Abstract
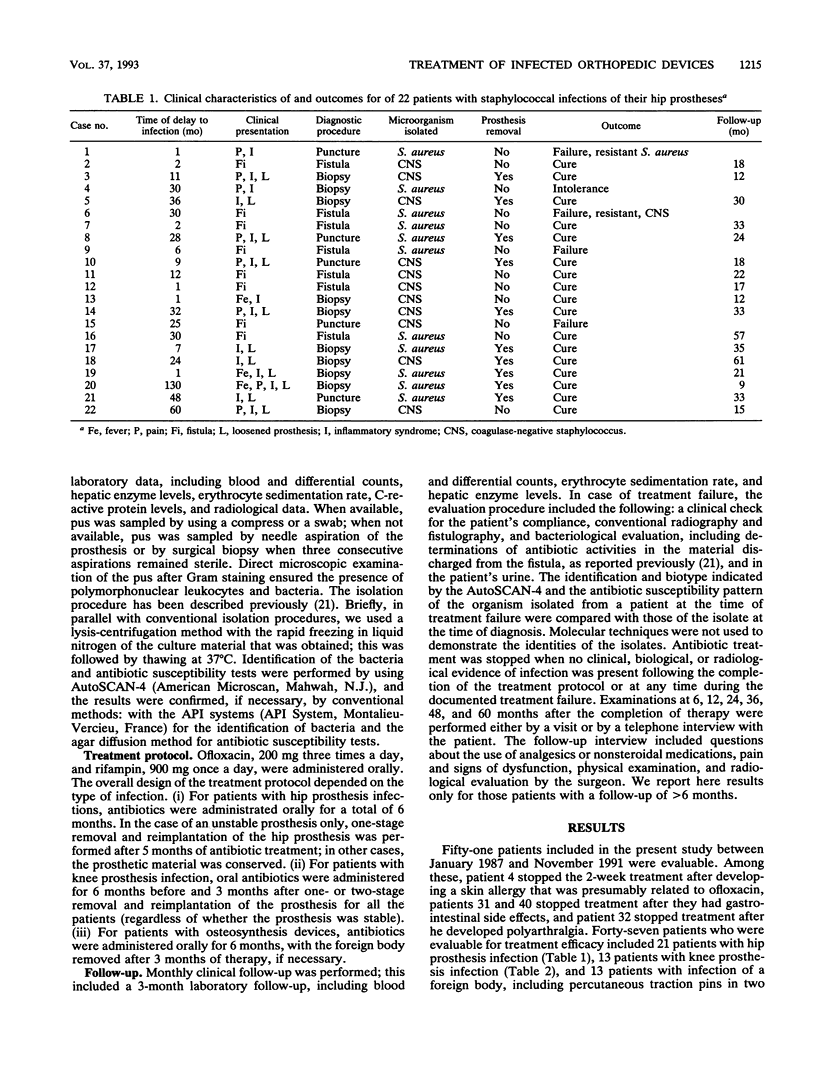
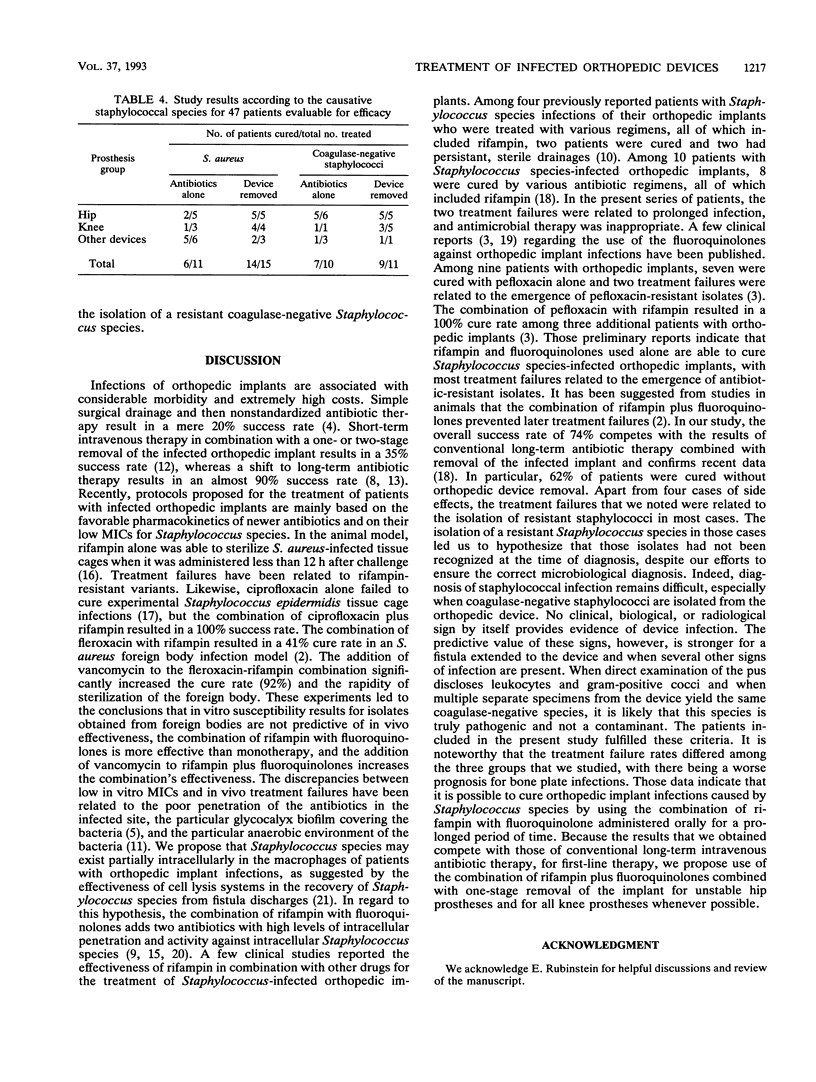
We examined the effectiveness and safety of the combination of rifampin plus ofloxacin given orally for treating prosthetic orthopedic implants infected with staphylococci. The prospective cohort study was conducted in a referral public hospital with ambulatory care services between 1985 and 1991. Consecutive patients from whom Staphylococcus organisms susceptible to the study drugs were isolated from their orthopedic implants and who had no contraindication to the treatment were eligible for the study. All patients were treated orally with rifampin, 900 mg/day, plus ofloxacin, 600 mg/day. Patients with hip prosthesis infection were treated for 6 months, with removal of any unstable prostheses after 5 months of treatment; patients with knee prosthesis infection were treated for 9 months, with removal of the prosthesis after 6 months of treatment; and patients with infected bone plates were treated for 6 months, with removal of the plate after 3 months of treatment, if necessary. Monthly clinical evaluations were conducted until the completion of the treatment and follow-up or telephone interviews were conducted at 6, 12, 24, 36, 48, and 60 months thereafter. Treatment failures were documented by clinical evaluation, sampling of the infected site for culture and antibiotic activity measurement, and fistulography, if possible. Cure was defined as the absence of clinical, biological, and radiological evidence of infection 6 months after the completion of treatment, treatment failure was defined as the absence of cure, and relapse was defined as the reappearance of infection caused by the same Staphylococcus isolate that caused the original infection, regardless of the timing of this secondary infection. Among 51 patients included in the study and evaluable for safety, 4 patients had side effects and were not evaluable for treatment effectiveness; the overall success rate was 74% among 47 patients, with a success rate of 81% for the hip prosthesis group, 69% for the knee prosthesis group, and 69% for the osteosynthesis device group. Eight treatment failures were relaxed to the isolation of a resistant bacterium. The combination of rifampin administered orally plus ofloxacin is a suitable alternative to the conventional long-term intravenous therapy for treatment of orthopedic implants infected with staphylococci.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Chuard C., Herrmann M., Vaudaux P., Waldvogel F. A., Lew D. P. Successful therapy of experimental chronic foreign-body infection due to methicillin-resistant Staphylococcus aureus by antimicrobial combinations. Antimicrob Agents Chemother. 1991 Dec;35(12):2611–2616. doi: 10.1128/aac.35.12.2611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Desplaces N., Acar J. F. New quinolones in the treatment of joint and bone infections. Rev Infect Dis. 1988 Jan-Feb;10 (Suppl 1):S179–S183. doi: 10.1093/clinids/10.supplement_1.s179. [DOI] [PubMed] [Google Scholar]
- Fitzgerald R. H., Jr, Nolan D. R., Ilstrup D. M., Van Scoy R. E., Washington J. A., 2nd, Coventry M. B. Deep wound sepsis following total hip arthroplasty. J Bone Joint Surg Am. 1977 Oct;59(7):847–855. [PubMed] [Google Scholar]
- Gristina A. G., Costerton J. W. Bacterial adherence to biomaterials and tissue. The significance of its role in clinical sepsis. J Bone Joint Surg Am. 1985 Feb;67(2):264–273. [PubMed] [Google Scholar]
- Grogan T. J., Dorey F., Rollins J., Amstutz H. C. Deep sepsis following total knee arthroplasty. Ten-year experience at the University of California at Los Angeles Medical Center. J Bone Joint Surg Am. 1986 Feb;68(2):226–234. [PubMed] [Google Scholar]
- Inman R. D., Gallegos K. V., Brause B. D., Redecha P. B., Christian C. L. Clinical and microbial features of prosthetic joint infection. Am J Med. 1984 Jul;77(1):47–53. doi: 10.1016/0002-9343(84)90434-0. [DOI] [PubMed] [Google Scholar]
- Insall J. N., Thompson F. M., Brause B. D. Two-stage reimplantation for the salvage of infected total knee arthroplasty. J Bone Joint Surg Am. 1983 Oct;65(8):1087–1098. [PubMed] [Google Scholar]
- Mandell G. L. The antimicrobial activity of rifampin: emphasis on the relation to phagocytes. Rev Infect Dis. 1983 Jul-Aug;5 (Suppl 3):S463–S467. doi: 10.1093/clinids/5.supplement_3.s463. [DOI] [PubMed] [Google Scholar]
- Norden C. W., Fierer J., Bryant R. E. Chronic staphylococcal osteomyelitis: treatment with regimens containing rifampin. Rev Infect Dis. 1983 Jul-Aug;5 (Suppl 3):S495–S501. doi: 10.1093/clinids/5.supplement_3.s495. [DOI] [PubMed] [Google Scholar]
- Norden C. W., Shaffer M. Treatment of experimental chronic osteomyelitis due to staphylococcus aureus with vancomycin and rifampin. J Infect Dis. 1983 Feb;147(2):352–357. doi: 10.1093/infdis/147.2.352. [DOI] [PubMed] [Google Scholar]
- Rand J. A., Bryan R. S. Reimplantation for the salvage of an infected total knee arthroplasty. J Bone Joint Surg Am. 1983 Oct;65(8):1081–1086. [PubMed] [Google Scholar]
- Salvati E. A., Robinson R. P., Zeno S. M., Koslin B. L., Brause B. D., Wilson P. D., Jr Infection rates after 3175 total hip and total knee replacements performed with and without a horizontal unidirectional filtered air-flow system. J Bone Joint Surg Am. 1982 Apr;64(4):525–535. [PubMed] [Google Scholar]
- Schutzer S. F., Harris W. H. Deep-wound infection after total hip replacement under contemporary aseptic conditions. J Bone Joint Surg Am. 1988 Jun;70(5):724–727. [PubMed] [Google Scholar]
- Solberg C. O., Halstensen A., Digranes A., Hellum K. B. Penetration of antibiotics into human leukocytes and dermal suction blisters. Rev Infect Dis. 1983 Jul-Aug;5 (Suppl 3):S468–S473. doi: 10.1093/clinids/5.supplement_3.s468. [DOI] [PubMed] [Google Scholar]
- Tshefu K., Zimmerli W., Waldvogel F. A. Short-term administration of rifampin in the prevention or eradication of infection due to foreign bodies. Rev Infect Dis. 1983 Jul-Aug;5 (Suppl 3):S474–S480. doi: 10.1093/clinids/5.supplement_3.s474. [DOI] [PubMed] [Google Scholar]
- Widmer A. F., Frei R., Rajacic Z., Zimmerli W. Correlation between in vivo and in vitro efficacy of antimicrobial agents against foreign body infections. J Infect Dis. 1990 Jul;162(1):96–102. doi: 10.1093/infdis/162.1.96. [DOI] [PubMed] [Google Scholar]
- Widmer A. F., Gaechter A., Ochsner P. E., Zimmerli W. Antimicrobial treatment of orthopedic implant-related infections with rifampin combinations. Clin Infect Dis. 1992 Jun;14(6):1251–1253. doi: 10.1093/clinids/14.6.1251. [DOI] [PubMed] [Google Scholar]
- Wispelwey B., Scheld W. M. Ciprofloxacin in the treatment of Staphylococcus aureus osteomyelitis. A review. Diagn Microbiol Infect Dis. 1990 Mar-Apr;13(2):169–171. doi: 10.1016/0732-8893(90)90103-3. [DOI] [PubMed] [Google Scholar]
- Yancey R. J., Sanchez M. S., Ford C. W. Activity of antibiotics against Staphylococcus aureus within polymorphonuclear neutrophils. Eur J Clin Microbiol Infect Dis. 1991 Feb;10(2):107–113. doi: 10.1007/BF01964421. [DOI] [PubMed] [Google Scholar]
- Zannier A., Drancourt M., Franceschi J. P., Aubaniac J. M., Raoult D. Intérêt d'une technique de lyse cellulaire par choc thermique dans l'isolement de bactéries responsables d'infections ostéo-articulaires. Pathol Biol (Paris) 1991 May;39(5):543–546. [PubMed] [Google Scholar]


