Abstract
Objective
To investigate dilatory changes of the aorta distal to the root in patients with Marfan's syndrome.
Methods and results
Data of 268 patients with Marfan's syndrome who were enrolled in the Euro Heart Survey on adult congenital heart disease were analysed. Data used for this study were baseline characteristics, diameters at four levels of the aorta and events during follow up (dissection, aortic repairs and death). At inclusion, 26 patients had a previous dissection and 53 patients without a previous dissection had undergone elective aortic repair, thus leaving 189 patients without previous dissection or repair. During follow up (median 5.4 years), four patients died. A total of 46 aortic events (dissection or elective surgery) occurred in 45 patients, in the distal aorta in 14 patients (31%). Baseline aortic diameter at the levels distal to the root (arch, descending aorta and abdominal aorta) was greater in patients with than in those without a previous elective aortic root intervention (median 26 mm v 24 mm, p = 0.01; 25 mm v 20 mm, p < 0.01; and 20 mm v 17 mm, p < 0.01, respectively). Multivariate analysis showed that a previous elective aortic intervention was associated with a fourfold increased probability of dilatation of the distal aorta, after adjustment for age and sex (p < 0.01). In patients without a previous intervention, the baseline diameter of the descending aorta was an independent predictor of aortic events (hazard ratio 3.0 per quartile, 95% CI 1.5 to 5.9, p = 0.002). Cause for concern is that complete measurements of the aorta (at least one measurement at each level at baseline or during follow up) were available for only 38% of the patients.
Conclusions
Almost one in every three aortic events occurring during follow up of these patients involved the distal aorta. After elective aortic root replacement, a dilated distal aorta is more common than before. Moreover, an increased diameter of the descending aorta is associated with a higher risk of aortic events in patients without previous dissection or aortic root replacement, independent of the diameter of the aortic root. Careful monitoring of the entire aorta is essential for the optimal management of patients with Marfan's syndrome, especially after elective surgery, but is insufficiently performed in Europe.
Prevention of aortic dissection is one of the cornerstones of the clinical care of patients with Marfan's syndrome.1 Abnormal fibrillin protein, which results from the genetic defect that causes this disease, gives rise to a pathological aortic wall, especially of the proximal aorta. Dissection is usually preceded by aortic dilatation. As timely replacement of the aortic root has been shown to reduce the risk of dissection,2,3,4,5 measurement of aortic diameters at regular intervals, in particular of the aortic root, has become a strongly recommended strategy of management.6,7 Prolonged survival after aortic root replacement has led to an increase in the number of patients with aortic complications beyond the root.8 As patient numbers are relatively small and randomised studies are not feasible, evaluation of the results of treatment remains difficult. The recently completed Euro Heart Survey on adult congenital heart disease included a considerable number of patients with Marfan's syndrome and provided a unique opportunity to study aortic complications and their prevention in a broad setting. We present the findings in this international patient population regarding monitoring of aortic diameters, preventive repairs and outcomes. Special attention is given to the measurement of the distal parts of the aorta, which has hitherto been relatively neglected.
METHODS
All patients who had Marfan's syndrome as the main diagnosis were selected from the database of the Euro Heart Survey on adult congenital heart disease. The methods that were used to collect the data for this survey have been described previously.9 Briefly, consecutive patients with one of eight congenital cardiac defects visiting an outpatient clinic of one of the participating centres in 1998 were identified, and their clinical course was documented in retrospect until April 2004. Data on medical history and results of diagnostic procedures and interventions were transcribed from patient records on to an electronic case record file. All data were entered anonymously by local investigators. Where required, approval of the local ethics committee was obtained.
For this analysis, the following data collected for patients with Marfan's syndrome in the survey were used: general patient information (age, sex); presence of diagnostic criteria for Marfan's syndrome; medical history of dissections (type A/B), interventions pertaining to the aorta or mitral valve and arrhythmias; aortic diameters, as measured by echocardiography, magnetic resonance imaging or computed tomography at four levels (aortic root, aortic arch, descending aorta and abdominal aorta); and events during follow up (death, the occurrence of dissection or aortic interventions).
An aortic event is defined as either an aortic dissection or elective surgery of the aorta. Elective surgery is surgery not performed because of actual or imminent dissection.
To avoid referral bias, a period of at least three months was required between study inclusion and any interventions during follow up.
Definition of the three groups of patients
Patients were divided into the following three groups for analysis: (1) patients without a history of dissections or elective aortic surgery at baseline; (2) patients without a history of dissection, but with previous elective aortic surgery; and (3) patients with a history of dissection (with or without previous aortic surgery).
Statistical analysis
Categorical baseline characteristics were expressed as percentages or counts and compared between (two of the three) groups by Pearson's χ2 test. Continuous variables were expressed as mean (SD) and compared by the two‐tailed t test for independent samples when appropriate or, when not normally distributed, as median (interquartile range) compared by a non‐parametric method. Values of p < 0.05 were considered significant.
The occurrence of events during follow up was assessed with survival analysis. In addition, absolute figures and percentages were given.
Elective repair of the aortic root and dilatation at levels beyond the root
Univariate logistic regression analysis was performed to study the relationship between previous elective repair of the aortic root and the presence of an enlarged aorta at levels beyond the root. Furthermore, multivariate analysis was used to adjust for non‐comparable baseline characteristics between patients with and without previous elective surgery. The outcome (dependent) variable for this analysis was defined as a baseline aortic diameter in the upper quartile (25% greatest diameters) at any level distal to the aortic root. Odds ratios and corresponding 95% confidence intervals (95% CIs) were calculated as an estimate of the relative risk associated with the variables of interest.
Patients with a previous dissection or with previous elective surgery involving the distal aorta were excluded from this analysis.
Baseline characteristics as predictors of events in patients without previous dissection or elective aortic surgery
Cox regression analysis was used to investigate the association between baseline characteristics and outcomes in the group of patients without a history of dissection or elective aortic repair. Various alternative end points were considered as the basis for this analysis, in particular death, dissection, elective aortic surgery and combinations of these. Univariate analysis was used to identify potential predictors. Hazard ratios were calculated together with a 95% CI as an estimate of the risk associated with the particular variable. The variables with a p < 0.1 were selected for multivariate analysis. The resulting multivariate model was derived by a forward stepwise algorithm, with comparison of likelihood ratio as criterion for model selection and with retention of variables with p < 0.1 in the model.
Lastly, the relation between one of the identified predictors (the diameter of the descending aorta) and the occurrence of events during follow up was investigated in this group of patients by the Kaplan–Meier method. For this purpose, patients were divided into quartiles (on the basis of diameter size).
Data were analysed with the SPSS package V.12.01 (SPSS Inc, Chicago, Illinois, USA).
RESULTS
The Euro Heart Survey collected data on 287 patients with Marfan's syndrome from 44 centres (35 tertiary referral centres) in 21 countries. For the present analyses, 19 patients were excluded for one of two reasons: either the patient was operated on within three months after inclusion (n = 14) or essential data were lacking (n = 5). Thus, 268 patients were studied for a median follow up of 5.4 years, constituting a total of 1303 patient years.
Measurements of the aortic root diameter at baseline were available for 96% (n = 182) of the patients without a history of dissection or elective intervention. Measurements at all aortic levels were available for only 29% (n = 54) of the patients in this group at baseline, however, and for 38% (n = 71) of patients for the whole follow‐up period (at least one measurement at each level at baseline or during follow up). Among patients with a previous elective aortic intervention, complete measurements of the distal aorta were available for only 23% (11 of 47, disregarding six patients with previous elective surgery of the distal aorta).
Comparison of baseline characteristics
Table 1 lists baseline characteristics of each of the three groups. Patients without a previous aortic intervention or dissection were younger, and more of those who had undergone elective aortic surgery were men. Because of outlying values, diameters were expressed as medians (interquartile range), and group differences were assessed with a non‐parametric method (Mann–Whitney test). Diameters at the level of the arch, descending aorta and abdominal aorta were significantly greater in the patients with than in those without previous elective aortic repair (see further below).
Table 1 Baseline characteristics of 268 patients with Marfan's syndrome.
| No dissection or aortic repair (n = 189) | Elective aortic repair (n = 53) | Dissection (type B: n = 2) (n = 26) | p Value* | ||
|---|---|---|---|---|---|
| Age (years) | 30 (11) | 36 (13) | 35 (10) | ||
| Women (n = 139) | 60% | 32% | 39% | ||
| Ever pregnant (n/m)** | 48% (53/110) | 31% (5/16) | 44% (4/9) | ||
| Mutations | |||||
| Yes | 52 | 12 | 8 | ||
| No | 60 | 19 | 5 | ||
| Unknown | 74 | 21 | 13 | ||
| Mitral valve intervention | 3 (2%) | 6 (11%) | 1 (4%) | ||
| Arrhythmias | 17 (9%)) | 6 (11%) | 5 (19%) | ||
| β blockers | 94 (50%) | 28 (53%) | 16 (62%) | ||
| Aortic diameter (mm) | |||||
| Root | n = 182† | 40 (36–45) | NA | ||
| Arch | n = 112,18,13† | 24 (22–27) | 26 (24–30)‡ | 27 (23–41)§ | 0.014 |
| Descending | n = 83,15,11† | 20 (18–22) | 25 (20–28)‡ | 30 (26–42)§ | 0.003 |
| Abdominal | n = 76,21,11† | 17 (15–19) | 20 (18–23)‡ | 30 (27–40)§ | 0.003 |
Age is reported as mean (SD); aortic dimensions as medians (interquartile range).
*Patients without dissection or aortic repair compared with patients with an elective aortic repair; †numbers of patients in each of the groups for whom data were available, enumerated in the same order as the columns of the table: no dissection, elective surgery, dissection; ‡patients who had undergone an aortic intervention in another part than the root (n = 6) were excluded in calculating these averages; §one patient who had undergone surgery of the distal aorta was excluded; **The denominator “m” refers to the numbers of patients for whom data on pregnancy were available.
Events
Table 2 shows the events occurring during follow up in each of the three defined groups. Overall, four patients died (two died of cardiovascular causes). Forty‐five patients had 46 aortic events (see Methods), involving the distal aorta in 14 of these patients (31%). Of those 46 events, 34 (7 dissections and 27 elective repairs) occurred in 33 patients without previous dissection or elective surgery at baseline. Six of these 34 events (18%) involved the distal aorta. Elective aortic repair of the distal aorta concerned the abdominal aorta in two patients, both of whom had undergone previous elective aortic surgery. Three other patients in that group had undergone surgery of the abdominal aorta before study inclusion.
Table 2 Numbers of events occurring during follow up.
| No dissection or aortic repair (n = 189)* | Elective aortic repair (n = 53)* | Dissection (n = 26)* | |
|---|---|---|---|
| Death | 1 | 1 | 2 |
| Aortic events | |||
| Dissection | 7 | 2 | 2 |
| Type A | 4† | 0 | 0 |
| Type B | 3 | 2 | 2‡ |
| Elective aortic repair | 27 | 6 | 2 |
| Aortic root | 24 | 4§ | 0 |
| Distal aorta | 3 | 2 | 2 |
*In these groups, 8, 2 and 0 patients were referred to another centre at some point during follow up and their further fate is not known; †one patient experienced a type A dissection, later followed by a type B dissection and this patient is counted twice; ‡one of these two patients died later and is thus counted twice; §one patient underwent repeat surgery of the ascending aorta and died later and this patient is counted twice.
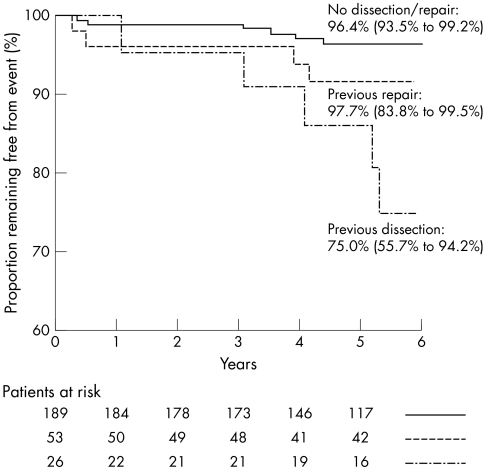
Figure 1 displays survival curves for the occurrence during follow up of aortic events in the distal aorta. Kaplan–Meier estimates for the proportions of patients experiencing such an event were 3.6% (95% CI 0.8% to 6.5%) for the group without previous dissection or surgery, 8.3% (95% CI 0.5% to 16.2%) for the group who had undergone previous elective surgery, and 25% (95% CI 5.8% to 44.3%) for the group with previous dissection. Risk was significantly different when pooled over the three groups (p = 0.002). The difference between the group with previous elective surgery and the group without previous surgery or dissection did not reach significance (p = 0.169).
Figure 1 Survival free from an event (dissection or surgery) in the distal aorta.
Elective repair of the aortic root and dilatation at levels beyond the root
Table 3 shows the percentages of patients meeting the criterion for distal aortic dilatation (a diameter in the upper quartile at one of the three distal levels), according to sex, age group and history of elective root repair. Table 3 shows that previous elective repair of the aortic root increased almost fivefold the prevalence of an enlarged distal aorta. When this association was adjusted for sex and age, it remained significant (odds ratio 3.87, p = 0.005). Cut points for stratifying patients into the upper quartile based on aortic diameters (greatest 25%) were 28 mm for the arch, 24 mm for the descending aorta, and 20 mm for the abdominal aorta. Six patients were excluded because previous elective surgery had involved the distal aorta.
Table 3 Presence of an enlarged aortic diameter relative to baseline characteristics.
| Characteristic | Odds ratio (95% CI) | p Value† | |||
|---|---|---|---|---|---|
| Present* | Absent* | Univariate | Multivariate | ||
| Previous elective aortic repair | 70% | 33% | 4.75 (1.92 to 11.72) | 3.87 (1.49 to 10.05) | 0.005 |
| Female sex | 33% | 48% | 0.55 (0.29 to 1.04) | 0.69 (0.34 to 1.42) | 0.313 |
| Age >40 years | 52% | 37% | 1.84 (0.85 to 4.00) | 1.72 (0.75 to 3.96) | 0.201 |
*The percentages represent proportions of patients with an aortic diameter in the upper quartile (greatest 25%) at any one of the levels of the arch, descending aorta or abdominal aorta (patients with previous dissections or interventions distal to the ascending aorta were excluded); †for the multivariate model.
Baseline characteristics as predictors of events in patients without previous dissection or elective aortic surgery
Univariate analysis with the composite end point of death, dissection or elective aortic surgery showed that aortic root diameter per quartile, descending aorta diameter per quartile and female sex were significant (p < 0.1). In the final multivariate model, only aortic root diameter (hazard ratio 2.5 per quartile, 95% CI 1.4 to 4.5, p = 0.002) and descending aorta diameter (hazard ratio 3.0 per quartile, 95% CI 1.5 to 5.9, p = 0.002) remained as independent predictors of the composite end point. When aortic root interventions alone were analysed as the end point, the diameter of the descending aorta remained a significant independent predictor (hazard ratio 2.534, p = 0.015 in a multivariable model that included the root diameter). Events were insufficient for an analysis of the end point death or dissection.
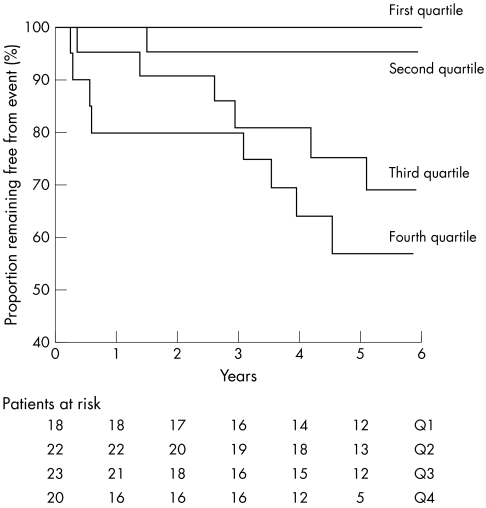
As the diameter of the descending aorta was identified as an important predictor of events, this relationship was further investigated. Figure 2 shows Kaplan–Meier curves that relate the occurrence of events during follow up to the diameter of the descending aorta. Starting with the smallest diameters (first quartile), the risk is seen to increase for each subsequent stratum (p < 0.001). The figure suggests that the major divide is between the second and third quartiles (cut point 20 mm).
Figure 2 Survival free from an event (dissection or surgery) per quartile (Q) (fourth quartile comprises the 25% greatest diameters) among patients without previous dissection or elective surgery.
DISCUSSION
Elective repair of the aortic root has greatly improved the survival of patients with Marfan's syndrome. Disease in the aorta distal to the root, however, remains a cause for concern. To our knowledge, this is the first study to establish that the diameter of the distal aorta is greater in patients who have undergone elective aortic root surgery than in patients without such intervention. Moreover, a greater diameter of the descending aorta was associated with a substantially higher risk of aortic events (dissections or elective aortic surgery). The distal aorta was the site of almost one in three of the aortic events observed in the follow‐up period, which emphasises the importance of surveillance of the entire aorta for dilatory changes. According to our findings, the distal aorta is not being sufficiently monitored.
Survival and events
Given the relatively large number of patients and participating centres, this study provides a broad view of the current treatment and outcomes of patients with Marfan's syndrome in Europe. The relevant guidelines for the prevention of aortic dissection recommend measuring the diameter of the aortic root and intervening when the root diameter has reached a threshold (50 mm or 55 mm, depending on additional factors).6,7 Our study shows that monitoring of the aortic root and preventive aortic root replacement have, indeed, been widely implemented throughout Europe. The success of this strategy may be inferred from the relatively low rate of major events (death, dissection) among the patients without previous dissection in the more than five years of follow up covered by this survey. Comparing these findings with the era before the introduction of aortic root replacement techniques is difficult, however, as outcome data from that period are lacking.10 Survival after aortic root replacement was certainly not worse in our study than in studies reported by others.2,3,4,5
Despite the greatly improved outcomes, aortic complications continue to occur, both before and after aortic root interventions.2,3,4,5,8 A dissection may disrupt the root before the threshold for intervention has been reached or complications may arise in the distal part of the aorta. After surgery, many patients need second surgeries for aneurysms or dissections at sites other than that of the first intervention.4,8 In fact, Marfan's syndrome may affect any vessel in which elastin fibres are an important structural component of its wall. This applies to the entire aorta, although elastin is found in diminishing quantities from its proximal to its distal part.11 In our study, of all aortic events observed during follow up, almost one in three occurred in the distal aorta.
Patients without previous dissection or elective surgery: first aortic events and distal aortic diameter
The distal aorta may be the site of first complications, as Finkbohner et al4 reported was the case in 16% of their patients. In our study, the first aortic event occurred in the distal aorta in 18% of the patients. The significance of the distal aorta further emerged in our investigation of factors associated with the risk of aortic complications. An increased diameter of the proximal aorta is widely known to be the strongest predictor of adverse outcome. Nollen et al12 have recently drawn attention to the importance of the descending aorta by showing that reduced distensibility of the descending thoracic aorta is a predictor of progressive dilatation of the descending thoracic aorta. To this, we add the observation that an increased diameter of the distal aorta is associated with a higher risk of aortic events, even when events in the distal aorta are excluded.
The distal aorta after elective aortic root replacement
The diameter of the distal aorta was greater in patients who had undergone elective aortic root surgery than in those who had not. The patients in the operated group were also older and more of them were men, both of which are factors known to be associated with a greater diameter.13 Yet multivariate analysis showed that after adjustment for age and sex previous elective aortic surgery was still significantly associated with a greater distal aortic diameter.
This finding may be clarified in two ways. The most obvious explanation is that patients who undergo elective surgery (the aortic root having reached the threshold) simply have a more advanced stage of the disease. Another possibility is that an intervention at the level of the root has an impact on the more distal aorta (for example, as a result of haemodynamic factors or altered wall mechanics, or because of clamping of the aorta during the operation). In an earlier study we did not find differences in the elasticity of the distal aorta between patients with and those without previous elective aortic root surgery.14
Elective replacement of the aortic root removes the most important predilection site for aneurysms, but the distal aorta remains at risk. The rate of events in the distal aorta in patients with previous elective aortic surgery was double that of patients without this surgery. Numbers were too small to reach significance. This finding should be seen, however, in the light of the increased diameter of the distal aorta in this group. In patients without previous dissection or elective surgery, an increased diameter of the distal aorta was clearly associated with an increased risk of aortic events (see above). We believe it is important to emphasise that the implication of these findings is that, after aortic root replacement, the distal aorta is at greater risk than the distal aorta in patients who have not (yet) undergone elective surgery.
Medical practice
Data on aortic diameters at all levels were not available for all patients. As several authors have stressed the importance of monitoring the entire aorta, it is certainly disappointing that this is apparently not being done consistently. Even for patients with previous aortic root surgery, information on the condition of the remaining native aorta was often lacking. It should be noted, however, that the guidelines on threshold diameters for the distal aorta are vague.6,7 Several imaging studies have reported average aortic diameters obtained by various modes of imaging (echocardiography, magnetic resonance imaging and computed tomography),15,16,17,18,19 but these provide an insufficient basis on which to derive reference values for this patient population. For this study, we defined dilatation in a relative sense, by considering quartiles.
Our observation that disease of the distal aorta is substantial reinforces the proposal that incorporating the entire thoracic and abdominal aorta in the follow‐up programme may be important to further improve outcomes. It certainly seems essential to image the remaining part of the aorta at regular intervals after aortic root replacement. This will require developing a consensus on thresholds for the diameter of the distal aorta, which could lead to specific guidelines.
Sex
A finding deserving separate comment is that men were overrepresented in the group of patients with a previous intervention. This male predominance is in line with recent findings that the aortic (root) diameter in men is about 5 mm greater than in women, at any age.13 Hence, relatively more men reach the threshold for elective intervention.
Limitations
This was a retrospective study, based on aortic measurements taken in different centres by different methods. Imaging modalities comprised echocardiography, magnetic resonance imaging and computed tomography, and the exact planes through the aorta at which the diameters of the four respective levels were measured are uncertain. It should be noted, however, that aortic diameters measured by various imaging modes have generally been found to correlate well.20 Furthermore, as all patients were followed up regularly and the primary purpose of imaging the aorta was to detect dilatation, we may assume that in most cases the diameter was measured at the plane of greatest cross section. As measurements were done as part of routine monitoring, missing values probably did not lead to systematic bias. Unless a dissection occurs, aortic dilatation is asymptomatic and there is no reason for preferential imaging of some of the patients over others. In principle, patients with previous aortic surgery may be expected to have been under greater surveillance during follow up. We found no evidence, however, that more of these patients were being treated at a referral centre than were patients without previous surgery or dissection (86% v 87%), or that fewer of them had missing data on the distal aorta.
Leaving aside the question of bias, we cannot exclude that the lack of many measurements could have led to underestimation of the frequency of disease of the distal aorta.
A final issue requiring comment is the absence of data on body size and body surface area. We do not believe that this was of much consequence, as several studies have shown that, after adjustment for age and sex, the effects of these variables on aortic diameter are negligible.21,22,23
Conclusion
Monitoring of aortic root diameter and prophylactic repair when the diameter reaches a threshold has become a widely established practice in the care of patients with Marfan's syndrome. Deaths caused by dissections starting in the aortic root have become rare. Disease of the aorta distal to the root, however, remains a cause for concern. Almost one in every three events occurring during follow up in this study involved the distal aorta. Patients who have undergone elective surgery have a larger distal aorta diameter. Moreover, the greater the diameter of the descending aorta, the higher the risk. Careful monitoring of the entire aorta is therefore essential for optimal management of patients with Marfan's syndrome but is insufficiently performed in Europe.
References
- 1.Milewicz D M, Dietz H C, Miller C. Treatment of aortic disease in patients with Marfan syndrome. Circulation 2005111e150–e157. [DOI] [PubMed] [Google Scholar]
- 2.Gott V L, Greene P S, Alejo D E.et al Replacement of the aortic root in patients with Marfan's syndrome. N Engl J Med 19993401307–1313. [DOI] [PubMed] [Google Scholar]
- 3.Gott V L, Cameron D E, Alejo D E.et al Aortic root replacement in 271 Marfan patients: a 24‐year experience. Ann Thorac Surg 200273438–443. [DOI] [PubMed] [Google Scholar]
- 4.Finkbohner R, Johnston D, Crawford E S.et al Marfan syndrome: long‐term survival and complication after aortic aneurysm repair. Circulation 199591728–733. [DOI] [PubMed] [Google Scholar]
- 5.Groenink M, Lohuis T A J, Tijssen J P G.et al Survival and complication free survival in Marfan's syndrome: implications of current guidelines. Heart 199982499–504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Therrien J, Gatzoulis M, Graham T.et al Canadian Cardiovascular Society Consensus Conference 2001 update: recommendations for the management of adults with congenital heart disease. Part II. Can J Cardiol 2001171029–1050. [PubMed] [Google Scholar]
- 7.Task Force on the Management of Grown Up Congenital Heart Disease of the European Society of Cardiology Management of grown up congenital heart disease. Eur Heart J 2003241035–1084. [DOI] [PubMed] [Google Scholar]
- 8.Carrel T, Beyeler L, Schnyder A.et al Reoperations and late adverse outcome in Marfan patients following cardiovascular surgery. Eur J Cardiothorac Surg 200425671–675. [DOI] [PubMed] [Google Scholar]
- 9.Engelfriet P, Boersma E, Oechslin E.et al The spectrum of adult congenital heart disease in Europe: morbidity and mortality in a 5 year follow‐up period. Eur Heart J 2005262325–2333. [DOI] [PubMed] [Google Scholar]
- 10.Silverman D I, Burton K J, Gray J.et al Life expectancy in the Marfan syndrome. Am J Cardiol 199575157–160. [DOI] [PubMed] [Google Scholar]
- 11.Halloran B G, Davis V A, McManus B M.et al Localization of aortic disease is associated with intrinsic differences in aortic structure. J Surg Res 19955917–22. [DOI] [PubMed] [Google Scholar]
- 12.Nollen G J, Groenink M, Tijssen J G P.et al Aortic stiffness and diameter predict progressive aortic dilatation in patients with Marfan syndrome. Eur Heart J 2004251146–1152. [DOI] [PubMed] [Google Scholar]
- 13.Meijboom L J, Timmermans J, Zwinderman A H.et al Aortic root growth in men and women with the Marfan's syndrome. Am J Cardiol 2005961441–1444. [DOI] [PubMed] [Google Scholar]
- 14.Nollen G J, Meijboom L J, Groenink M.et al Comparison of aortic elasticity in patients with the Marfan syndrome with and without aortic root replacement. Am J Cardiol 200391637–640. [DOI] [PubMed] [Google Scholar]
- 15.Aronberg D J, Glazer H S, Madsen K.et al Normal thoracic aortic diameters by computed tomography. J Comput Assist Tomogr 19848247–250. [PubMed] [Google Scholar]
- 16.Garcier J M, Petitcolin V, Filaire M.et al Normal diameter of the thoracic aorta in adults: a magnetic resonance imaging study. Surg Radiol Anat 200325322–329. [DOI] [PubMed] [Google Scholar]
- 17.Rizzo J A, Coady M A, Elefteriades J A. Procedures for estimating growth rates in thoracic aortic aneurysms. J Clin Epidemiol 199851747–754. [DOI] [PubMed] [Google Scholar]
- 18.Horejs D, Gilbert P M, Burstein S.et al Normal aortoiliac diameters by CT. J Comput Assist Tomogr 198812602–603. [DOI] [PubMed] [Google Scholar]
- 19.Benachenhou K, Azarnouch K, Filaire M.et al Evolution of healthy thoracic aortic segment diameter during follow‐up of patients with aortic aneurysm or dissection: a magnetic resonance imaging study. Surg Radiol Anat 200527142–146. [DOI] [PubMed] [Google Scholar]
- 20.Dinsmore R E, Liberthson R R, Wismer G L.et al Magnetic resonance imaging of thoracic aortic aneurysms: comparison with other imaging methods. Am J Roentgenol 1986146309–314. [DOI] [PubMed] [Google Scholar]
- 21.Hager A, Kaemmerer H, Rapp‐Bernhardt U.et al Diameters of the thoracic aorta throughout life as measured with helical computed tomography. J Thorac Cardiovasc Surg 20021231060–1066. [DOI] [PubMed] [Google Scholar]
- 22.Aronberg D J, Glazer H S, Madsen K.et al Normal thoracic aortic diameters by computed tomography. J Comput Assist Tomogr 19848247–250. [PubMed] [Google Scholar]
- 23.Reed C M, Richey P A, Pulliam D A.et al Aortic dimensions in tall men and women. Am J Cardiol 199371608–610. [DOI] [PubMed] [Google Scholar]