The reasons why some apparently healthy people experience sudden and unpredictable fainting attacks remain unclear, although predisposing factors include small blood or plasma volumes, less efficient reflex vasoconstriction and less effective cerebrovascular autoregulation.1 Recently we studied some asymptomatic volunteers who, despite never fainting, had poor tolerance to an orthostatic stress test.2 These subjects had greater postural sway during normal standing than those with good orthostatic tolerance (OT). We suggested that the subjects with poor measured OT who did not normally faint compensated for their poor reflex responses by greater postural sway. This would cause enhanced muscle pumping, thereby reducing venous pooling and preventing fainting during normal standing but not during the orthostatic stress test.
In this study we measured postural sway in patients with posturally related syncope (PRS) who had poor measured OT but without discernable cardiovascular or neurological abnormality. We compared their results with those previously published in two groups of volunteers: with good and with poor OT. Our hypothesis was that postural sway in patients with PRS, unlike non‐fainting controls with poor OT, would not be greater than that of the controls with good measured OT and that this could explain their fainting tendency.
METHODS
Thirteen consecutive patients (aged 35 (4.7) years; six men) were studied who had PRS diagnosed on the basis of their clinical histories (two PRS episodes per week to one episode every three months) and positive responses to orthostatic stress testing. All were otherwise apparently healthy, were taking no drugs and provided informed written consent. The study was approved by the local research ethics committee and was performed in accordance with the Declaration of Helsinki.
OT was determined by combined head‐upright tilting and lower body suction as described previously.3 The test was performed exactly as in our earlier studies of postural sway in normal subjects.2 Test were terminated when systolic blood pressure fell to below 80 mm Hg and patients experienced presyncopal symptoms similar to their spontaneous events. OT was quantified as the time to termination of the test. Throughout testing we recorded beat‐to‐beat blood pressure, heart rate and forearm blood flow velocity.2
We determined postural sway as detailed previously.2 Patients were instructed to stand still on a force platform and foot position was standardised; there were no auditory or visual cues. We recorded both distance and velocity of movements in anteroposterior and mediolateral directions for 30 s periods after 1 and 5 min of standing.
Data were tested for normality and are expressed as mean (SEM). Data recorded after minutes 1 and 5 were compared by paired t tests. Published data from healthy control subjects with good and poor OT were compared with our results by one‐way analysis of variance with the Bonferroni adjustment for multiple comparisons. Significance was assumed when p < 0.05.
RESULTS
All patients with PRS had a shorter time to presyncope (OT) than that predicted.3 The mean OT was 13.4 (1.7) min. The maximum increase in vascular resistance during the orthostatic stress was small (59.2 (19.5)%) and this is consistent with previous data.1
The distances moved after 1 and 5 min standing were as follows: mediolateral 135.6 (13.5) mm and 130.4 (10.1) mm; and anteroposterior 146.6 (14.6) mm and 179.7 (16.9) mm, respectively. The corresponding velocities were mediolateral 4.5 (0.5) mm/s and 4.4 (0.3) mm/s; and anteroposterior 4.9 (0.5) mm/s and 6.0 (0.6) mm/s. The total distances moved after 1 and 5 min were 247.9 (19.4) mm and 271.4 (18.8) mm, and velocities were 8.3 (0.6) mm/s and 9.0 (0.6) mm/s. The distances and velocities of sway in the two planes were similar and did not change between 1 and 5 min. Further assessments were not possible, as some subjects developed presyncopal symptoms after 5 min.
DISCUSSION
This paper describes for the first time the postural sway profile of patients with PRS determined by established techniques. Postural sway, by compressing veins and enhancing return of blood, is an important mechanism in the maintenance of cardiac output and blood pressure when standing.4 Our hypothesis for undertaking this study was that, in people who may have less efficient cardiovascular control, an important difference between those who do not faint and those who do may be that fainters fail adequately to compensate by increased leg movements.
In our recent study of volunteer subjects who had never fainted and who had either good or poor OT to orthostatic stress testing,2 we noted that those with poor OT had enhanced postural sway during normal standing. We suggested that the greater movements in controls with poor OT would reduce venous pooling while standing, thereby compensating for their poor responses. However, during tilt testing, when movement was prevented, they could not make this compensation. The subjects with good OT had no need of this enhanced movement.
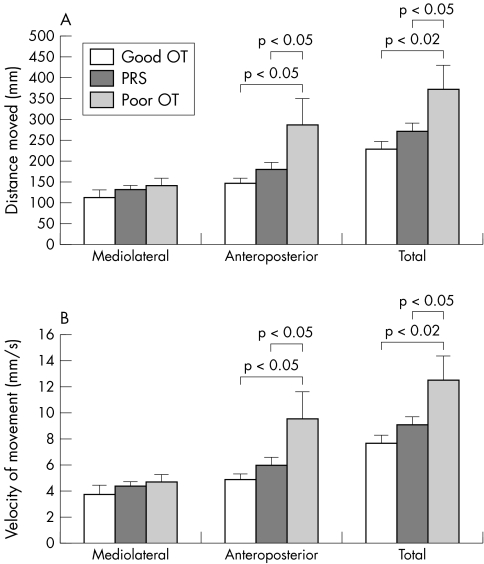
Both the patients in this study and the volunteers with poor measured OT in the earlier study had smaller forearm vasoconstrictor responses than those observed in healthy volunteers with good tolerance1,2 (table 1). This should render both patients with PRS and volunteers with poor OT susceptible to syncope. The measures of postural sway, however, were quite different (fig 1, table 1). Both the distance and velocity of movements associated with postural sway in the controls with poor OT increased during standing. In both the controls with good OT and the patients with PRS, however, there was little change. We suggest that a possible explanation for why patients with PRS faint, whereas the volunteers with similarly poor tolerance do not, may be that, for some reason, the patients have not learnt to compensate by increasing their postural movements.
Table 1 Characteristics and postural sway in patients with PRS compared with published data from control subjects with both good and poor OT.
| PRS | Good OT | Poor OT | |
|---|---|---|---|
| Number | 13 | 12 | 11 |
| Men:women | 6:7 | 6:6 | 5:6 |
| Age (years) | 35.0 (4.7) | 31.8 (3.9) | 26.9 (1.8) |
| OT (min) | 13.4 (1.7)*** | 36.7 (2.1) | 18.9 (1.8)*** |
| Max VR response (%) | 59.2 (19.5)* | 152.5 (23.9) | 95.3 (29.1) |
| Sway at minute 5 | |||
| Velocity (mm/s) | 9.0 (0.6) | 7.6 (0.6) | 12.5 (1.9)**† |
| Distance (mm) | 271.4 (18.8) | 228.8 (17.0) | 374.1 (55.1)**† |
| Increase in sway at minute 5 | |||
| Velocity (mm/s) | 1.24 (0.6) | 0.39 (0.3) | 3.0 (1.8) |
| Distance (mm) | 37.1 (17.8) | 11.8 (9.2) | 91.2 (53.0) |
Data are mean (SEM).
*p<0.05, **p<0.02, ***p<0.001 v good orthostatic tolerance (OT); †p<0.05 versus posturally related syncope (PRS).
Max VR, maximum vascular resistance.
Figure 1 (A) Distance moved and (B) velocity after 5 min of standing in patients with posturally related syncope (PRS) and control subjects with both good and poor orthostatic tolerance (OT). Controls with poor OT had greater distances and velocities of anteroposterior and total postural sway than patients with PRS and controls with good OT.
These results suggest that, in patients with uncomplicated PRS, a failure to compensate for poor reflex control of the circulation by enhanced postural sway may contribute to their predisposition to episodes of postural syncope. This probably explains the reason for the effectiveness of such procedures as leg crossing and muscle tensing.5 We advocate that patients with PRS be encouraged to increase their leg movements when standing to increase venous return and help prevent syncopal attacks.
ACKNOWLEDGEMENTS
We thank Professor Roger Soames for allowing us to use his biomechanical force measuring platform during this study.
Footnotes
This work did not receive financial support.
Competing interests: None declared.
References
- 1.Hainsworth R, Claydon V E. Syncope and fainting: classification and physiological basis. In: Bannister R, Mathias CJ, eds. Autonomic failure: a textbook of clinical disorders of the autonomic nervous system. Oxford: Oxford University Press, 2006
- 2.Claydon V E, Hainsworth R. Increased postural sway in control subjects with poor orthostatic tolerance. J Am Coll Cardiol 2005461309–1313. [DOI] [PubMed] [Google Scholar]
- 3.El‐Bedawi K M, Hainsworth R. Combined head up tilt and lower body suction: a test of orthostatic tolerance. Clin Auton Res 1994441–47. [DOI] [PubMed] [Google Scholar]
- 4.Guyton A C, Richardson T Q, Langston J B. Regulation of cardiac output and venous return. Clin Anesth 196431–34. [PubMed] [Google Scholar]
- 5.Krediet C T P, Van Dijk N, Linzer M.et al Management of vasovagal syncope: controlling or aborting faints by leg crossing and muscle tensing. Circulation 20021061684–1689. [DOI] [PubMed] [Google Scholar]