Med 1983309197–203.Much quoted landmark study with prospective follow‐up of syncope patients. The high cost of admission, investigation, and low yield are highlighted. Also highlighted are the outcomes of syncope with and without structural heart disease. About 50% of patients are undiagnosed despite 10 days in hospital and costly investigations. [DOI] [PubMed] [Google Scholar]
- 14.Zaidi A, Crampton S, Clough P.et al Head‐up tilting is a useful provocative test for psychogenic non‐epileptic seizures. Seizure 19996353–355.Use of tilt table testing to diagnose psychogenic seizures or non‐epileptic attack disorder (NEAD). [DOI] [PubMed] [Google Scholar]
- 15.Slater J D, Brown M C, Jacobs W.et al Induction of pseudoseizures with intravenous saline placebo. Epilepsia 199536580–585.Use of intravenous saline injection to precipitate NEAD has aroused some debate about ethical considerations of tricking patients. [DOI] [PubMed] [Google Scholar]
- 16.Gibson T C, Heitzman M R. Diagnostic efficacy of 24‐hour electrocardiographic monitoring for syncope. Am J Cardiol 1984531013–1017.Large study of 24 hour Holter monitoring in syncope, showing yield of < 1%. [DOI] [PubMed] [Google Scholar]
- 17.Linzer M, Pritchett E L, Pontinen M.et al Incremental diagnostic yield of loop electrocardiographic recorders in unexplained syncope. Am J Cardiol 199066214–219.Yield of external loop recorders varies from about 10–30% in T‐LOC. [DOI] [PubMed] [Google Scholar]
- 18.Fitzpatrick A P, Lee R J, Epstein L M.et al Effect of patient characteristics on the yield of prolonged baseline head‐up tilt‐testing and the additive yield of drug provocation. Heart 199676406–411.The only known “all comers” study of tilt testing in T‐LOC. Shows that the tilt test response depends upon the pre‐test likelihood of a positive or negative test, and that overall yield in T‐LOC is about 20%, as against 10% in controls. Shows that drug provocation after baseline unmedicated tilt has a low additive yield. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Krahn A D, Klein G J, Yee R.et al Randomized assessment of syncope trial: conventional diagnostic testing versus a prolonged monitoring strategy. Circulation 200110446–51.Randomised study showing that the yield of implantable ECG monitoring in syncope is independent of tilt table testing result. [DOI] [PubMed] [Google Scholar]
- 20.Stokes W. Observations on some cases of permanently slow pulse. Dublin Q J M Sci 1846273–74.Original description of the Stokes‐Adam attack caused by heart block. [Google Scholar]
- 21.Lesser R P. Treatment and outcome of psychogenic nonepileptic seizures. Epilepsy Curr 20033198–200.Useful review of the background to psychogenic seizures, which may account for 5–15% of T‐LOC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fitzpatrick A P, Theodorakis G, Ahmed R.et al Methodology of head‐up tilt in the investigation of unexplained syncope. J Am Coll Cardiol 199117125–130.Early work showing a high yield in elderly patients with syncope and no structural heart disease (70%), a low yield in controls with syncope caused by heart block or sick sinus syndrome (10%), but a low reproducibility of tilt table testing within patients. Also demonstrated was the need for the angle of tilt to be 60° or greater. [DOI] [PubMed] [Google Scholar]
- 23.Grubb B P, Samoil D, Kosinski D.et al Fluoxetine hydrochloride for the treatment of severe refractory orthostatic hypotension. Am J Med 199497366–368.Unrandomised, uncontrolled study of medical treatment for reflex syncope showing benefits. [DOI] [PubMed] [Google Scholar]
- 24.Fitzpatrick A P, Ahmed R, Williams S.et al A randomised trial of medical therapy for vasodepressor vasovagal syncope. Eur J Pacing Electrophysiol 1991243–48.Randomised, placebo controlled, double blind crossover study of clonidine, scopolamine patches and atenolol treatment for reflex syncope showed no benefits over placebo. [Google Scholar]
- 25.Madrid A H, Ortega J, Rebollo J G.et al Lack of efficacy of atenolol for the prevention of neurally mediated syncope in a highly symptomatic population: a prospective, double‐blind, randomized and placebo‐controlled study. J Am Coll Cardiol 200137554–559.Randomised, placebo controlled, double blind study of atenolol for treatment for reflex syncope showed no benefits over placebo. [DOI] [PubMed] [Google Scholar]
- 26.Ward C R, Gray J C, Gilroy J J.et al Midodrine: a role in the management of neurocardiogenic syncope. Heart 19987945–49.Randomised, placebo controlled, double blind study of midodrine in the treatment for reflex syncope showed significant benefits over placebo. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.