Abstract
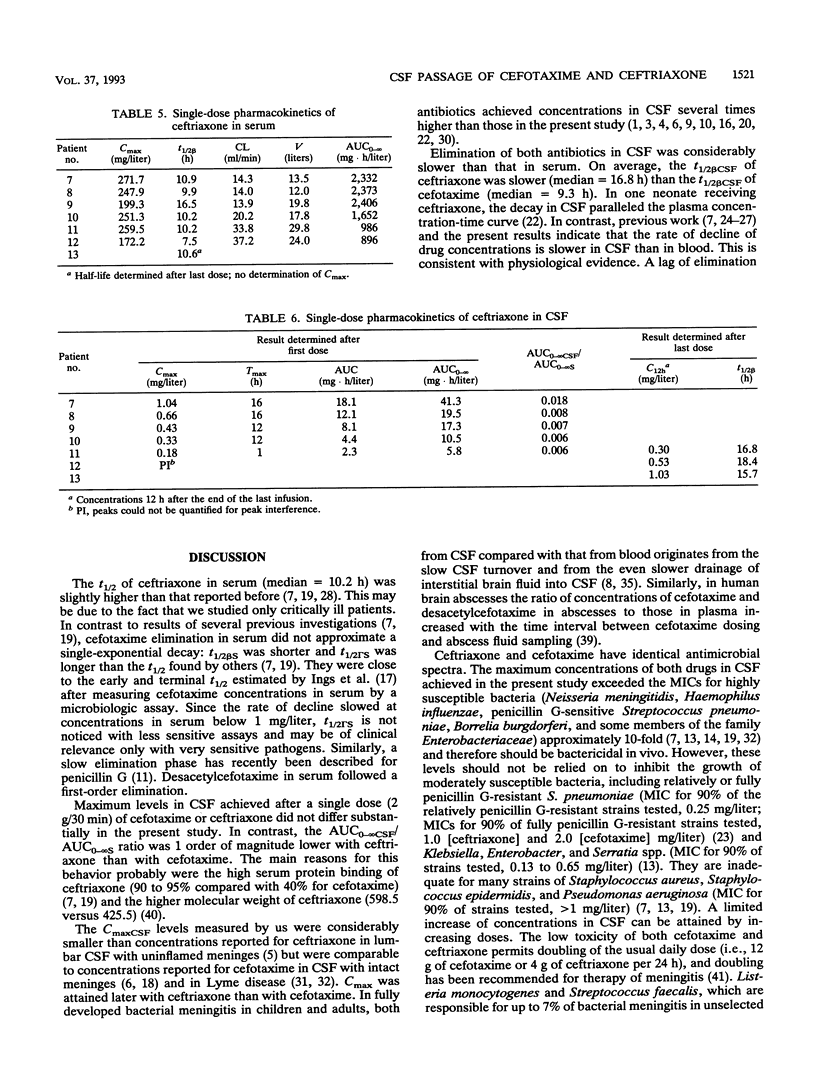
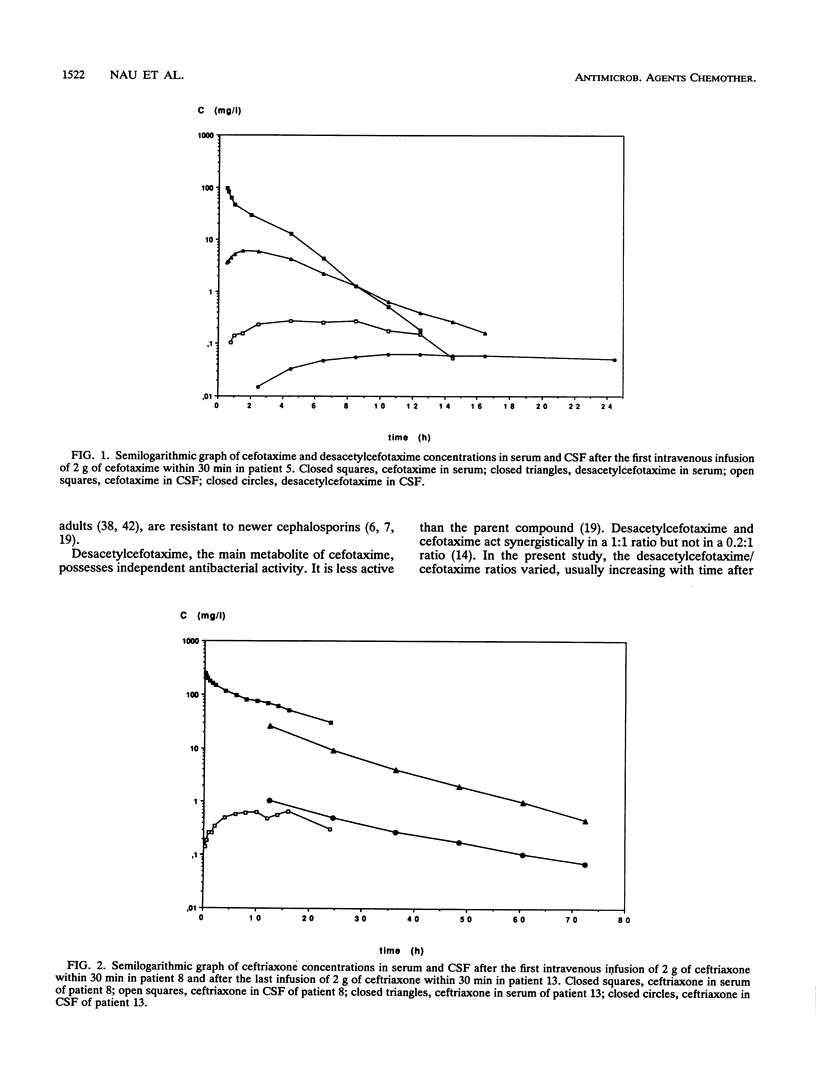
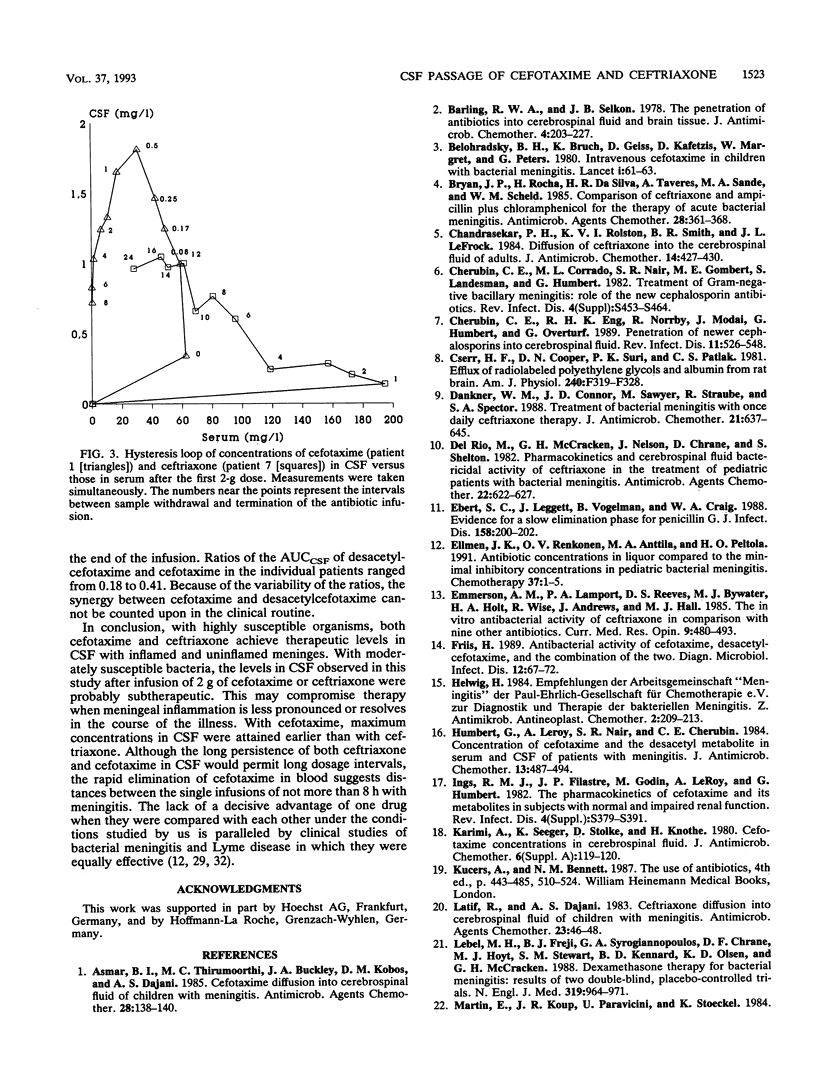
Cefotaxime and ceftriaxone have proven to be effective in pyogenic infections of the central nervous system. Since in some bacterial central nervous system infections the blood-cerebrospinal fluid (CSF) barrier is either minimally impaired or recovers in the course of the illness, we studied the penetration of both antibiotics in the absence of inflamed meninges. Patients who had undergone external ventriculostomies for noninflammatory occlusive hydrocephalus received either cefotaxime (2 g/30 min) or ceftriaxone (2 g/30 min) to treat extracerebral infections. Serum and CSF were drawn repeatedly after the first dose. With ceftriaxone, they were also drawn after the last dose. The concentrations of cefotaxime, its metabolite desacetylcefotaxime, and ceftriaxone were determined by high-performance liquid chromatography with UV detection. Maximum concentrations of cefotaxime in CSF were reached 0.5 to 8 h (median = 3 h; n = 6) after the end of the infusion and ranged from 0.14 to 1.81 mg/liter (median = 0.44 mg/liter; n = 6). Maximum levels of ceftriaxone in CSF ranging from 0.18 to 1.04 mg/liter (median = 0.43 mg/liter; n = 5) were seen 1 to 16 h (median = 12 h; n = 5) after the infusion. The elimination half-life of cefotaxime in CSF was 5.0 to 26.9 h (median = 9.3 h; n = 5), and that of ceftriaxone was 15.7 to 18.4 h (median = 16.8 h; n = 3). It is concluded that after a single dose of 2 g, maximal concentrations of cefotaxime and ceftriaxone in CSF do not differ substantially. The long elimination half-lives guarantee uniform concentrations in CSF. These concentrations reliably inhibit highly susceptible bacteria but cannot be relied on to inhibit staphylococci and penicillin G-resistant Streptococcus pneumoniae.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Asmar B. I., Thirumoorthi M. C., Buckley J. A., Kobos D. M., Dajani A. S. Cefotaxime diffusion into cerebrospinal fluid of children with meningitis. Antimicrob Agents Chemother. 1985 Jul;28(1):138–140. doi: 10.1128/aac.28.1.138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barling R. W., Selkon J. B. The penetration of antibiotics into cerebrospinal fluid and brain tissue. J Antimicrob Chemother. 1978 May;4(3):203–227. doi: 10.1093/jac/4.3.203. [DOI] [PubMed] [Google Scholar]
- Belohradsky B. H., Bruch K., Geiss D., Kafetzis D., Marget W., Peters G. Intravenous cefotaxime in children with bacterial meningitis. Lancet. 1980 Jan 12;1(8159):61–63. doi: 10.1016/s0140-6736(80)90491-2. [DOI] [PubMed] [Google Scholar]
- Bryan J. P., Rocha H., da Silva H. R., Taveres A., Sande M. A., Scheld W. M. Comparison of ceftriaxone and ampicillin plus chloramphenicol for the therapy of acute bacterial meningitis. Antimicrob Agents Chemother. 1985 Sep;28(3):361–368. doi: 10.1128/aac.28.3.361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chandrasekar P. H., Rolston K. V., Smith B. R., LeFrock J. L. Diffusion of ceftriaxone into the cerebrospinal fluid of adults. J Antimicrob Chemother. 1984 Oct;14(4):427–430. doi: 10.1093/jac/14.4.427. [DOI] [PubMed] [Google Scholar]
- Cherubin C. E., Corrado M. L., Nair S. R., Gombert M. E., Landesman S., Humbert G. Treatment of gram-negative bacillary meningitis: role of the new cephalosporin antibiotics. Rev Infect Dis. 1982 Sep-Oct;4 (Suppl):S453–S464. doi: 10.1093/clinids/4.supplement_2.s453. [DOI] [PubMed] [Google Scholar]
- Cherubin C. E., Eng R. H., Norrby R., Modai J., Humbert G., Overturf G. Penetration of newer cephalosporins into cerebrospinal fluid. Rev Infect Dis. 1989 Jul-Aug;11(4):526–548. doi: 10.1093/clinids/11.4.526. [DOI] [PubMed] [Google Scholar]
- Cserr H. F., Cooper D. N., Suri P. K., Patlak C. S. Efflux of radiolabeled polyethylene glycols and albumin from rat brain. Am J Physiol. 1981 Apr;240(4):F319–F328. doi: 10.1152/ajprenal.1981.240.4.F319. [DOI] [PubMed] [Google Scholar]
- Dankner W. M., Connor J. D., Sawyer M., Straube R., Spector S. A. Treatment of bacterial meningitis with once daily ceftriaxone therapy. J Antimicrob Chemother. 1988 May;21(5):637–645. doi: 10.1093/jac/21.5.637. [DOI] [PubMed] [Google Scholar]
- Del Rio M., McCracken G. H., Jr, Nelson J. D., Chrane D., Shelton S. Pharmacokinetics and cerebrospinal fluid bactericidal activity of ceftriaxone in the treatment of pediatric patients with bacterial meningitis. Antimicrob Agents Chemother. 1982 Oct;22(4):622–627. doi: 10.1128/aac.22.4.622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ebert S. C., Leggett J., Vogelman B., Craig W. A. Evidence for a slow elimination phase for penicillin G. J Infect Dis. 1988 Jul;158(1):200–202. doi: 10.1093/infdis/158.1.200. [DOI] [PubMed] [Google Scholar]
- Ellmén J. K., Renkonen O. V., Anttila M. A., Peltola H. O. Antibiotic concentrations in liquor compared to the minimal inhibitory concentrations of isolates in paediatric bacterial meningitis. The Finnish Study Group. Chemotherapy. 1991;37(1):1–5. doi: 10.1159/000238825. [DOI] [PubMed] [Google Scholar]
- Emmerson A. M., Lamport P. A., Reeves D. S., Bywater M. J., Holt H. A., Wise R., Andrews J., Hall M. J. The in vitro antibacterial activity of ceftriaxone in comparison with nine other antibiotics. Curr Med Res Opin. 1985;9(7):480–493. doi: 10.1185/03007998509109622. [DOI] [PubMed] [Google Scholar]
- Friis H. Antibacterial activity of cefotaxime, desacetylcefotaxime, and the combination of the two. Diagn Microbiol Infect Dis. 1989 Jan-Feb;12(1):67–72. doi: 10.1016/0732-8893(89)90048-5. [DOI] [PubMed] [Google Scholar]
- Humbert G., Leroy A., Nair S. R., Cherubin C. E. Concentrations of cefotaxime and the desacetyl metabolite in serum and CSF of patients with meningitis. J Antimicrob Chemother. 1984 May;13(5):487–494. doi: 10.1093/jac/13.5.487. [DOI] [PubMed] [Google Scholar]
- Ings R. M., Fillastre J. P., Godin M., Leroy A., Humbert G. The pharmacokinetics of cefotaxime and its metabolites in subjects with normal and impaired renal function. Rev Infect Dis. 1982 Sep-Oct;4 (Suppl):S379–S391. doi: 10.1093/clinids/4.supplement_2.s379. [DOI] [PubMed] [Google Scholar]
- Karimi A., Seeger K., Stolke D., Knothe H. Cefotaxime concentration in cerebrospinal fluid. J Antimicrob Chemother. 1980 Sep;6 (Suppl A):119–120. doi: 10.1093/jac/6.suppl_a.119. [DOI] [PubMed] [Google Scholar]
- Latif R., Dajani A. S. Ceftriaxone diffusion into cerebrospinal fluid of children with meningitis. Antimicrob Agents Chemother. 1983 Jan;23(1):46–48. doi: 10.1128/aac.23.1.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lebel M. H., Freij B. J., Syrogiannopoulos G. A., Chrane D. F., Hoyt M. J., Stewart S. M., Kennard B. D., Olsen K. D., McCracken G. H., Jr Dexamethasone therapy for bacterial meningitis. Results of two double-blind, placebo-controlled trials. N Engl J Med. 1988 Oct 13;319(15):964–971. doi: 10.1056/NEJM198810133191502. [DOI] [PubMed] [Google Scholar]
- Marton A., Gulyas M., Munoz R., Tomasz A. Extremely high incidence of antibiotic resistance in clinical isolates of Streptococcus pneumoniae in Hungary. J Infect Dis. 1991 Mar;163(3):542–548. doi: 10.1093/infdis/163.3.542. [DOI] [PubMed] [Google Scholar]
- Nau R., Dreyhaupt T., Kolenda H., Prange H. W. Low blood-to-cerebrospinal fluid passage of sorbitol after intravenous infusion. Stroke. 1992 Sep;23(9):1276–1279. doi: 10.1161/01.str.23.9.1276. [DOI] [PubMed] [Google Scholar]
- Nau R., Prange H. W., Martell J., Sharifi S., Kolenda H., Bircher J. Penetration of ciprofloxacin into the cerebrospinal fluid of patients with uninflamed meninges. J Antimicrob Chemother. 1990 Jun;25(6):965–973. doi: 10.1093/jac/25.6.965. [DOI] [PubMed] [Google Scholar]
- Nau R., Prange H. W., Menck S., Kolenda H., Visser K., Seydel J. K. Penetration of rifampicin into the cerebrospinal fluid of adults with uninflamed meninges. J Antimicrob Chemother. 1992 Jun;29(6):719–724. doi: 10.1093/jac/29.6.719. [DOI] [PubMed] [Google Scholar]
- Nau R., Prins F. J., Kolenda H., Prange H. W. Temporary reversal of serum to cerebrospinal fluid glycerol concentration gradient after intravenous infusion of glycerol. Eur J Clin Pharmacol. 1992;42(2):181–185. doi: 10.1007/BF00278481. [DOI] [PubMed] [Google Scholar]
- Patel I. H., Chen S., Parsonnet M., Hackman M. R., Brooks M. A., Konikoff J., Kaplan S. A. Pharmacokinetics of ceftriaxone in humans. Antimicrob Agents Chemother. 1981 Nov;20(5):634–641. doi: 10.1128/aac.20.5.634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peltola H., Anttila M., Renkonen O. V. Randomised comparison of chloramphenicol, ampicillin, cefotaxime, and ceftriaxone for childhood bacterial meningitis. Finnish Study Group. Lancet. 1989 Jun 10;1(8650):1281–1287. doi: 10.1016/s0140-6736(89)92685-8. [DOI] [PubMed] [Google Scholar]
- Peretti P., Sueri L., Tosi M., Ciammarughi R., Cadeo G. P., Milanesi B. Cefotaxime in the cerebrospinal fluid and serum in patients with purulent meningitis. J Antimicrob Chemother. 1984 Sep;14 (Suppl B):117–123. doi: 10.1093/jac/14.suppl_b.117. [DOI] [PubMed] [Google Scholar]
- Pfister H. W., Preac-Mursic V., Wilske B., Einhäupl K. M. Cefotaxime vs penicillin G for acute neurologic manifestations in Lyme borreliosis. A prospective randomized study. Arch Neurol. 1989 Nov;46(11):1190–1194. doi: 10.1001/archneur.1989.00520470044025. [DOI] [PubMed] [Google Scholar]
- Pfister H. W., Preac-Mursic V., Wilske B., Schielke E., Sörgel F., Einhäupl K. M. Randomized comparison of ceftriaxone and cefotaxime in Lyme neuroborreliosis. J Infect Dis. 1991 Feb;163(2):311–318. doi: 10.1093/infdis/163.2.311. [DOI] [PubMed] [Google Scholar]
- Reiber H., Felgenhauer K. Protein transfer at the blood cerebrospinal fluid barrier and the quantitation of the humoral immune response within the central nervous system. Clin Chim Acta. 1987 Mar 30;163(3):319–328. doi: 10.1016/0009-8981(87)90250-6. [DOI] [PubMed] [Google Scholar]
- Schaad U. B., Suter S., Gianella-Borradori A., Pfenninger J., Auckenthaler R., Bernath O., Cheseaux J. J., Wedgwood J. A comparison of ceftriaxone and cefuroxime for the treatment of bacterial meningitis in children. N Engl J Med. 1990 Jan 18;322(3):141–147. doi: 10.1056/NEJM199001183220301. [DOI] [PubMed] [Google Scholar]
- Schlech W. F., 3rd, Ward J. I., Band J. D., Hightower A., Fraser D. W., Broome C. V. Bacterial meningitis in the United States, 1978 through 1981. The National Bacterial Meningitis Surveillance Study. JAMA. 1985 Mar 22;253(12):1749–1754. [PubMed] [Google Scholar]
- Sjölin J., Eriksson N., Arneborn P., Cars O. Penetration of cefotaxime and desacetylcefotaxime into brain abscesses in humans. Antimicrob Agents Chemother. 1991 Dec;35(12):2606–2610. doi: 10.1128/aac.35.12.2606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thea D., Barza M. Use of antibacterial agents in infections of the central nervous system. Infect Dis Clin North Am. 1989 Sep;3(3):553–570. [PubMed] [Google Scholar]
- Tunkel A. R., Wispelwey B., Scheld W. M. Bacterial meningitis: recent advances in pathophysiology and treatment. Ann Intern Med. 1990 Apr 15;112(8):610–623. doi: 10.7326/0003-4819-112-8-610. [DOI] [PubMed] [Google Scholar]


