Abstract
Objectives
To examine recent time trends in blood pressure (BP), total cholesterol, body mass index (BMI) and current smoking among people in the UK of different deprivation groups.
Design
Repeatable survey.
Setting
Primary care‐based UK cardiovascular risk factor screening programme (58 Stockport general practices).
Participants
37 161 women and 33 977 men aged 35–60 years responding to a screening invitation and with a first screening episode during 1989–99.
Results
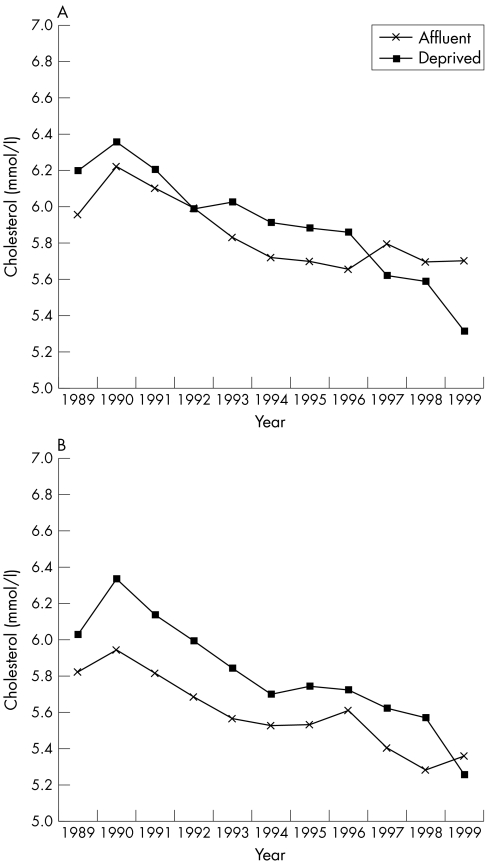
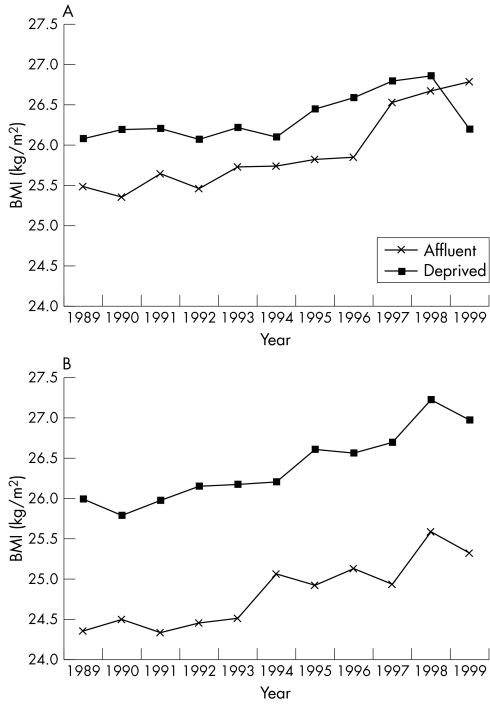
There were significant decreasing trends in total cholesterol (−0.06 mmol/l/year, 95% confidence interval (CI) −0.07 to −0.06 for women, −0.07 mmol/l/year, 95% CI −0.07 to −0.06 for men), with a significantly faster drop in more deprived groups (−0.005 mmol/year/increasing deprivation group, 95% CI −0.01 to −0.001 for both sexes). There were decreasing trends in current smoking prevalence (odds ratio (OR) 0.97/year, 95% CI 0.96 to 0.97 for women, OR 0.96/year, 95% CI 0.95 to 0.96 for men) with a significantly slower drop in the more deprived groups (OR 1.01/year/increasing deprivation group, 95% CI 1.00 to 1.01 for both sexes). There were significant increasing trends in BMI (0.11 kg/m2/year in women, 95% CI 0.09 to 0.13, 0.10 kg/m2/year in men, 95% CI 0.08 to 0.11), with a significantly slower increase in the more deprived groups among men only (−0.02 kg/m2/year/increasing deprivation group, 95% CI −0.01 to −0.03). Inequality in BP narrowed among men but widened among women.
Conclusion
Inequalities in risk factors between different deprivation groups may be both widening (smoking, BP in women) and narrowing (total cholesterol, BMI and BP in men). Given baseline inequalities in risk factors levels, these trends suggest that inequalities in cardiovascular disease are likely to persist in the future.
Cardiovascular disease, including coronary heart disease and stroke, is the leading cause of death in the UK and is responsible for about 238 000 deaths annually, or 39% of total mortality.1 Lower socioeconomic status is strongly associated with both higher prevalence of cardiovascular disease and higher prevalence of various cardiovascular risk factors.
In the UK, decreasing population trends in cardiovascular risk factors such as total cholesterol, smoking and blood pressure (BP) have been observed since at least the early 1990s; however, other factors such as body mass index (BMI) have tended to deteriorate.2 Whereas the recent epidemiology of major cardiovascular risk factors for the UK population as a whole is relatively well described, there is a paucity of information about cardiovascular risk factors in specific UK deprivation groups, as, for example, sources such as the Health Survey for England and the Whitehall studies measure socioeconomic status by individual, as opposed to area‐based, measures. Previous research has shown the relevance of area of residence as a determinant of cardiovascular risk, independently and in addition to the effect of individually measured socioeconomic status.3,4
Historical trends data about cardiovascular risk factors can help predict future expected disease burden, as previously described for the general UK population.5,6,7 There is, however, a relative paucity of evidence about risk factor time trends in population subgroups, such as deprivation groups. Such evidence is important both for the monitoring of changes in health inequalities and for healthcare service planning and health promotion initiatives. The acquisition of information about historical trends in cardiovascular risk factors therefore can be seen as a research priority.
A previous meta‐analysis of studies reported between 1977 and 1996 challenged the overall effectiveness and cost effectiveness of multiple cardiovascular risk factor screening.8 One potentially important secondary use of population‐based screening programmes is, however, as public health surveillance tools to monitor trends in population risk factors and determinants, as highlighted by the UK government's white paper on public health.9 The Stockport Cardiovascular Disease Risk Factor Screening Programme, originally introduced in 1989,10 provides an example of the potential for secondary use of routine data sources for public health surveillance purposes. Further details about operating protocols and population coverage of this programme have been previously described.11,12,13
Briefly, the programme was introduced in 1989 and used a call‐recall system operated by the Stockport Health Authority, where all Stockport residents aged between 35–60 were invited every five years to book a screening appointment at their general practice surgery. Cardiovascular risk factors including BP, total cholesterol, BMI and smoking status were assessed by a general practitioner or, more often, by a practice nurse. Between 1989 and 1993, about 10.8% of all patients registered with a general practitioner were excluded from the screening invitation, as they were already known to have hypertension (3.9%), diabetes (1.2%), and conditions including a history of any cardiovascular disease and terminal illness (6.6%)—note that some patients had more than one indication for exclusion.11 Over the 11‐year period 1989–99, the population coverage for one (first) screening was about 72.2% for Stockport men aged 35–60 and about 78.4% for Stockport women (see supplemental file 1 on the Heart website—http://www.heartjnl.com/supplemental).13 Individual data on risk factor levels were collated by the Health Authority and anonymised into a usable electronic dataset, which was used in the present study.11,12 We therefore conducted a study to examine recent risk factor trends in BP, cholesterol, BMI and smoking status among people of various deprivation groups by using the Stockport cardiovascular risk factor screening dataset 1989–99.
Stockport is a borough of northwest England. In recent years, general population health has been slightly better than that of the general UK population, with a standardised mortality ratio from all causes (all ages) of 96 (95% confidence interval (CI) 94 to 98).14
METHODS
Information on men and women aged 35–60 who had a first screening episode during the 11‐year period between 1989 and 1999 was analysed.
Deprivation status and risk factor measurements
Information on deprivation status was based on the enumeration district of residence (1991 census) Townsend deprivation index score.15 The Townsend deprivation score measures deprivation at a small area level (census enumeration district) based on information from four separate census‐based variables: unemployment (unemployed residents older than 16 as a percentage of all economically active residents older than 16), overcrowding (households with one or more people to a room as a percentage of all households), non‐car ownership (households with no car as a percentage of all households) and non‐home ownership (households not owning their own home as percentage of all households) (see also http://www.avon.nhs.uk/phnet/Methods/townsend.htm). Five deprivation quintiles were defined based on the Stockport distribution of the Townsend score. The range of Townsend scores among study participants was −7.12 to 10.9 (mean −1.69, median −2.39, SD 2.88). The range for the population of England and Wales as a whole was −7.55 to 11.8 (mean 0, median −0.65, SD 3.39). Details of other risk factor measurements are available in supplemental file 2 on the Heart website (http://www.heartjnl.com/supplemental) and as described previously.11
Statistical analysis
For each deprivation group and by sex, the mean age of participants and the completeness of ascertainment of each risk factor were calculated. The significance of differentials in screening coverage by deprivation group was assessed with logistic regression, with deprivation group entered as a continuous variable, and when appropriate adjusted for age.
To assess whether risk factor levels differed between deprivation groups, age‐standardised risk factor levels by year and sex were calculated by the direct method.16,17,18 Associated 95% CIs were calculated by the normal approximation to the binomial distribution for each age stratum.
To inform the interpretation further and to assess the significance of any risk factor level differences by deprivation group, linear regression models adjusted for age and test year were constructed. No attempt was made to examine interaction effects (correlations) between the risk factors—that is, each risk factor was treated individually in all models. Each continuous risk factor was used as the dependent variable, adjusted for age, test year and deprivation group, entered as a continuous variable (model 1a). The coefficient for deprivation group denotes the (age‐ and test year‐adjusted) overall difference in risk factor levels between a given deprivation group and the group that is immediately more deprived, for all study years 1989–99. For smoking, logistic regression was used, with smoking status (current or non‐current) as the dependent binary variable, and age, test year and deprivation group entered as a continuous variable (model 1b). The exponential of the coefficient denotes the (age‐ and test year‐adjusted) overall difference in probability of current smoking status between the given deprivation group and the group immediately more deprived (hereafter “by incremental deprivation groups”), for all study years 1989–99.
To illustrate the effect of deprivation status on trends, both the absolute and the proportional (percentage) difference in risk factor levels between the first (1989) and the last (1999) study year are presented for quintiles 1 (least deprived, or “affluent”) and 5 (“deprived”).
To examine time trends in risk factor levels by deprivation group further, for each continuous risk factor a linear regression model was fitted, with age and test year as the independent variables, and applied to each deprivation group separately (model 2a). Similarly, for smoking, a logistic regression model was constructed, with current smoking status as the dependent variable and adjusted for age and test year, and applied separately to each deprivation group (model 2b). The coefficients for test year from these models denote the mean annual age‐adjusted change in the risk factor level (continuous variables), or mean annual change in the logit of the probability of smoking status, specific to each deprivation group, for each study year (on average) of the 1989–99 study period.
Convergence or divergence in risk factor trends between deprivation groups (that is, significant differentials in speed of risk factor change over time) was assessed with the significance level of the coefficient for an interaction term deprivation group × test year, which was added to models also including age, test year and deprivation group as independent variables (models 3a and 3b). The coefficient for this interaction term denotes by how much the level of a continuous risk factor (or the probability of current smoking status) changes by moving simultaneously from one study year to the next, and by one deprivation group to the one immediately more deprived. Interaction variables were centred to avoid possible co‐linearity.
Sensitivity analysis
Additionally, alternatively analytical approaches were used to minimise the potential that the results obtained were due to systematic differences in deprivation and age profile of participants in different periods of the programme (1989–93 and 1994–9). In particular, alternative modelling approaches were the following:
Only including in the models patients aged 35–39 in each study year 1989–99
Including in the models a study period variable (1989–93 or 1994–9)—that is, adjusting for study period in the models used in analysis
Restricting analysis to the two study periods sequentially (1989–93 and 1994–9).
RESULTS
There were 37 294 women and 34 122 men aged 35–60 with a first screening episode between 1989 and 1999. Among these, it was possible to ascribe deprivation status to 37 161 women (99.6%) and 33 977 men (99.6%). About two thirds of the data relate to the period 1989–93.
Participant characteristics and ascertainment completeness
Certain systematic differences between participants of various deprivation groups were observed, including in relation to ascertainment for cholesterol, BMI and smoking (diastolic BP ascertainment was complete and systolic BP nearly complete for all groups and both sexes), although the order of magnitude (size) of these otherwise significant differences was small in both absolute and relative terms (table 1). In addition, participants in the 1989–93 study period were significantly older than those of the 1994–9 period. More specifically:
Table 1 Main characteristics of participants, by deprivation group.
| Affluent | 2 | 3 | 4 | Deprived | p Value for trend | |
|---|---|---|---|---|---|---|
| Women | ||||||
| Number | 7407 | 7466 | 7416 | 7426 | 7446 | |
| Mean age (years) | 45.8 | 45.8 | 45.7 | 45.2 | 45.9 | 0.224* |
| IQR | 39–53 | 39–53 | 39–53 | 38–51 | 39–54 | |
| % of first screening episodes during 1989–93 | 71.2 | 70.4 | 68.4 | 68.0 | 66.8 | <0.001† |
| Mean age during 1989–93 | 46.8 | <0.001 | ||||
| Median (IQR) | 45.0 (40.0–54.0) | |||||
| Mean age during 1994–1999 | 43.1 | |||||
| Median (IQR) | 40.0 (35.0–50.0) | |||||
| BMI ascertainment | 74.5% | 76.5% | 81.3% | 85.4% | 84.3% | <0.001† |
| Cholesterol ascertainment | 54.6% | 50.3% | 47.0% | 54.1% | 55.0% | 0.009† |
| Smoking status ascertainment | 74.9% | 76.6% | 81.5% | 86.0% | 85.3% | <0.001† |
| Men | ||||||
| Number | 6770 | 6851 | 6737 | 6827 | 6792 | |
| Mean age (years) | 45.9 | 45.8 | 45.5 | 45.0 | 45.5 | <0.001* |
| IQR | 40–53 | 40–53 | 39–52 | 37–51 | 39–53 | |
| % of first screening episodes during 1989–93 | 68.7 | 67.7 | 65.7 | 62.9 | 61.4 | <0.001† |
| Mean age during 1989–93 | 46.6 | <0.001 | ||||
| Median (IQR) | 45.0 (40.0–54) | |||||
| Mean age during 1994–1999 | 43.6 | |||||
| Median (IQR) | 41.0 (35.0–50.0) | |||||
| BMI ascertainment | 78.7% | 79.8% | 85.2% | 87.1% | 84.9% | <0.001† |
| Cholesterol ascertainment | 60.6% | 56.3% | 59.2% | 60.2% | 57.2% | 0.092† |
| Smoking status ascertainment | 79.2% | 79.8% | 85.4% | 87.8% | 85.0% | <0.001† |
*From regression; †from regression adjusted for age.
BMI, body mass index; IQR, interquartile range.
The mean age of participants was significantly greater among least deprived men than among more deprived men, with an absolute mean difference between the least and most deprived groups of 0.4 years. A similar apparent trend among women was not significant.
A greater proportion of participants in the 1989–93 study period of the programme belonged to the least deprived groups.
Ascertainment completeness was systematically higher among the more deprived groups for BMI and smoking, and for cholesterol among women only (absolute difference between the most and least deprived groups of −0.4%), mirroring previously described findings.12
Risk factor levels by deprivation group
As a whole, more deprived women and men consistently during the whole study period 1989–99 had significantly higher levels of (or exposure to) each risk factor. Among women, for any incremental progression in deprivation group there was a significant increase in systolic BP (0.56 mm Hg, 95% CI 0.45 to 0.67), diastolic BP (0.37 mm Hg, 95% CI 0.31 to 0.44), total cholesterol (0.07 mmol/l, 95% CI 0.06 to 0.08) and BMI (0.39 kg/m2, 95% CI 0.36 to 0.43) (table 2, model 1a). Similarly, among men, for any ordinal increase in deprivation group there was a significant increase in systolic BP (0.47 mm Hg, 95% CI 0.35 to 0.58), diastolic BP (0.33 mm Hg, 95% CI 0.26 to 0.41), total cholesterol (0.02 mmol/l, 95% CI 0.01 to 0.03) and BMI (0.11 kg/m2, 95% CI 0.08 to 0.14). For any ordinal increase in deprivation group, there was a significant increase in probability of current smoking status for both women and men, with odds ratios (ORs) of 1.24 (95% CI 1.22 to 1.26) for men and 1.26 (95% CI 1.24 to 1.28) for women (table 3, model 1b).
Table 2 Increase in mean risk factor levels by one level increase in deprivation group (DG) (model 1a), risk factor level time trends by DG (model 2a) and differential risk factor trends by one level increase in DG (model 3a).
| Men | Women | |||||
|---|---|---|---|---|---|---|
| Mean | 95% CI | p Value | Mean | 95% CI | p Value | |
| Systolic blood pressure | ||||||
| Model 1a (overall difference between incremental DGs) | ||||||
| DG trend difference* | 0.47 | 0.35 to 0.58 | <0.001 | 0.56 | 0.45 to 0.67 | <0.001 |
| Model 2a (DG‐specific risk factor level time trends)† | ||||||
| Affluent | 0.30 | 0.18 to 0.43 | <0.001 | −0.10 | −0.23 to 0.28 | 0.124 |
| 2 | 0.13 | 0 to 0.25 | 0.052 | −0.07 | −0.20 to 0.06 | 0.294 |
| 3 | 0.23 | 0.10 to 0.35 | 0.001 | 0.04 | −0.09 to 0.17 | 0.550 |
| 4 | 0.27 | 0.14 to 0.40 | <0.001 | −0.03 | −0.16 to 0.10 | 0.617 |
| Deprived | 0.20 | 0.07 to 0.33 | 0.002 | 0.17 | 0.04 to 0.31 | 0.009 |
| All DGs | 0.23 | 0.18 to 0.29 | <0.001 | 0.01 | −0.05 to 0.07 | 0.750 |
| Model 3a (time trend difference between incremental DGs) | ||||||
| DG × time‡ | −0.02 | −0.06 to 0.02 | 0.418 | 0.05 | 0.01 to 0.09 | 0.010 |
| Diastolic blood pressure | ||||||
| Model 1a (overall difference between incremental DGs) | ||||||
| DG trend difference* | 0.33 | 0.26 to 0.41 | <0.001 | 0.37 | 0.31 to 0.44 | <0.001 |
| Model 2a (DG‐specific risk factor level time trends)† | ||||||
| Affluent | 0.23 | 0.14 to 0.31 | <0.001 | −0.01 | −0.09 to 0.07 | 0.755 |
| 2 | 0.18 | 0.10 to 0.26 | <0.001 | 0.09 | 0.01 to 0.17 | 0.022 |
| 3 | 0.18 | 0.10 to 0.26 | <0.001 | 0.10 | 0.02 to 0.18 | 0.011 |
| 4 | 0.18 | 0.10 to 0.26 | <0.001 | 0.03 | −0.05 to 0.11 | 0.443 |
| Deprived | 0.10 | 0.02 to 0.18 | 0.020 | 0.11 | 0.03 to 0.19 | 0.005 |
| All DGs | 0.18 | 0.15 to 0.22 | <0.001 | 0.08 | 0.04 to 0.11 | <0.001 |
| Model 3a (time trend difference between incremental DGs) | ||||||
| DG × time‡ | −0.03 | −0.05 to 0.00 | 0.034 | 0.02 | 0.00 to 0.05 | 0.069 |
| Cholesterol | ||||||
| Model 1a (overall difference between incremental DGs) | ||||||
| DG trend difference* | 0.02 | 0.01 to 0.03 | <0.001 | 0.07 | 0.06 to 0.08 | <0.001 |
| Model 2a (DG‐specific risk factor level time trends)† | ||||||
| Affluent | −0.06 | −0.08 to −0.05 | <0.001 | −0.06 | −0.07 to −0.05 | <0.001 |
| 2 | −0.06 | −0.07 to −0.05 | <0.001 | −0.06 | −0.07 to −0.04 | <0.001 |
| 3 | −0.07 | −0.08 to −0.06 | <0.001 | −0.06 | −0.07 to −0.05 | <0.001 |
| 4 | −0.07 | −0.08 to −0.05 | <0.001 | −0.08 | −0.09 to −0.06 | <0.001 |
| Deprived | −0.09 | −0.10 to −0.08 | <0.001 | −0.08 | −0.09 to −0.06 | <0.001 |
| All DGs | −0.07 | −0.07 to −0.06 | <0.001 | −0.06 | −0.07 to −0.06 | <0.001 |
| Model 3a (time trend difference between incremental DGs) | ||||||
| DG × time‡ | −0.005 | −0.01 to −0.001 | 0.012 | −0.005 | −0.01 to −0.001 | 0.016 |
| Body mass index | ||||||
| Model 1a (overall difference between incremental DGs) | ||||||
| DG trend difference* | 0.11 | 0.08 to 0.14 | <0.001 | 0.39 | 0.36 to 0.43 | <0.001 |
| Model 2a (DG‐specific risk factor level time trends)† | ||||||
| Affluent | 0.12 | 0.09 to 0.16 | <0.001 | 0.10 | 0.06 to 0.14 | <0.001 |
| 2 | 0.13 | 0.10 to 0.16 | <0.001 | 0.08 | 0.04 to 0.12 | <0.001 |
| 3 | 0.08 | 0.05 to 0.11 | <0.001 | 0.14 | 0.10 to 0.18 | <0.001 |
| 4 | 0.10 | 0.06 to 0.13 | <0.001 | 0.08 | 0.04 to 0.12 | <0.001 |
| Deprived | 0.06 | 0.02 to 0.09 | <0.001 | 0.11 | 0.07 to 0.16 | <0.001 |
| All DGs | 0.10 | 0.08 to 0.11 | <0.001 | 0.11 | 0.09 to 0.13 | <0.001 |
| Model 3a (time trend difference between incremental DGs) | ||||||
| DG × time‡ | −0.02 | −0.03 to −0.01 | 0.002 | 0.01 | −0.01 to 0.02 | 0.419 |
*Model 1: effect of one group ordinal change in DG adjusted for age, survey year and DG (continuous variable); †model 2: mean annual change per survey year by DG, adjusted for age; ‡model 3: mean change between survey years and ordinal increase in DG (DG × test year) adjusted for age, survey year and DG.
Table 3 Probability of smoking by ordinal increase in deprivation group (DG) (model 1b), probability of change in current smoking status over time by DG (model 2b) and differential convergence or convergence of time trends in probability of current smoking (model 3b).
| Men | Women | |||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p Value | OR | 95% CI | p Value | |
| Model 1b (overall difference between a given DG and the one immediately more deprived) | ||||||
| DG trend difference* | 1.24 | 1.22 to 1.26 | <0.001 | 1.26 | 1.24 to 1.28 | <0.001 |
| Model 2b (trends by DG)† | ||||||
| Affluent | 0.94 | 0.93 to 0.96 | <0.001 | 0.96 | 0.94 to 0.97 | <0.001 |
| 2 | 0.94 | 0.92 to 0.96 | <0.001 | 0.97 | 0.95 to 0.99 | 0.001 |
| 3 | 0.97 | 0.95 to 0.99 | <0.001 | 0.96 | 0.94 to 0.98 | <0.001 |
| 4 | 0.96 | 0.94 to 0.98 | 0.001 | 0.95 | 0.93 to 0.97 | <0.001 |
| Deprived | 0.95 | 0.92 to 0.98 | 0.001 | 0.98 | 0.95 to 1.00 | 0.094 |
| All DGs | 0.96 | 0.95 to 0.96 | <0.001 | 0.97 | 0.96 to 0.97 | <0.001 |
| Model 3b (time trend difference between a given DG and the one immediately more deprived) | ||||||
| DG × time‡ | 1.01 | 1.00 to 1.01 | 0.020 | 1.01 | 1.00 to 1.01 | 0.016 |
*Model 1: effect of one group ordinal change in DG adjusted for age, survey year and DG (continuous variable); †model 2: mean annual change by DG adjusted for age; ‡model 3: mean change by test year and ordinal increase in DG (DG × test year) adjusted for age, test year and DG.
OR, odds ratio.
Risk factor level trends
Indicative changes between least and most deprived groups between 1989 and 1999
Table 4 shows absolute and proportional change between the least and most deprived groups between 1989 and 1999. Inequalities in current smoking levels increased during the study period for both sexes. For all other risk factors, there was a degree of reduction in inequalities in men. In women only, inequalities widened in relation to systolic and diastolic BP, although there was reduction in relation to cholesterol and BMI.
Table 4 Absolute and percentage difference in risk factor levels between study baseline (1989) and end period (1999) for most and least deprived groups and percentage ascertainment completeness along with sample size for each observation.
| Risk factor | Men | Women | |||||||
|---|---|---|---|---|---|---|---|---|---|
| 1989 | 1999 | Absolute difference | % difference | 1989 | 1999 | Absolute difference | % difference | ||
| Cholesterol | |||||||||
| Affluent | % ascertained | 46.3% | 51.8% | 43.8% | 37.6% | ||||
| Number | 327 | 114 | 355 | 79 | |||||
| Mean (mmol/l) | 5.953 | 5.700 | −0.253 | −4.3% | 5.819 | 5.356 | −0.463 | −8.0% | |
| 95% CI | 5.832 to 6.074 | 5.214 to 6.186 | 5.714 to 5.924 | 5.042 to 5.670 | |||||
| Deprived | % ascertained | 48.0% | 46.3% | 44.5% | 38.3% | ||||
| Number | 303 | 222 | 354 | 103 | |||||
| Mean (mmol/l) | 6.189 | 5.310 | −0.879 | −14.2% | 6.031 | 5.252 | −0.779 | −12.9% | |
| 95% CI | 6.050 to 6.328 | 5.145 to 5.475 | 5.924 to 6.137 | 5.026 to 5.477 | |||||
| Systolic blood pressure | |||||||||
| Affluent | % ascertained | 100% | 100% | 99.8% | 100% | ||||
| Number | 707 | 220 | 808 | 210 | |||||
| Mean (mm Hg) | 129.2 | 131.8 | 2.6 | 2.0% | 126.1 | 122.0 | 4.1 | 3.3% | |
| 95% CI | 128.1 to 130.3 | 129.6 to 134.0 | 125.0 to 127.2 | 119.3 to 124.7 | |||||
| Deprived | % ascertained | 100% | 100% | 100% | 100% | ||||
| Number | 631 | 319 | 795 | 269 | |||||
| Mean (mm Hg) | 131.3 | 129.7 | 1.6 | 1.2% | 127.6 | 126.5 | 1.1 | 0.9% | |
| 95% CI | 130.2 to 132.5 | 127.8 to 131.6 | 126.5 to 128.8 | 123.7 to 129.1 | |||||
| Diastolic blood pressure | |||||||||
| Affluent | % ascertained | 100% | 100% | 100% | 100% | ||||
| Number | 707 | 220 | 810 | 210 | |||||
| Mean (mm Hg) | 80.0 | 81.7 | 1.7 | 2.1% | 77.5 | 75.3 | 2.2 | 2.8% | |
| 95% CI | 79.3 to 80.7 | 80.1 to 83.3 | 76.9 to 78.1 | 73.7 to 76.9 | |||||
| Deprived | % ascertained | 100% | 100% | 100% | 100% | ||||
| Number | 631 | 479 | 795 | 269 | |||||
| Mean (mm Hg) | 81.7 | 80.9 | 0.8 | 1.0% | 78.6 | 79.4 | 0.8 | 1.0% | |
| 95% CI | 81.0 to 82.4 | 79.7 to 82.1 | 77.9 to 79.3 | 78.0 to 80.8 | |||||
| Body mass index | |||||||||
| Affluent | % ascertained | 58.3% | 92.3% | 56.4% | 89.5% | ||||
| Number | 412 | 203 | 457 | 188 | |||||
| Mean (kg/m2) | 25.48 | 26.79 | 1.31 | 5.1% | 24.36 | 25.32 | 0.96 | 3.9% | |
| 95% CI | 25.20 to 25.76 | 26.25 to 27.33 | 23.97 to 24.75 | 24.33 to 26.31 | |||||
| Deprived | % ascertained | 75.3% | 92.5% | 75.6% | 92.2% | ||||
| Number | 475 | 416 | 601 | 248 | |||||
| Mean (kg/m2) | 26.08 | 26.7 | 0.62 | 2.4% | 25.99 | 26.97 | 0.98 | 3.8% | |
| 95% CI | 25.72 to 26.43 | 25.68 to 26.70 | 25.54 to 26.44 | 25.99 to 27.95 | |||||
| Smoking | |||||||||
| Affluent | % ascertained | 59.0% | 92.3% | 56.5% | 85.7% | ||||
| Number | 417 | 203 | 458 | 189 | |||||
| Mean (% current smokers) | 43.0% | 24.7% | −18.3% | −42.6% | 32.4% | 12.7% | −19.7% | −60.8% | |
| 95% CI | 38.1% to 47.9% | 17.5% to 31.9% | 28.0% to 36.7% | 6.3 to 19.1 | |||||
| Deprived | % ascertained | 75.9% | 92.2% | 76.6% | 92.6% | ||||
| Number | 479 | 294 | 609 | 249 | |||||
| Mean (% current smokers) | 65.8% | 59.7% | −6.1% | −9.3% | 51.3% | 43.3% | −8% | −15.6% | |
| 95% CI | 61.4% to 70.2% | 53.3% to 66.2% | 47.4% to 55.3% | 35.4% to 51.2% | |||||
All participants
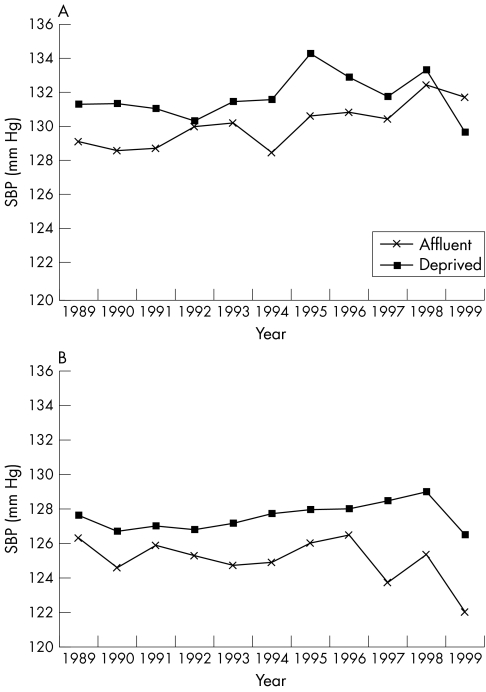
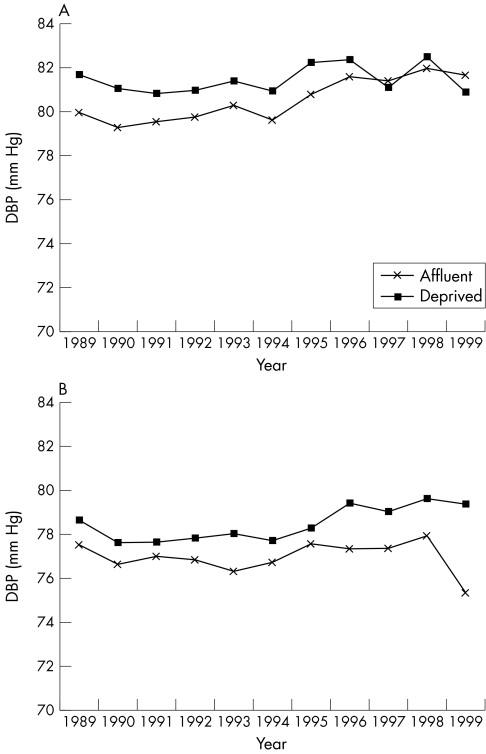
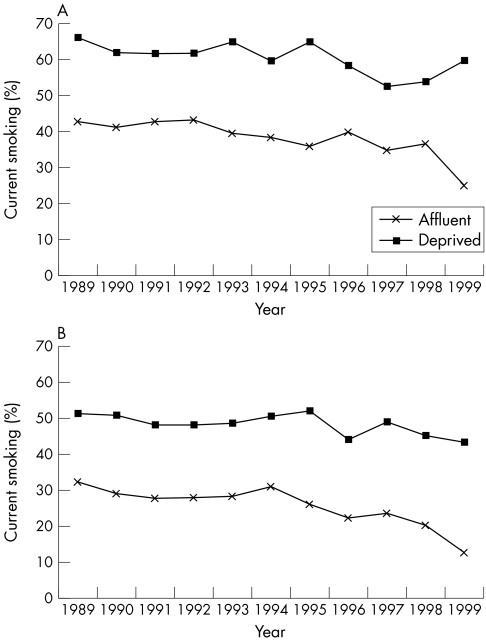
Figures 1–5 show age‐standardised risk factor trends by sex and age group. Among women of all deprivation groups significant increasing time trends in diastolic BP (0.08 mm Hg/year, 95% CI 0.04 to 0.11) and BMI (0.11 kg/m2/year, 95% CI 0.09 to 0.13) and decreasing time trends in total cholesterol (−0.06 mmol/l/year, 95% CI −0.07 to −0.06) were seen. Among men of all deprivation groups significantly increasing time trends in systolic BP (0.23 mm Hg/year, 95% CI 0.18 to 0.29), diastolic BP (0.18 mm Hg/year, 95% CI 0.15 to 0.22) and BMI (0.10 kg/m2/year, 95% CI 0.08 to 0.11) and decreasing trends in total cholesterol (−0.07 mmol/l/year, 95% CI −0.07 to −0.06) (table 2, model 2a) were seen. For smoking, overall there was a significant decreasing time trend in probability of prevalence of current smoking (OR 0.97, 95% CI 0.96 to 0.97 for women; and OR 0.96, 95 CI 0.95 to 0.96 for men) (table 3, model 2b).
Figure 1 Age‐standardised mean systolic blood pressure (SBP) in the most and least deprived groups in (A) men (−0.02 mm Hg/year/incremental deprivation group, p = 0.418) and (B) women (0.05 mm Hg/year/incremental deprivation group, p = 0.010).
Figure 2 Age‐standardised mean diastolic blood pressure (DBP) in the most and least deprived groups in (A) men (−0.03 mm Hg/year/incremental deprivation group, p = 0.034) and (B) women (0.02 mm Hg/year/incremental deprivation group, p = 0.069).
Figure 3 Age‐standardised mean cholesterol in the most and least deprived groups in (A) men (−0.005 mmol/l/year/incremental deprivation group, p = 0.012) and (B) women (−0.005 mmol/l/year/incremental deprivation group, p = 0.015).
Figure 4 Age‐standardised mean body mass index (BMI) in the most and least deprived groups in (A) men (−0.02 kg/m2/year/incremental deprivation group, p = 0.002) and (B) women (0.01 kg/m2/year/incremental deprivation group, p = 0.419).
Figure 5 Age‐standardised mean prevalence of current smoking in the most and least deprived groups in (A) men (odds ratio 1.01/year/incremental deprivation group, p = 0.020) and (B) women (OR 1.01/year/incremental deprivation group, p = 0.016).
Deprivation group trends
As indicated by a significant interaction term for deprivation group × test year among women, systolic BP increase was faster in more deprived groups (by 0.05 mm Hg/year/increasing deprivation group, or by 0.25 mm Hg/year between the least and the most deprived groups) (table 2, model 3a). For both sexes, cholesterol dropped faster in more deprived groups (by −0.005 mmol/l/year/increasing deprivation group, or −0.025 mmol/l/year between the least and the most deprived groups). For men, diastolic BP increased more slowly among more deprived groups (by −0.03 mm Hg/year /increasing deprivation group, or −0.15 mm Hg/year between the least and the most deprived deprivation groups). In men only, BMI also increased more slowly in more deprived groups (by −0.02 kg/m2/year/increasing deprivation group, or −0.1 kg/m2/year between the least and the most deprived groups). For both men and women, the current smoking status drop was slower among the most deprived groups (with the probability of current smoking status being higher by 1%/year/increasing deprivation group, or 5% between the least and the most deprived groups) (table 3, model 3b).
Sensitivity analysis
Modelling by approach 1 (confining modelling to participants aged 35–39 only) overall produced non‐significant trends due to loss of power.
Modelling by approach 2 (including a study period, 1989–93 and 1994–9, variable in modelling) produced little difference in the results obtained by models not including adjustment for study period, denoting that time trends were overall independent of study period.
Modelling by approach 3 (restricting analysis sequentially to either the 1989–93 or the 1994–9 study period) overall produced some discordant results between the two study periods, also with some null (non‐significant) trends for some risk factors and study periods due to loss of power, as with approach 1.
DISCUSSION
The findings show that in the study setting and during the whole study period 1989–99, more deprived middle‐aged people overall possessed an adverse risk factor profile compared with the least deprived group. The findings also apparently show both a similar and a dissimilar pattern of time trends in risk factor levels for the examined five risk factors between deprivation groups, with some evidence of inequality in trends, which, however, is not consistently in favour of either the least or the most deprived. Given the significant differences in risk factor level status at baseline in favour of the least deprived groups, this means that overall inequalities in cardiovascular risk factors, and ultimately cardiovascular disease, are likely to continue in the future.
Change (decrease) in cholesterol was observed to be faster among the more deprived groups for both sexes. Although the exact reasons for this observation are difficult to postulate, the finding may relate to the eventual late diffusion of more healthy dietary habits among the more deprived groups during the study period (for example, a switch to use of low fat dairy products or substitution of animal‐derived with plant‐derived fat), at the same time when the diet of the least deprived groups did not improve further. Similarly, for men only, the observed changes in BMI and BP were also in favour of the most deprived groups. This finding can also be postulated most likely to relate to the adoption during the study period of a more sedentary lifestyle and a diet higher in calories at a comparatively faster pace among the least affluent groups. The findings in general are potent reminders of the evolving nature of health inequality in cardiovascular risk factors. They also strongly advocate the use of observations spanning different time periods when studying inequality patterns and more research in time trends in inequality.
The findings confirm the strong socioeconomic pattern of cardiovascular risk factors, also observed in many other studies, including the population‐based samples of the Health Survey for England (1991–1999)1 and the Health Survey for Scotland,19 supporting the external validity of the dataset. Similarly, for cholesterol concentration, BMI and smoking status, the observed population risk factor time trends are in agreement with those observed in the population‐based samples of the Health Survey for England (1991–1999)1 and the Health Survey for Scotland,19 reflecting downward trends for cholesterol and smoking status but increasing BMI trends. The lack of any significant decreasing trends in systolic and diastolic BP is, however, in contrast to information from population‐based epidemiological surveys of high quality—for example, the Health Survey for England. This difference raises the question as to whether the difference can be due to bias, a “real” effect or chance. Selection bias is theoretically possible, as patients with a known diagnosis of hypertension and other cardiovascular conditions were excluded from the study, unlike population‐based surveys such as the Health Survey for England that randomly include such patients. For this exclusion to have been responsible for the findings, however, would mean that population levels of BP continued to rise in all participants other than those with hypertension and other cardiovascular conditions. Artefactual explanations are also likely—for example, systematic differences in measurement progressing during the study period (for example, timing allowed to achieve a resting state, body posture, observer technique and training, number of BP readings and calculation of mean values from more than one reading).
A crucial question in relation to the generalisability of the study findings is whether participants in screening were representative of the Stockport population as a whole and whether they were representative of all screening participants. Coverage estimates by deprivation group (see supplemental file 1 on the Heart website—http://www.heartjnl.com/supplemental) show overall small variation in coverage, for both 1989–93 and overall (1989–99). Similarly, there were systematic differences between participants in ascertainment completeness, mean age and proportion of participants who had their first screen in the prevalence round of the programme (table 1). Given, however, that deprivation group differences in both population coverage and data ascertainment completeness are small overall, in both absolute and relative terms, the representativeness of the study's sample is likely to be good in relation to the eligible Stockport population of 35–60 year olds. Similarly, when considering the generalisability of the study, the age of participants (35–60 years) should be borne in mind, as, for example, people older than 60 years are less healthy and may be more deprived on average. Extending the study's findings in relation to change in risk factor levels and trends in inequality to such age groups would therefore be inappropriate.
A potential limitation of the study is the use of an area‐based measure of socioeconomic status, measured at one point in time (1991). Changes in either local demography or deprivation geography may introduce misclassification error and potentially bias. Analysis of demographic and deprivation changes in the intercensus years between 1991 and 2001 has provided evidence of a trivial degree of change.20 We therefore believe that these factors have not biased the results. It should also be noted that about two thirds of the data relate to the period 1989–93—that is, near the census year. Other limitations are the relatively incomplete ascertainment for some risk factors (BMI, smoking and, particularly, cholesterol) and the potential for risk measurement errors, which due to the non‐research design of the study can be considered substantial.
As described, participants in the 1989–93 study period were significantly older and less deprived than the participants in the 1994–9 period. Nevertheless, adjustment for age (which is a feature of all analyses presented here) and adjustment or restriction for deprivation group (which also is a feature of all analyses) can be expected to account for a large amount of potential bias that could have been introduced by this factor. Moreover, the sensitivity analysis approaches used overall failed to provide significant results that could have pointed to alternative time trends. Lastly, visual inspection of the mean values for each year (1989–99) did not detect any apparent “step” effect between study periods. We therefore believe that the main approach used (analysing all study years together, and adjusting for age and deprivation) was the best method to analyse the dataset in a valid and informative way.
Socioeconomic status can be measured directly (by measuring a person's income, occupation or education) or indirectly by using area‐based measures (based on the predominant characteristics of the population of a small area).21 An area‐based measurement (Townsend deprivation score) was used in this study, in common with other previous UK research in the field of socioeconomic inequalities in health, because information about individual measures of socioeconomic status of participants was incomplete and potentially inaccurate. Although in theory the use of a direct individual marker of socioeconomic status may have been preferable, area‐based UK deprivation indices have been shown to predict poor health outcomes at the individual level,22 including coronary heart disease.23 If full account had been taken of both individual socioeconomic status and deprivation status, socioeconomic differences in risk factor levels would possibly have been even higher, as deprivation is a significant predictor of cardiovascular disease risk, even after adjustment for socioeconomic status measured individually.3 Although Stockport as a whole is more deprived than England and Wales, the range of Townsend deprivation score among study participants was large and comparable with the national range.
Prospective use of routinely collected data has been advocated as a method to help support surveillance and monitoring of risk factor trends in the population.24 Our analysis proves that indeed there is a very important potential for using data relating to the first screening assessment in the Stockport cardiovascular risk factors screening programme, both historically (prospectively) and at present. Information about the studied population could have been of use to health promotion and public health initiatives, at least locally and probably nationally, and could have similarly been used to further inform prospective and timely estimation of the population impact of changes in risk factors. It is of note that population‐based data on trends of total cholesterol were not available in the Health Survey for England until 1993, and between 1989–99 such data from the same source are available for only five of the 11 years during 1989–99.
Conclusion
This study provides further evidence that socioeconomic status (measured in this instance with small area deprivation) has an independent effect on the level of exposure to conventional cardiovascular risk factors. Changes in risk factor levels by deprivation group over time differed and were associated with both widening and narrowing of inequalities. This means that overall historical and current inequalities in cardiovascular risk factor levels (and ultimately cardiovascular disease) are likely to persist. The use of routinely available data for monitoring of population trends is supported.
Supplemental files 1 and 2, including tables, appear on the Heart website—http://www.heartjnl.com/supplemental
Supplementary Material
ACKNOWLEDGEMENTS
Thanks to Professor Deborah Baker, Dr Stephen Watkins, Ms Jane Jefferson, Ms Jane Pilkington, Dr Gill Greenhough, Ms Jane Bowdenleigh, Dr Gill Burroughs, Ms Bernadette Ryan‐Wooley, Ms Barbara Shallaker, Mr Dan Byrne and Ms Eleanor Bannister.
Footnotes
Competing interests: None declared.
Supplemental files 1 and 2, including tables, appear on the Heart website—http://www.heartjnl.com/supplemental
References
- 1.British Heart Foundation Deaths by cause, men, 2002, United Kingdom. British Heart Foundation statistics website. http://www.heartstats.org/uploads/documents/Fig%201.3a%20web04.xls (accessed 29 Mar 2006)
- 2.McPherson K, Britton A, Causer L.Coronary heart disease: estimating the impact of changes in risk factors. London: The Stationery Office, National Heart Forum, 2002
- 3.Sundquist K, Malmstrom M, Johansson S‐E. Neighbourhood deprivation and incidence of coronary heart disease: a multilevel study of 2.6 million women and men in Sweden. J Epidemiol Community Health 20045871–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shohaimi S, Luben R, Wareham N.et al Residential area deprivation predicts smoking habit independently of individual educational level and occupational social class: a cross sectional study in the Norfolk cohort of the European Investigation into Cancer (EPIC‐Norfolk). J Epidemol Community Health 200358270–276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Unal B, Critchley J A. Capewell S. Explaining the decline in coronary heart disease mortality in England and Wales between 1981 and 2000. Circulation 20041091101–1107. [DOI] [PubMed] [Google Scholar]
- 6.Critchley J A, Capewell S. Substantial potential for reductions in coronary heart disease mortality in the UK through changes in risk factor levels. J Epidemiol Community Health 200357243–247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Capewell S, Morrison C E, McMurray J J. Contribution of modern cardiovascular treatment and risk factor changes to the decline in coronary heart disease mortality in Scotland between 1975 and 1994. Heart 199981380–386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ebrahim S, Smith G D. Systematic review of randomised controlled trials of multiple risk factor interventions for preventing coronary heart disease. BMJ 19973141666–1674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Department of Health Choosing health: making healthy choices easier. London: HMSO, 2004, http://www.dh.gov.uk/PublicationsAndStatistics/Publications/PublicationsPolicyAndGuidance/PublicationsPolicyAndGuidanceArticle/fs/en?CONTENT_ID = 4094550&chk = aN5Cor (accessed 29 Mar 2006)
- 10.Edgar M A, Schneiden H. The economics of mild hypertension programmes. Soc Sci Med 198928211–222. [DOI] [PubMed] [Google Scholar]
- 11.Lyratzopoulos G, McElduff P, Heller R F.et al Mid‐term body mass index increase among obese and non‐obese individuals in middle life and deprivation status: A cohort Study. BMC Public Health 2005532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bartys S, Baker D, Lewis P.et al Inequity in recording of risk in a local population‐based screening programme for cardiovascular disease. Eur J Cardiovasc Prev Rehab 20051263–67. [PubMed] [Google Scholar]
- 13.Lyratzopoulos G, McElduff P, Heller R F.et al Comparative levels and time trends in blood pressure, total cholesterol, body mass index and smoking among Caucasian and South‐Asian participants of a UK primary‐care based cardiovascular risk factor screening programme. BMC Public Health 200528125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Office for National Statistics Compendium of clinical indicators, 1998–2000. London: HMSO, 2001
- 15.Townsend P, Phillimore P, Beattie A.Health and deprivation: inequality and the north. London: Croom Helm, 1988
- 16.Armitage P, Berry G.Statistical methods in medical research. 3rd ed. Oxford: Blackwell Scientific Publications, 1994
- 17.Anand S S, Yusuf S, Vuksan V.et al Differences in risk factors, atherosclerosis, and cardiovascular disease between ethnic groups in Canada: the study of health assessment and risk in ethnic groups (SHARE). Lancet 2000356279–284. [DOI] [PubMed] [Google Scholar]
- 18.Cappuccio F P, Cook D G, Atkinson R W.et al Prevalence, detection, and management of cardiovascular risk factors in different ethnic groups in south London. Heart 199778555–563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shaw A, McMunn A, Field J. eds. The Scottish Health Survey 1998. http://www.show.scot.nhs.uk/scottishhealthsurvey/sh8‐00.html (accessed 29 Mar 2006)
- 20.Office for National Statistics Stockport. Census 2001. Office for National Statistics. http://www.statistics.gov.uk/census2001/profiles/00bs.asp (accessed 29 Mar 2006)
- 21.Liberatos P, Link B G, Kelsey J L. The measurement of social class in epidemiology. Epidemiol Rev 19881087–121. [DOI] [PubMed] [Google Scholar]
- 22.Carstairs V. Deprivation indices: their interpretation and use in relation to health. J Epidemiol Community Health 199549(Suppl 2)S3–S8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Woodward M. Small area statistics as markers for personal social status in the Scottish Heart Health study. J Epidemiol Community Health 199650570–576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bundred P, Kitchiner D, Buchan I. Prevalence of overweight and obese children between 1989 and 1998: population based series of cross sectional studies. BMJ 2001322326–328. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.